Abstract
Background
The prognosis for marginally resectable gastric cancer with extensive lymph node metastasis (ELM) remains unfavorable, even after R0 resection. To assess the safety and efficacy of preoperative docetaxel, oxaliplatin, and S-1 (DOS), we conducted a multicenter phase II trial.
Methods
Eligibility criteria included histologically proven HER2-negative gastric adenocarcinoma with bulky nodal (bulky N) involvement around major branched arteries or para-aortic node (PAN) metastases. Patients received three cycles of docetaxel (40 mg/m2, day 1), oxaliplatin (100 mg/m2, day 1), and S-1 (80–120 mg/body, days 1–14), followed by gastrectomy with D2 plus PAN dissection. Subsequently, patients underwent postoperative chemotherapy with S-1 for 1 year. The primary endpoint was major (grade ≥ 2a) pathological response rate (pRR) according to the Japanese Classification of Gastric Carcinoma criteria.
Results
Between October 2018 and March 2022, 47 patients (bulky N, 20; PAN, 17; both, 10) were enrolled in the trial. One patient was ineligible. Another declined any protocol treatments before initiation. Among the 45 eligible patients who initiated DOS chemotherapy, 44 (98%) completed 3 cycles and 42 (93%) underwent R0 resection. Major pRR and pathological complete response rates among the 46 eligible patients, including the patient who declined treatment, were 57% (26/46) and 24% (11/46), respectively. Common grade 3 or 4 toxicities were neutropenia (24%), anorexia (16%), febrile neutropenia (9%), and diarrhea (9%). No treatment-related deaths occurred.
Conclusions
Preoperative chemotherapy with DOS yielded favorable pathological responses with an acceptable toxicity profile. This multimodal approach is highly promising for treating gastric cancer with ELM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is the fourth leading cause of cancer deaths worldwide [1]. The only curative treatment for gastric cancer is surgical resection [2,3,4]. Patients with gastric cancer sometimes have para-aortic lymph node metastases or bulky lymph node metastases located along the main arteries such as the celiac, splenic, common, or proper hepatic arteries. The prognosis of patients with gastric cancer who have such extensive lymph node metastasis (ELM) is extremely poor, even after R0 resection. To improve the outcomes of patients with marginally resectable disease, the Stomach Cancer Study Group of the Japan Clinical Oncology Group (SCSG/JCOG) conducted three phase II trials (JCOG0001, JCOG0405, and JCOG1002) of preoperative chemotherapy with or without postoperative chemotherapy after 2000 [5,6,7]. Based on the results of these three trials, the current Japanese Gastric Cancer Treatment Guidelines state that a preoperative doublet regimen of cisplatin plus S-1 (CS) for two cycles followed by extended surgery and postoperative S-1 for eight cycles is the standard treatment for gastric cancer with ELM [8].
However, in the West, perioperative chemotherapy with fluorouracil, leucovorin, oxaliplatin, and docetaxel (FLOT) is the standard treatment for resectable gastric cancer (except for cT1N0) according to the results of a German phase III trial (FLOT4) [9]. In addition, a preoperative triplet regimen of docetaxel, oxaliplatin, and S-1 (DOS) for three cycles followed by postoperative S-1 for eight cycles resulted in a significant improvement in progression-free survival (PFS) and overall survival (OS) compared with postoperative S-1 for eight cycles after upfront surgery for cT2-3N1 or cT4 gastric cancer in a Korean phase III trial (PRODIGY) [10, 11]. An Osaka University research group modified the dose of docetaxel from 50 to 40 mg/m2 due to concerns about neutropenia [12]. They reported sufficient antitumor effects and tolerable safety in a phase II trial of preoperative DOS for cStage III gastric or esophagogastric junction adenocarcinoma [13]. Based on these findings, the SCSG/JCOG initiated a new phase II trial (JCOG1704) to evaluate the safety and efficacy of preoperative DOS for gastric cancer with ELM.
Patients and methods
Patients
JCOG1704 was a multicenter phase II trial involving 22 institutions within the SCSG/JCOG. The eligibility and exclusion criteria for this trial were previously reported [14]. Briefly, histologically proven HER2-negative gastric adenocarcinoma with lymph node metastasis (larger than 1 cm based on enhanced computed tomography (CT)) in para-aortic node (PAN) stations (no. 16a2 or 16b1) or bulky lymph node (bulky N) metastasis (one lymph node larger than 3 cm or two lymph nodes larger than 1.5 cm based on enhanced CT) in stations no. 7, 8a, 9, 11, 12a, or 14v was eligible. Conversely, patients with distant metastasis except in lymph node stations no. 16a2 or 16b1, esophageal invasion of more than 3 cm, or remnant gastric cancer were ineligible. Macroscopic (Borrmann) type 4 or large (≥ 8 cm) type 3 tumors were excluded from the eligibility criteria of this trial, because they usually exhibit peritoneal metastases even after R0 resection. Other patient eligibility criteria included: age from 20 to 75 years, ECOG performance status of 0 or 1, sufficient oral intake with or without bypass surgery, and appropriate organ function (neutrophil count ≥ 2000/mm3, hemoglobin ≥ 8.0 g/dL, platelet count ≥ 100,000/mm3, serum total bilirubin ≤ 1.5 mg/dL, serum aspartate aminotransferase (AST) ≤ 100 IU/L, serum alanine aminotransferase (ALT) ≤ 100 IU/L, and creatinine clearance (CCr) ≥ 50 mL/min). Patients with a history of gastric cancer surgery except for bypass surgery or endoscopic resection or a history of chemotherapy or radiation therapy for other malignancies were excluded.
Staging laparoscopy or laparotomy before enrollment was mandatory to confirm the absence of peritoneal metastasis (P0) and negative cytology in peritoneal lavage fluid (CY0). All patients provided written informed consent. The JCOG Protocol Review Committee and the Certified Review Board of the National Cancer Center Hospital approved this trial protocol, which was registered in the Japan Registry of Clinical Trials (jRCTs031180028).
Preoperative chemotherapy
Within 2 weeks after enrollment, patients received preoperative chemotherapy consisting of intravenous docetaxel (40 mg/m2) and oxaliplatin (100 mg/m2) on day 1 and oral S-1 (80 mg/m2/day adjusted based on body surface area (< 1.25 m2, 80 mg/day; 1.25–1.5 m2, 100 mg/day; and > 1.5 m2, 120 mg/day) on days 1–14, in a 3-week cycle. This treatment cycle was repeated three times based on the PRODIGY trial, unless clear disease progression or unacceptable toxicity was observed. Tumor response was assessed after cycles 1 and 3 of preoperative chemotherapy using enhanced abdominal CT. The specific criteria for dose reduction and suspension of S-1 administration were previously documented [14].
Surgery
Within 4 (recommended) to 8 weeks after the last administration of S-1, we performed surgery on patients who were amenable to R0 resection based on enhanced abdominal and chest CT findings and had satisfactory organ function as indicated by blood tests conducted within 2 weeks before surgery. In this trial, it was mandatory for each patient to undergo either distal or total gastrectomy with D2 dissection in addition to the complete PAN dissection of stations no. 16a2 and 16b1, as previously described [15]. PAN dissection. The spleen was preserved unless the tumor involved the greater curvature of the upper stomach or there was suspected metastasis in the splenic hilar node (no. 10). Any neighboring organ(s) invaded by the tumor were removed to ensure R0 resection. The method of reconstruction was not prespecified. Laparoscopic gastrectomy and complete bursectomy were not permitted. If laparotomy revealed unresectable metastases, including positive cytology in peritoneal lavage fluid (CY1), the protocol treatment was terminated at that point.
Postoperative chemotherapy
Within 6 weeks after achieving R0 resection, patients began receiving postoperative chemotherapy consisting of S-1 (80 mg/m2/day) on days 1–28, repeated every 6 weeks until 1 year after surgery, unless the pathological response to preoperative DOS chemotherapy was graded as 0 (no evident treatment effect) on the basis of the Japanese Classification of Gastric Carcinoma (JCGC) criteria. If postoperative S-1 administration could not start within 12 weeks after surgery due to any reason, the protocol treatment was terminated at that point.
Patients were subject to a fixed follow-up schedule for at least 5 years after surgery. Blood tests measuring CEA and CA19-9 were repeated every 3 months during the initial 3 years and then every 6 months for the subsequent 2 years. Enhanced abdominal CT was performed every 6 months for the first 3 years and annually for the following 2 years. Chest X-ray and upper esophagogastroduodenoscopy (except after total gastrectomy) were carried out annually.
Outcomes
Pathological response was assessed based on both the JCGC and Becker regression criteria [16, 17]. In brief, JCGC grade 3 indicates the absence of viable tumor cells, grade 2b indicates viable tumor cells in less than 1/10 of the tumor area, grade 2a indicates viable tumor cells in 1/10 to 1/3 of the tumor area, and grade 1b indicates viable tumor cells in 1/3 to 2/3 of the tumor area. According to the Becker regression criteria of tumor regression grade (TRG), grade 1a indicates the absence of residual tumor cells, grade 1b indicates less than 10% residual tumor cells, and grade 2 indicates 10–50% residual tumor cells.
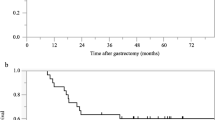
The primary endpoint for this trial was the major pathological response rate (pRR), defined as JCGC grade 3, 2b, or 2a. The secondary endpoints included OS, relapse-free survival for patients undergoing R0 resection, proportion of patients with R0 resection, preoperative chemotherapy response rate according to RECIST, version 1.0, proportion of patients completing both preoperative chemotherapy and protocol-specified surgery, proportion of patients completing all protocol-directed treatments, and adverse events. Adverse events were assessed based on the Common Terminology Criteria for Adverse Events (CTCAE), version 4.0. The Clavien–Dindo classification was used to evaluate postoperative morbidities [18, 19]. Clinical and pathological staging was evaluated according to the 15th edition of the JCGC.
Statistical analysis
In the previous JCOG0405 trial with the identical patient eligibility criteria, major pRR was 27%. Employing a SWOG two-stage study design [20], with 80% statistical power for an anticipated major pRR of 40% with a threshold of 25% and one-sided alpha of 10%, the projected sample size was determined to be 45. Therefore, we planned to enroll 50 patients, accounting for 5 potentially ineligible participants. If 5 or more patients among the initial 25 patients had a major pathological response during the first stage, an additional 25 patients would be enrolled for the second stage. At the second-stage analysis for all patients, preoperative DOS chemotherapy would be considered a promising regimen if the preset threshold value of 25% was rejected with a one-sided alpha of 10%. In other words, if 17 or more of 50 patients had a major pathological response, preoperative DOS chemotherapy would be considered a promising regimen. The confidence interval for pRR was estimated using Clopper-Pearson method. All analyses were conducted based on the intention-to-treat principle using SAS® version 9.4 or higher (SAS Institute, Cary, NC, USA).
Results
Between December 2018 and March 2022, a total of 47 patients (20 with bulky N, 17 with PAN, and 10 with both) were enrolled in this trial (Fig. 1). Among these patients, one was ineligible due to a special histological type (adenocarcinoma with enteroblastic differentiation). The baseline characteristics of the 47 patients are shown in Table 1. However, one eligible patient declined any protocol treatments before initiation. Among the 45 eligible patients who initiated DOS chemotherapy, 44 patients (98%) completed 3 cycles, whereas 1 patient discontinued after 1 cycle due to a grade 3 thromboembolic event. The relative dose intensity was 94.9% for docetaxel, 94.2% for oxaliplatin, and 87.7% for S-1. Adverse events experienced during preoperative DOS chemotherapy among the 45 eligible patients who initiated DOS are detailed in Table 2. Notably, grade 3 or 4 toxicities attributed to DOS included neutropenia in 11 patients (24%), anorexia in 7 (16%), febrile neutropenia in 4 (9%), and diarrhea in 4 (9%). There were no treatment-related deaths.
Among the 45 eligible patients who initiated DOS chemotherapy, 43 (96%) underwent surgery after chemotherapy and 42 (93%) underwent R0 resection. One patient underwent R1 resection due to positive cytology (CY1). Two patients were not amenable to R0 resection on the basis of a preoperative assessment. The pathological findings in the resected specimens are summarized in Table 3. Postoperative complications (Clavien–Dindo grade III or higher) were pancreatic fistula in two patients (5%), abdominal abscess in one (2%), anastomotic leakage in one (2%), and pleural effusion in one (2%). There were no in-hospital deaths.
Responses to preoperative chemotherapy based on RECIST, version 1.0 were partial response (PR) in 30 patients, stable disease (SD) in 12, and progressive disease (PD) in 2, resulting in a response rate of 65% (30/46) among all eligible patients. Pathological responses of the primary tumor among the 43 eligible patients who underwent surgical resection are outlined in Table 4. Briefly, major (JCGC grade ≥ 2a) pRR and pathological complete response (pCR) were attained in 26 (60%) and 11 (26%) patients, respectively. Regarding JCGC grade 3 cases, there was a trend toward a higher prevalence (45%) of cases located in the upper third of the stomach (Supplementary Table S1). Concerning JCGC grade 1a cases, we observed a trend toward a higher proportion (69%) of cases with bulky N only and a lower proportion (15%) of cases with PAN only (Supplementary Table S2). Among 46 eligible patients, including 1 patient who declined any protocol treatments, major pRR was 57% (80% CI, 46–67%; 95% CI, 41.1–71.1%), with a statistical significance against the threshold of 25% (p < 0.0001). Patients with differentiated histological types had a major pRR of 61% (20/33), while patients with undifferentiated types had a rate of 46% (6/13) (p = 0.51). Furthermore, neither tumor location nor node status (bulky N, PAN, or both) significantly affected major pRR (p = 0.43 and p = 0.43, respectively). When evaluating pathological responses according to the Becker criteria, major (TRG 1a or 1b) and minor (TRG 1a, 1b, or 2) pRR were 39% (18/46) and 65% (30/46), respectively. Pathological responses across JCOG phase II trials targeting gastric cancer with ELM are summarized in Table 5.
Discussion
In this multicenter phase II trial, preoperative DOS chemotherapy for marginally resectable gastric cancer with ELM exhibited much greater efficacy than initially anticipated. Along with the proportion of patients with R0 resection exceeding 90% within this patient population with highly advanced disease, the substantial pathological impact of DOS chemotherapy, with major pRR of 57% and pCR rate of 24%, was particularly notable. The chemotherapy regimen could be safely managed while maintaining high relative dose intensities for all three drugs. Importantly, no treatment-related deaths were observed during preoperative chemotherapy or after extended surgery involving PAN dissection. This outcome provides robust support for the use of this multimodal treatment approach for this category of gastric cancer, even in the absence of subsequent confirmation via phase III trials. In addition, it is worth noting that the DOS regimen could potentially expand the eligibility for conversion surgery in cStage IV patients with other types of distant metastasis, leading to improved long-term outcomes.
In the context of marginally resectable gastric cancer with ELM, JCOG has consistently conducted phase II trials to find the most promising preoperative chemotherapy regimens while adhering to the same eligibility criteria. In the initial JCOG0001 trial, preoperative chemotherapy consisting of irinotecan plus cisplatin was hampered by significant toxicity, evidenced by a mortality rate of 5.5% [5]. Nonetheless, minor (JCGC grade ≥ 1b) pRR was only 15%. The subsequent JCOG0405 trial achieved the establishment of a tentative standard treatment for this category of gastric cancer. Preoperative chemotherapy with CS yielded higher pRRs (minor, 51%; major, 27%) and a 3-year OS rate of 59% without any mortality [6]. However, the subsequent JCOG1002 trial of a triplet regimen consisting of docetaxel plus CS (DCS) did not yield better results than JCOG0405 [7]. The failure of DCS might be attributed to the lower dose intensity of S-1 (280 mg/m2/week) and docetaxel (10 mg/m2/week). By contrast, the DOS regimen in this JCOG1704 trial incorporated higher dose intensities of S-1 (373 mg/m2/week) and docetaxel (13 mg/m2/week) than in JCOG1002. The substitution of oxaliplatin for cisplatin might have contributed to increased efficacy [21]. Notably, the DOS triplet regimen yielded major pRR at least 30% higher and pCR rate at least 20% higher than CS in JCOG0405.
In the West, FLOT has been the standard perioperative chemotherapy regimen for resectable gastric cancer [9]. In the phase II FLOT4 trial, preoperative FLOT chemotherapy yielded major (TRG 1a or 1b) and minor (TRG 1a, 1b, or 2) pRRs of 32% (47/148) and 47% (70/148), respectively, with pCR rate of 14% (20/148) [22]. These pathological response rates for FLOT were comparatively lower than those for DOS in JCOG1704, even though FLOT4 involved patients with earlier-stage gastric cancer. We believe that the robust efficacy of DOS is potentially attributed to the effect of S-1, considering the lower dose intensity of docetaxel and oxaliplatin in DOS compared with that in FLOT. The recent Korean phase III PRODIGY trial demonstrated that preoperative DOS improves both PFS and OS in cStage II–III gastric cancer compared with postoperative S-1 alone [10, 11]. The antitumor activity of S-1 in contrast to 5-fluorouracil in the FLOT regimen might explain the superior pathological efficacy [23]. In this JCOG1704 trial, the dose of docetaxel on day 1 (40 mg/m2) was slightly lower than that (50 mg/m2) in the PRODIGY trial, on the basis of a prior Japanese phase II trial [13]. This mild dose reduction might have contributed to the favorable compliance rate without compromising efficacy in this trial. However, it is worth noting the relatively elevated incidences of grade 3 or 4 neutropenia, anorexia, diarrhea, and febrile neutropenia. Thus, careful management of adverse events during DOS chemotherapy is necessary.
The primary endpoint of the JCOG1704 trial was major pRR, which diverged from the primary endpoints of previous JCOG trials targeting the same patient population. When recent analyses were conducted using data from previous JCOG trials of preoperative chemotherapy for marginally resectable gastric cancer, pRR was a superior surrogate indicator for survival when compared to response rate based on RECIST [24]. Furthermore, major (JCGC grade ≥ 2a) pRR was found to be more predictive than the minor (JCGC grade ≥ 1b) pRR for non-type 4 gastric cancer, while the predictive difference between the cutoff of residual tumor < 10% and < 33% was quite small [25]. Recent phase II trials evaluating preoperative treatment in the West have often employed pCR rate as the primary endpoint [26]. In this context, the notably high pCR rate (24%) achieved with DOS in JCOG1704 supports the efficacy of this treatment.
While acknowledging the limitations of a single-arm phase II trial, it is important to note that this category of gastric cancer with ELM is relatively uncommon. Conducting a phase III trial with a large sample size might be impractical given the rarity of this condition. Thus, the current Japanese Gastric Cancer Treatment Guidelines describe preoperative CS followed by extended surgery and postoperative S-1 as the standard treatment for gastric cancer with ELM, on the basis of the findings from the JCOG0405 phase II trial. We believe DOS should replace CS as the new standard regimen for preoperative chemotherapy in gastric cancer with ELM.
Conclusions
Preoperative DOS chemotherapy for marginally resectable gastric cancer with ELM was associated with an impressive pathological response and a notable proportion of patients who achieved R0 resection. The manageable toxicity profile of preoperative DOS, along with favorable compliance for all three drugs, is noteworthy. In addition, the postoperative morbidity associated with D2 plus PAN dissection following DOS chemotherapy was limited. These findings suggest that this multimodal treatment approach is highly promising for treating gastric cancer with ELM.
References
International Agency for Research on Cancer. GLOBOCAN 2020. https://gco.iarc.fr/today/data/factsheets/cancers/39-All-cancers-fact-sheet.pdf. Accessed August 17, 2023.
Kurokawa Y, Doki Y, Mizusawa J, et al. Five-year follow-up of a randomized clinical trial comparing bursectomy and omentectomy alone for resectable gastric cancer (JCOG1001). Br J Surg. 2022;110:50–6.
Hashimoto T, Kurokawa Y, Mori M, et al. Update on the treatment of gastric cancer. JMA Journal. 2018;1:40–9.
Yanagimoto Y, Kurokawa Y, Doki Y. Essential updates 2021/2022: perioperative and surgical treatments for gastric and esophagogastric junction cancer. Ann Gastroenterol Surg. 2023;7:698–708.
Yoshikawa T, Sasako M, Yamamoto S, et al. Phase II study of neoadjuvant chemotherapy and extended surgery for locally advanced gastric cancer. Br J Surg. 2009;96:1015–22.
Tsuburaya A, Mizusawa J, Tanaka Y, et al. Neoadjuvant chemotherapy with S-1 and cisplatin followed by D2 gastrectomy with para-aortic lymph node dissection for gastric cancer with extensive lymph node metastasis. Br J Surg. 2014;101:653–60.
Takahari D, Ito S, Mizusawa J, et al. Long-term outcomes of preoperative docetaxel with cisplatin plus S-1 therapy for gastric cancer with extensive nodal metastasis (JCOG1002). Gastric Cancer. 2020;23:293–9.
Japanese Gastric Cancer Association. Japanese Gastric Cancer Treatment Guidelines 2021 (6th edition). Gastric Cancer. 2023;26:1–25.
Al-Batran SE, Homann N, Pauligk C, et al. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): a randomised, phase 2/3 trial. Lancet. 2019;393:1948–57.
Kang Y-K, Yook JH, Park Y-K, et al. PRODIGY: a phase III study of neoadjuvant docetaxel, oxaliplatin, and S-1 plus surgery and adjuvant S-1 versus surgery and adjuvant S-1 for resectable advanced gastric cancer. J Clin Oncol. 2021;39:2903–13.
Kang Y-K, Kim H-D, Yook JH, et al. Neoadjuvant docetaxel, oxaliplatin, and S-1 plus surgery and adjuvant S-1 for resectable advanced gastric cancer: final survival outcomes of the randomized phase 3 PRODIGY trial. J Clin Oncol. 2023;41(suppl 16; abstr 4067).
Saito T, Kurokawa Y, Takahashi T, et al. Neoadjuvant docetaxel, oxaliplatin and S-1 (DOS) combination chemotherapy for patients with resectable adenocarcinoma of esophagogastric junction. Gastric Cancer. 2022;25:966–72.
Kurokawa Y, Kawase T, Takeno A, et al. Phase 2 trial of neoadjuvant docetaxel, oxaliplatin, and S-1 for clinical stage III gastric or esophagogastric junction adenocarcinoma. Ann Gastroenterol Surg. 2023;7:247–54.
Sato Y, Kurokawa Y, Doki Y, et al. A phase II study of preoperative chemotherapy with DOS in gastric cancer with extensive lymph node metastasis (JCOG1704). Future Oncol. 2020;16:31–8.
Sano T, Sasako M, Yamamoto S, et al. Gastric cancer surgery: morbidity and mortality results from a prospective randomized controlled trial comparing D2 and extended para-aortic lymphadenectomy—Japan Clinical Oncology Group study 9501. J Clin Oncol. 2004;22:2767–73.
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–112.
Becker K, Mueller JD, Schulmacher C, et al. Histomorphology and grading of regression in gastric carcinoma treated with neoadjuvant chemotherapy. Cancer. 2003;98:1521–30.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Katayama H, Kurokawa Y, Nakamura K, et al. Extended Clavien–Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today. 2016;46:668–85.
Green S, Benedetti J, Crowley J. The design of clinical trials. In: Clinical trials in oncology, 2nd ed. Boca Raton: Chapman & Hall/CRC; 2003. p. 41–77.
Yamada Y, Higuchi K, Nishikawa K, et al. Phase III study comparing oxaliplatin plus S-1 with cisplatin plus S-1 in chemotherapy-naïve patients with advanced gastric cancer. Ann Oncol. 2015;26:141–8.
Al-Batran SE, Hofheinz RD, Pauligk C, et al. Histopathological regression after neoadjuvant docetaxel, oxaliplatin, fluorouracil, and leucovorin versus epirubicin, cisplatin, and fluorouracil or capecitabine in patients with resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4-AIO): results from the phase 2 part of a multicentre, open-label, randomised phase 2/3 trial. Lancet Oncol. 2016;17:1697–708.
Boku N, Yamamoto S, Fukuda H, et al. Fluorouracil versus combination of irinotecan plus cisplatin versus S-1 in metastatic gastric cancer: a randomised phase 3 study. Lancet Oncol. 2009;10:1063–9.
Kurokawa Y, Shibata T, Sasako M, et al. Validity of response assessment criteria in neoadjuvant chemotherapy for gastric cancer (JCOG0507-A). Gastric Cancer. 2014;17:514–21.
Nakamura K, Kuwata T, Shimoda T, et al. Determination of the optimal cutoff percentage of residual tumors to define the pathological response rate for gastric cancer treated with preoperative therapy (JCOG1004-A). Gastric Cancer. 2015;18:597–604.
Hofheinz RD, Merx K, Haag GM, et al. FLOT versus FLOT/trastuzumab/pertuzumab perioperative therapy of human epidermal growth factor receptor 2-positive resectable esophagogastric adenocarcinoma: a randomized phase II trial of the AIO EGA Study Group. J Clin Oncol. 2022;40:3750–61.
Acknowledgements
We thank Harumi Kaba and Kumiko Yanagida for data management, Haruhiko Fukuda for overseeing the management of this study, and Noriko Mitome, Yusuke Sano, Masayuki Yokoyama for helpful advice in writing the manuscript.
Funding
Open Access funding provided by Osaka University. This study was supported in part by the National Cancer Center Research and Development Fund (29-A-3, 2020-J-3, 2023-J-03).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yukinori Kurokawa and Yuichiro Doki have received research funding and lecture fees from Taiho Pharmaceutical, Ono Pharmaceutical, Yakult Honsha, Eli Lilly Japan, and Daiichi Sankyo outside of the submitted work. Haruhiko Cho has received lecture fees from Yakult Honsha outside of the submitted work. Junki Mizusawa has received lecture fees from Taiho Pharmaceutical outside the submitted work; His spouse an employee of Pfizer. Narikazu Boku has received research funding from Ono Pharmaceutical and Takeda Pharmaceutical and lecture fees from Taiho Pharmaceutical, Ono Pharmaceutical, Bristol Myers Squib Japan, Eli Lilly Japan, and Daiichi Sankyo outside of the submitted work. Masanori Terashima has received personal fees from Taiho Pharmaceutical, Chugai Pharmaceutical, Ono Pharmaceutical, Bristol Myers Squib Japan, Yakult Honsha, Takeda Pharmaceutical, Eli Lilly Japan, Pfizer Japan, Daiichi Sankyo, Johnson and Johnson, Medtronic Japan, Intuitive Japan, and Olympus outside of the submitted work.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the Japanese Clinical Trials Act and the related regulations and with the 1964 Helsinki Declaration and its later amendments. Informed consent to be included in the study was obtained from all patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kurokawa, Y., Doki, Y., Kitabayashi, R. et al. Short-term outcomes of preoperative chemotherapy with docetaxel, oxaliplatin, and S-1 for gastric cancer with extensive lymph node metastasis (JCOG1704). Gastric Cancer 27, 366–374 (2024). https://doi.org/10.1007/s10120-023-01453-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-023-01453-7