Abstract
Background
The optimal treatment strategy after first-line induction therapy in advanced HER2-positive oeso-gastric adenocarcinoma (OGA) remains challenging.
Methods
Patients treated with trastuzumab (T) plus platinum salts and fluoropyrimidine (F) as first-line chemotherapy between 2010 and 2020 for HER2-positive advanced OGA at 17 academic care centers in France, Italy, and Austria were included. The primary objective was the comparison of F + T vs T alone as maintenance regimen in terms of progression-free survival (PFS) and overall survival (OS) after a platinum-based chemotherapy induction + T. As secondary objective, PFS and OS between patients treated with reintroduction of initial chemotherapy or standard second-line chemotherapy at progression were assessed.
Results
Among the 157 patients included, 86 (55%) received F + T and 71 (45%) T alone as a maintenance regimen after a median of 4 months of induction chemotherapy. Median PFS from start of maintenance therapy was 5.1 months in both groups (95% CI 4.2–7.7 for F + T and 95% CI 3.7–7.5 for T alone; p = 0.60) and median OS was 15.2 (95% CI 10.9–19.1) and 17.0 months (95% CI 15.5–21.6) for F + T and T alone, respectively (p = 0.40). Of 112/157 patients (71%) receiving systemic therapy after progression under maintenance, 26/112 (23%) were treated with a reintroduction of initial chemotherapy + T and 86/112 (77%) with a standard second-line regimen. Here, median OS was significantly longer with the reintroduction (13.8 (95% CI 12.1–19.9) vs 9.0 months (95% CI 7.1–11.9); p = 0.007) as confirmed by multivariate analysis (HR 0.49; 95% CI 0.28–0.85; p = 0.01).
Conclusion
No additional benefit of adding F to T monotherapy as a maintenance treatment could be observed. Reintroduction of initial therapy at first progression may be a feasible approach to preserve later treatment lines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Overexpression of the human epidermal growth factor receptor 2 (HER2) was identified as predictive biomarker for the efficacy of trastuzumab (T) in advanced gastric cancer a decade ago and is present in 7–34% of patients [1,2,3,4]. The randomized phase III TOGA trial established T in combination with cisplatin and fluoropyrimidine (F) as standard first-line treatment in patients with advanced oeso-gastric adenocarcinoma since progression-free survival (PFS) as well as overall survival (OS) were remarkably improved by adding this targeted agent [5]. Given the toxicity profile of platinum salts, continuation of this regimen for a long period is often not feasible and may significantly impair quality of life of these patients. In line with that, patients without progression after 6 cycles of a cisplatin-based chemotherapy induction treated within the TOGA trial were deescalated to T monotherapy as maintenance regimen. However, many centers are not following this de-escalation after 6 cycles and may continue the full treatment regimen or F + T until limiting toxicity or disease progression. Also, many centers use oxaliplatin instead of cisplatin in daily clinical routine due to its easiest way of administration and to the results of several non-randomized trials, showing promising outcomes compared to the original cisplatin-based regimen of the TOGA trial [6, 7]. Nevertheless cumulative peripheral sensory neuropathy induced by oxaliplatin may also necessitate early chemotherapy de-escalation with this regimen[7].
Altogether, tough different chemotherapy regimens may be combined with T in HER2-positive advanced gastric cancer, the optimal maintenance strategy after first-line platinum-based induction remains unknown.
Within two small retrospective studies of maintenance regimens in this setting, PFS from induction treatment was 6 months under continuation of T alone, and 12 months when combined with capecitabine[8, 9]. The only prospective observational study to date included 78 Chinese patients with metastatic gastric cancer and revealed an—albeit not significantly—improved PFS and OS with the combination of a single agent chemotherapy and T compared to T alone [10].
In this uniquely large, retrospective, international, multicentric study, we aimed to investigate the optimal treatment strategy after induction chemotherapy in the first-line setting of HER2-positive oeso-gastric cancer. We therefore assessed different maintenance regimens as well as the role of reintroduction of the initial regimen at progressive disease.
Methods
Patients
For this retrospective, multicentric, international study, patients with histologically proven HER2-positive advanced (locally advanced or metastatic) gastric or gastroesophageal junction (GEJ) adenocarcinoma treated in 17 centers in France, Italy, and Austria between January 2010 and December 2020 were included. All patients received at least one cycle of a first-line doublet chemotherapy of a platinum salt with F in combination with T followed by a maintenance therapy with either a combination of F and T or T alone. Patients with incomplete information on their clinical course of disease were excluded.
Patients were included into this study only if information on HER2 status was available and HER2 testing was conducted according to international standards. HER2 positivity was defined as immunohistochemical staining intensity of either 3 + or 2 + with a positive HER2 deoxyribonucleic acid (DNA) amplification tested by fluorescence in situ hybridization (FISH) [11].
Information relating to patient demographics, case history, and survival were collected by each treating center by retrospective chart review. This study was conducted in accordance with the Declaration of Helsinki and approval by each national institutional review board (IRB) was obtained. Data of patients were centralized within a password-secured REDCAP database. Treatment decisions were taken in an interdisciplinary tumor board.
Study design and objectives
As primary objective, we aimed to investigate the impact of F + T and T alone as maintenance regimens after a platinum-based doublet chemotherapy + T induction in the first-line setting of advanced oeso-gastric cancer patients. As secondary objective, we compared reintroduction of induction chemotherapy vs standard second-line treatment in patients receiving subsequent systemic therapy after progression under maintenance therapy.
Statistical analysis
For the primary objective, investigating the association between maintenance regimens and PFS/OS, patients were grouped in being treated with a combination of F + T or T monotherapy. Here, PFS was defined as interval from start of maintenance treatment until progressive disease or death of any cause. OS was defined as interval from start of maintenance treatment until death of any cause or last date of follow-up.
For the secondary objective, investigating the association of different treatment strategies at progression under first-line maintenance with PFS/OS, patients were grouped in being treated with reintroduction of initial chemotherapy or standard second-line therapy. For this question, PFS was defined as interval from start of reintroduction/second-line therapy until progressive disease or death of any cause. OS was defined as interval from start of reintroduction/second-line therapy until death of any cause or last date of follow-up.
PFS and OS were estimated using Kaplan–Meier (KM) method and described using median or rate at specific time points with their 95% confidence intervals (95% CI). Follow-up was calculated using a reverse KM estimation. To test for differences between survival curves, the log-rank test was used. The association between patients’ characteristics and survival endpoints was assessed with univariate Cox regression models for both objectives. Factors included in the multivariable analyses were baseline prognostic factors identified in univariable analyses (p value < 0.10) in addition to clinically relevant factors. For the first objective, we therefore included besides maintenance regimen, gender, age at advanced disease, number of metastatic sites, duration of first-line therapy, reason for de-escalation to maintenance, and ECOG PS at maintenance as clinically relevant factors and HER2 expression and metachronous/synchronous metastases as significant factors from univariable analysis into multivariable analysis for PFS and gender, age at advanced disease, number of metastatic sites, duration of first-line therapy, reason for de-escalation to maintenance, and ECOG PS at maintenance as clinically relevant factors and metachronous/synchronous metastases as significant factor from univariable analysis into multivariable analysis for OS. For the second objective, we included besides treatment strategy after maintenance, gender and age at advanced disease as clinically relevant factors and ECOG PS as significant factor from univariable analysis into multivariable analyses for PFS as well as OS.
Median (range) values and proportions (percentage) were provided for the description of continuous and categorical variables, respectively. Median and proportions were compared using Wilcoxon–Mann–Whitney test and Chi-square test (or Fisher’s exact test, if appropriate), respectively. p values of less than 0.05 were considered statistically significant, and all tests were two sided. All analyses were performed using SAS version 9.4 (SAS Institute, Cary NC) and R software version 2.15.2 (R Development Core Team, Vienna, Austria; http://www.r-project.org).
Results
Patients characteristics
Among 253 patients with HER2-positive unresectable or metastatic oeso-gastric cancer who were collected for the present study, 44 had to be excluded due to incomplete information on their clinical course of disease leaving 209 patients who received at least one cycle of a first-line doublet chemotherapy of a platinum salt with F in combination with T. For 23 patients, induction therapy was stopped early due to progressive disease at first restaging. Among remaining patients, induction chemotherapy was continued until disease progression or death in 17 patients, and completely stopped after a median of 5 months (range 2–6) when stabilization of the disease was obtained in 12 patients. In 157 patients, induction chemotherapy was deescalated to a F + T or T maintenance regimen representing the final patient cohort for the present study (Fig. 1).
Patients presented with a median age of 63 years (range 16 to 88), a median ECOG Performance Status (ECOG PS) of 0–1 in 95%, and with a median of 2 metastatic sites (range 0 to 5) at start of induction chemotherapy. Three of 157 patients (2%) had a locally advanced tumor, whereas 151/157 patients (98%) presented with metastatic disease at diagnosis. Seventy-seven of 157 patients (49%) received an oxaliplatin-based, 79/157 patients (50%) a cisplatin-based, and 1/157 patients (1%) a carboplatin-based chemotherapy induction regimen in combination with T over a median of 4 months. Median PFS and OS from start of induction chemotherapy were 10.8 months and 21.5 months, respectively. Detailed patients’ characteristics of the overall cohort are listed within Table 1.
Maintenance therapies and their association with PFS and OS
Eighty-six of 157 patients (55%) were treated with a combination of F and T and 71 (45%) with T monotherapy as a maintenance regimen. Patients’ characteristics were generally well balanced between the two groups except for more patients with an esophageal primary tumor (p = 0.04), a well-differentiated tumor grading (p < 0.001), with synchronous metastases (p < 0.001), treated with oxaliplatin-based induction chemotherapy (p < 0.001) and a de-escalation to maintenance due to toxicity (p < 0.001) in the F + T combination regimen group. Detailed patients’ characteristics according to maintenance regimens are listed within Table 1.
From maintenance start, median PFS of patients treated with F + T and those treated with T alone did not differ significantly (5.1 vs 5.1 months; p = 0.60). Median OS was not significantly different either between the two groups (15.2 vs 17.0 months; p = 0.40). Corresponding KM curves are illustrated within Fig. 2.
Within the performed multivariable analysis, metachronous metastases (p < 0.01) and HER2 3 + (p = 0.01) were independently associated with longer PFS. Metachronous metastases was the only factor independently associated with longer OS (p = 0.01). Results of the univariable and multivariable analyses are listed within Table 2.
Treatment strategies at disease progression during maintenance therapy and their association with PFS and OS
Among 112/157 patients (71%) receiving systemic treatment after progression under maintenance first-line therapy, 26 patients (23%) were treated by a reintroduction of the platinum-based chemotherapy induction in combination with T and 86 patients (77%) were switched directly to a standard second-line chemotherapy regimen. Patients’ characteristics were generally well balanced between the two groups without any significantly different parameters identified. Detailed patients’ characteristics of the overall cohort at progression under maintenance therapy as well as according to treatment strategies are listed within Table 3.
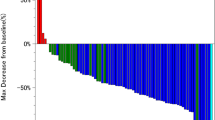
Median PFS was 4.4 months in the reintroduction therapy and 3.7 months in the second-line group (p = 0.10). Median OS was significantly longer in patients receiving reintroduction compared to patients with second-line therapy (13.8 vs 9.0 months; p = 0.007). Corresponding KM curves are illustrated within Fig. 3.
Within the performed multivariable analysis, none of the factors was identified to be independently associated with PFS. Treatment strategy after maintenance remained the only factor independently associated with longer OS (p = 0.01). Results of the univariable and multivariable analyses are listed within Table 4.
Conclusion
The aim of the present multinational study was to assess the optimal treatment strategy after first-line plantinum-based doublet chemotherapy plus T induction in advanced HER2-positive oeso-gastric cancer patients. We investigated the association of different maintenance regimens with PFS/OS as well as the question of reintroduction of induction chemotherapy at progression. This seems especially important considering that only 9% of patients who started first-line induction therapy continue it for a longer period of time and 6% of patients will stop it compeletely as observed within the present study.
Addressing the first objective of our study, we did not observe a significant improvement of PFS or OS with the combination of F + T as compared to T alone. Since there is no randomized prospective clinical trial investigating the question of optimal maintenance therapy in this setting so far, no direct comparisons of our results can be made. In the TOGA trial, patients were treated with a first-line induction chemotherapy of 5-fluorouracil (5-FU)/Capecitabine + Cisplatin + T for 6 cycles followed by a maintenance therapy with T alone and this should remain the standard maintenance strategy. However, the phase III KEYNOTE-811 study showed promising activity of first-line chemotherapy plus T and the anti-PD-1 agent pembrolizumab and this upfront regimen has been approved by the Food And Drug Administration (FDA) based on the preliminary objective response rate (ORR) results pending survival data analysis [12]. Therefore, in case of confirmation of the preliminary results, optimal maintenance strategies will need to be re-assessed in the frame of pembrolizumab-based therapy, especially considering that KEYNOTE-811 did not pre-specify the duration of induction chemotherapy.
Whereas in other tumor entities like metastatic RAS-wildtype colorectal cancer (CRC), the combination of a single agent chemotherapy with a monoclonal antibody inhibiting the epidermal growth factor receptor (EGFR) as maintenance treatment was shown to be more effective than either one of the agents alone [13, 14], HER2-targeted therapy may be more potent as a monotherapy due to its multiple and diverse mechanisms of action [15,16,17,18,19]. In line with that, the targeted approach of dual HER2 inhibition by T and pertuzumab represents the standard maintenance treatment after first-line induction with a taxane chemotherapy backbone in HER2-positive breast cancer since many years [20]. In HER2-positive gastric cancer, however, several HER2-targeted treatment approaches being effective in HER2-positive breast cancer patients failed to improve outcome [21,22,23,24,25]. Distinct differences in the tumor biologies as well as in resistance mechanisms between these two HER2-positive cancer entities may be an explanation. Nevertheless, the targeted approach of T alone resulted in the same efficacy as in combination with chemotherapy in the present study. Considering the importance of quality of life in this palliative patient population, the generally better toxicity profile and practicability of application of the HER2-targeted agent also argue for the importance of its continuation in this setting.
Within the multivariable analysis we performed for the maintenance treatment strategies of T +/- F, HER2 3 + expression rate as well as metachronous metastases were independently associated with longer PFS and the latter also with longer OS. Whereas some studies suggested an impaired prognosis of gastric cancer patients with higher HER2 levels due to an increased disease aggressiveness, a post hoc analysis of the TOGA trial observed a 4.2 months survival benefit in patients with higher HER2 levels [1, 3, 5]. Here, an increased sensitivity for the targeted agent most likely caused an improved efficacy, which could explain the significant association of HER2 positivity in our study as well. The prognostic role of synchronous metastatic disease, however, has been well explored by several studies, and thus the negative prognostic impact observed in our study seems comprehensible [26].
As secondary objective of our study, we investigated the question of reintroduction of initial chemotherapy at progression under maintenance therapy and observed a significantly prolonged OS compared to patients treated with standard second-line therapy. The strategy of reintroduction of a chemotherapy agent at progression under maintenance had been investigated so far most notably in metastatic CRC patients. Here, a treatment stop of oxaliplatin during maintenance and its reintroduction at progression was shown to be as efficient or even beneficial to a full core treatment continuation or a subsequent, direct switch to second-line treatment [27,28,29]. Considering the limited prognosis of patients with advanced gastric cancer, maintenance followed by a reintroduction of a chemotherapy agent may, therefore allow to preserve later treatment lines and improve quality of life. However, these findings should be interpreted with caution since the choice of reintroduction may have also been related to the association with more favorable prognostic features and treatment responsiveness.
The main strength of our study lies in the multicentric, multinational design involving a broad diversity in treatment strategies according to different centers’ clinical practice. Main study limitation is the retrospective design, which did not allow for a standardized duration and type of induction treatment in all patients. De-escalation to maintenance therapy was not only performed as pre-planned, but also due to toxicity reasons, which may implicate some bias of selection. Physicians choice of therapies differed between participating countries and centers, and thus treatment lines after first-line were heterogenous. Sample sizes of patients especially for the analyses of the second objective were rather low, and therefore the detected results have to be interpreted with caution. Detailed information about patients’ characteristics and the clinical course of disease was sometimes incomplete. Moreover, information about therapy-associated toxicity and quality of life would have been of interest to further compare treatment strategies. However, to our best knowledge, the present study represents the largest so far published population of advanced HER2-positive oeso-gastric patients investigating different maintenance regimens as well as treatment strategies at progression thereafter.
In conclusion, no difference between F + T and T as maintenance therapy could be observed in terms of PFS and OS within this uniquely large patient population. Therefore, de-escalation to a single targeted treatment approach may serve as a feasible option in the maintenance setting. Moreover, reintroduction instead of a direct switch to second-line treatment at progression under maintenance may be beneficial since OS was significantly and independently longer in these patients. Our findings may help to support treatment decisions in this setting.
Data availability
All data generated or analyzed during this study are included in this published article.
Abbreviations
- 5-FU:
-
5-Fluoururacil
- CI:
-
Confidence intervals
- CRC:
-
Colorectal cancer
- DNA:
-
Deoxyribonucleic acid
- F:
-
Fluoropyrimidine
- ECOG PS:
-
ECOG Performance Status
- EGFR:
-
Epidermal growth factor receptor
- FDA:
-
Food And Drug Administration
- FISH:
-
Fluorescence in situ hybridization
- GEJ:
-
Gastroesophageal junction
- HER2:
-
Human epidermal growth factor receptor 2
- IRB:
-
Institutional review board
- KM:
-
Kaplan–Meier
- ORR:
-
Objective response rate
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- T:
-
Trastuzumab
References
Tanner M, Hollmén M, Junttila TT, Kapanen AI, Tommola S, Soini Y, et al. Amplification of HER-2 in gastric carcinoma: association with Topoisomerase IIalpha gene amplification, intestinal type, poor prognosis and sensitivity to trastuzumab. Ann Oncol England. 2005;16:273–8.
Hofmann M, Stoss O, Shi D, Büttner R, van de Vijver M, Kim W, et al. Assessment of a HER2 scoring system for gastric cancer: results from a validation study. Histopathology England. 2008;52:797–805.
Gravalos C, Jimeno A. HER2 in gastric cancer: a new prognostic factor and a novel therapeutic target. Ann Oncol England. 2008;19:1523–9.
Palle J, Rochand A, Pernot S, Gallois C, Taïeb J, Zaanan A. Human epidermal growth factor receptor 2 (HER2) in advanced gastric cancer: current knowledge and future perspectives. Drugs New Zealand. 2020;80:401–15.
Bang Y-J, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet (London, England). 2010;376:687–97.
Soularue É, Cohen R, Tournigand C, Zaanan A, Louvet C, Bachet J-B, et al. Efficacy and safety of trastuzumab in combination with oxaliplatin and fluorouracil-based chemotherapy for patients with HER2-positive metastatic gastric and gastro-oesophageal junction adenocarcinoma patients: a retrospective study. Bull Cancer France. 2015;102:324–31.
Ryu M-H, Yoo C, Kim JG, Ryoo B-Y, Park YS, Park SR, et al. Multicenter phase II study of trastuzumab in combination with capecitabine and oxaliplatin for advanced gastric cancer. Eur J Cancer England. 2015;51:482–8.
Fu X, Zhang Y, Yang J, Qi Y, Ming Y, Sun M, et al. Efficacy and safety of trastuzumab as maintenance or palliative therapy in advanced HER2-positive gastric cancer. Onco Targets Ther. 2018;11:6091–100.
Gürbüz M, Akkuş E, Sakin A, Urvay S, Demiray AG, Şahin S, et al. Trastuzumab ± Capecitabine maintenance after the first-line treatment of HER2-positive advanced gastric cancer: retrospective observational real-life data of Turkish Oncology Group. J Gastrointest Cancer. 2021;53(2):282–8.
Li Q, Lv M, Jiang H, Wang Y, Yu S, Li W, et al. A prospective observational study on the optimal maintenance strategy in HER2-positive advanced gastric cancer treated with trastuzumab-based therapy. J Cancer Res Clin Oncol Germany. 2020;146:287–95.
Rüschoff J, Hanna W, Bilous M, Hofmann M, Osamura RY, Penault-Llorca F, et al. HER2 testing in gastric cancer: a practical approach. Mod Pathol an Off J United States Can Acad Pathol Inc. United States; 2012;25:637–50.
Janjigian YY, Kawazoe A, Yañez P, Li N, Lonardi S, Kolesnik O, et al. The KEYNOTE-811 trial of dual PD-1 and HER2 blockade in HER2-positive gastric cancer. Nature England. 2021;600:727–30.
Modest DP, Karthaus M, Frühauf S, Graeven U, Müller L, Koenig A, et al. Maintenance therapy with 5-fluoruracil/leucovorin (5FU/LV) plus panitumumab (pmab) or 5FU/LV alone in RAS wildtype (WT) metastatic colorectal cancer (mCRC) - the PANAMA trial (AIO KRK 0212). J Clin Oncol Wolters Kluwer. 2021;39:3503.
Pietrantonio F, Morano F, Corallo S, Miceli R, Lonardi S, Raimondi A, et al. Maintenance therapy with panitumumab alone vs panitumumab plus fluorouracil-leucovorin in patients with RAS wild-type metastatic colorectal cancer: a phase 2 randomized clinical trial. JAMA Oncol. 2019;5:1268–75.
Valabrega G, Montemurro F, Aglietta M. Trastuzumab: mechanism of action, resistance and future perspectives in HER2-overexpressing breast cancer. Ann Oncol. 2007;18:977–84.
Clynes RA, Towers TL, Presta LG, Ravetch JV. Inhibitory Fc receptors modulate in vivo cytotoxicity against tumor targets. Nat Med United States. 2000;6:443–6.
Yen L, You XL, Al Moustafa AE, Batist G, Hynes NE, Mader S, et al. Heregulin selectively upregulates vascular endothelial growth factor secretion in cancer cells and stimulates angiogenesis. Oncogene England. 2000;19:3460–9.
Molina MA, Codony-Servat J, Albanell J, Rojo F, Arribas J, Baselga J. Trastuzumab (herceptin), a humanized anti-Her2 receptor monoclonal antibody, inhibits basal and activated Her2 ectodomain cleavage in breast cancer cells. Cancer Res United States. 2001;61:4744–9.
Nagata Y, Lan K-H, Zhou X, Tan M, Esteva FJ, Sahin AA, et al. PTEN activation contributes to tumor inhibition by trastuzumab, and loss of PTEN predicts trastuzumab resistance in patients. Cancer Cell United States. 2004;6:117–27.
Swain SM, Miles D, Kim S-B, Im Y-H, Im S-A, Semiglazov V, et al. Pertuzumab, trastuzumab, and docetaxel for HER2-positive metastatic breast cancer (CLEOPATRA): end-of-study results from a double-blind, randomised, placebo-controlled, phase 3 study. Lancet Oncol England. 2020;21:519–30.
Tabernero J, Hoff PM, Shen L, Ohtsu A, Shah MA, Cheng K, et al. Pertuzumab plus trastuzumab and chemotherapy for HER2-positive metastatic gastric or gastro-oesophageal junction cancer (JACOB): final analysis of a double-blind, randomised, placebo-controlled phase 3 study. Lancet Oncol England. 2018;19:1372–84.
Satoh T, Xu R-H, Chung HC, Sun G-P, Doi T, Xu J-M, et al. Lapatinib plus paclitaxel versus paclitaxel alone in the second-line treatment of HER2-amplified advanced gastric cancer in Asian populations: TyTAN–a randomized, phase III study. J Clin Oncol United States. 2014;32:2039–49.
Hecht JR, Bang Y-J, Qin SK, Chung HC, Xu JM, Park JO, et al. Lapatinib in combination with capecitabine plus oxaliplatin in human epidermal growth factor receptor 2-positive advanced or metastatic gastric, esophageal, or gastroesophageal adenocarcinoma: TRIO-013/LOGiC–a randomized phase III trial. J Clin Oncol United States. 2016;34:443–51.
Thuss-Patience PC, Shah MA, Ohtsu A, Van Cutsem E, Ajani JA, Castro H, et al. Trastuzumab emtansine versus taxane use for previously treated HER2-positive locally advanced or metastatic gastric or gastro-oesophageal junction adenocarcinoma (GATSBY): an international randomised, open-label, adaptive, phase 2/3 study. Lancet Oncol England. 2017;18:640–53.
Janjigian YY, Ku GY, Ilson DH, Boyar MS, Capanu M, Chou JF, et al. A phase II study of afatinib in patients (pts) with metastatic human epidermal growth factor receptor (HER2)-positive trastuzumab refractory esophagogastric (EG) cancer. J Clin Oncol Wolters Kluwer. 2015;33:59.
Lordick F, Carneiro F, Cascinu S, Fleitas T, Haustermans K, Piessen G, et al. Gastric cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann Oncol England. 2022;33(10):1005–20.
Tournigand C, Cervantes A, Figer A, Lledo G, Flesch M, Buyse M, et al. OPTIMOX1: a randomized study of FOLFOX4 or FOLFOX7 with oxaliplatin in a stop-and-Go fashion in advanced colorectal cancer–a GERCOR study. J Clin Oncol United States. 2006;24:394–400.
André T, Tournigand C, Mineur L, Fellague-Chebra R, Flesch M, Mabro M, et al. Phase II study of an optimized 5-fluorouracil-oxaliplatin strategy (OPTIMOX2) with celecoxib in metastatic colorectal cancer: a GERCOR study. Ann Oncol England. 2007;18:77–81.
Fucà G, Raimondi A, Prisciandaro M, Lonardi S, Cremolini C, Ratti M, et al. Reinduction of an Anti-EGFR-based first-line regimen in patients with RAS wild-type metastatic colorectal cancer enrolled in the Valentino Study. Oncologist. 2022;27:e29-36.
Acknowledgements
We thank the European Society of Medical Oncology (ESMO) for supporting ESB by a translational research fellowship.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conceptualization: ESB, EA, AZ; data curation: EA; formal analysis: EA; funding acquisition: AZ; investigation: ESB, EA, AZ; methodology: ESB, EA, AZ; project administration: AZ; resources: ESB, EA, AZ; software: EA; supervision: AZ; validation: LP, AIM, GWP, FP, MA, FG, DB, GA, RL, VH, DT, PA, MM, AD, GR, MBA, IC, CT, LM, RG, JT, AZ; visualization: ESB, EA; writing—original draft: ESB, EA, AZ; writing—review and editing: ESB, LP, AIM, GWP, FP, MA, FG, DB, GA, RL, VH, DT, PA, MM, AD, GR, MBA, IC, CT, LM, RG, JT, AZ.
Corresponding author
Ethics declarations
Conflict of interest
EA has participated in advisory boards for Amgen and Sanofi Genzymes. AIM has participated in advisory boards organized by MSD, Servier, and BMS; recived lecture honoraria from Eli Lilly, Servier, BMS, and MSD; is a local PI for clinical trials sponsored by BMS and Roche; declares a consulting role for Astellas and MSD; and received travel support from BMS, Roche, Eli Lilly, and Daiichi Sankyo. GWP declares advisory roles for Merck, Amgen, Roche, Servier, Bayer, Pierre Fabre, MSD, BMS, AstraZeneca, and Daiichi Sankyo. FP has received honoraria as a speaker or in an advisory role from ASTRAZENECA, BMS, MSD, MERCK-SERONO, AMGEN, PIERRE FABRE, LILLY, and SERVIER and received research grants from Astrazeneca, Incyte, and BMS. DT has participated in consulting and/or advisory boards for Amgen, Merck, Roche, Sanofi, Servier, Pierre Fabre, MSD, BMS, Astra Zeneca, and Daiichi Sankyo. PA declares consulting or advisory roles for Servier, Pierre-Fabre, AstraZeneca, BMS, MSD, Amgen, Viatris travel and accommodations or expenses from Servier, Pierre-Fabre. AD has participated in advisory boards for Amgen, Roche, Servier, and AstraZeneca. GR declares consulting or an advisory role for Servier, AstraZeneca, Bristol Myers Squibb, MSD, Servier, Amgen, Ipsen, Viatris, Accord Healthcare, Sanofi and travel, accommodations or expenses from Servier, AstraZeneca, Bristol Myers Squibb, MSD, Roche, Amgen, Ipsen. MBA participated in advisory boards for Merck Serono, BMS, Incyte, Amgen, Pierre Fabre, Servier, Sanofi, IPSEN, and Bayer. CT participated in consulting and/or advisory boards for Amgen, Astra-Zeneca, Bayer, BMS, Ipsen, Merck, MSD, Pierre Fabre, Sanofi, and Servier. RG has received honoraria as a speaker or in an advisory role from AAA, AMGEN, BMS, IPSEN, MSD, PIERRE FABRE, ROCHE, and SERVIER. JT has received honoraria as a speaker or in an advisory role from AMGEN, ASTELLAS, BMS, MSD, MERCK, NOVARTIS, PIERRE FABRE, ROCHE, and SERVIER. AZ has participated in consulting and/or advisory boards for Amgen, Merck, Roche, Sanofi, Servier, Baxter, Havas Life, Alira Health, Zymeworks, MSD, BMS, AstraZeneka, Daiichi Sankyo. All other authors declare no conflicts of interests.
Ethical approval and consent to participate.
This study was conducted in accordance with the Declaration of Helsinki and approval by each national institutional review board (IRB) was obtained.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bergen, E.S., Pilla, L., Auclin, E. et al. Optimal treatment strategy after first-line induction therapy in advanced HER2-positive oeso-gastric adenocarcinoma—a retrospective, international, multicentric AGEO study. Gastric Cancer 26, 425–437 (2023). https://doi.org/10.1007/s10120-023-01374-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-023-01374-5