Abstract
Objective
Endoscopic resection (ER) is an effective treatment method for gastric submucosal tumors (G-SMTs), but endoscopic resection failure requires emergency surgery. The purpose of this study was to assess potential risk factors for endoscopic resection failure.
Methods
A total of 1041 patients with G-SMT undergoing endoscopic resection were enrolled. Twenty-five patients in whom endoscopic resection failed, requiring a transition to surgery midway through the operation, were included in the failed group, and 1016 patients who received successful endoscopic resection were included in the successful endoscopic resection group. Baseline and lesion characteristics were recorded, and the differences in tumor characteristics and risk factors for resection failure of G-SMT were analyzed. Sensitivity analysis was performed to detect the stability of the indicator.
Results
Of the 1041cases included, there were 25 cases (2.4%) of failed endoscopic resection. Binary logistic analysis showed that the independent risk factors included tumors originating from deep muscularis propria(OR = 14.42, 95% CI 4.47–46.52), size > 3 cm (OR = 7.75, 95% CI 2.64–22.70), exophytic growth pattern (OR = 4.98, 95% CI 1.62–15.29), endoscopist with less experience (OR = 5.99, 95% CI 1.07–12.19), and irregular borders (OR = 4.13, 95% CI 1.40–12.19). The stable risk factors were tumors size, tumor origin and growth pattern according to sensitivity analysis.
Conclusions
Tumors originating from the deep muscularis propria, tumor size > 3 cm, endoscopists with less experience, an exophytic growth pattern, and irregular boundaries were found to be independent risk factors for endoscopic resection failure. To reduce the risk of endoscopic resection failure, physicians should carefully evaluate G-SMT characteristics preoperative.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric submucosal tumors (G-SMTs) refer to tumors that originate below the gastric mucosal layer, mainly including gastrointestinal stromal tumors (GISTs), neurogenic tumors, leiomyomas and lipomas. Most of them have no clinical symptoms and are incidentally detected during upper endoscopic examination; however, the malignant transformation of GISTs, the most frequent gastric mesenchymal neoplasm arising from the muscularis propria (MP) of the stomach, can occur in up to 10–30% of cases [1,2,3,4,5]. Some benign tumors can also cause abdominal pain, bleeding and other clinical manifestations. According to the guidelines established by the National Comprehensive Cancer Network (NCCN), resection is the first-line treatment for nonmetastatic GISTs > 2 cm. However, GISTs < 2 cm that lack high-risk features upon endoscopic ultrasound (EUS) only require monitoring and follow-up every 1–2 years [6]. Unfortunately, long-term follow-up can make patients feel anxious, and even GIST tumors < 2 cm with < 5 mitoses/50 high-power fields (HPF) can metastasize, although it is rare [7, 8].
Endoscopic resection (ER) is a minimally invasive treatment that is characterized by less trauma, a high overall resection rate, quick postoperative recovery, few adverse events and excellent long-term results [9,10,11]. In addition, ER can achieve similar oncological outcomes as surgical treatment for G-SMTs less than 5 cm in size [12, 13]. Most G-SMTs do not cause lymph node metastasis [14,15,16] and can be removed directly without the need for lymph node dissection. Thus, ER has become a suitable choice for the treatment of small G-SMTs [17, 18].
However, the accurate assessment of surgical indications and the complete resection rate still have important clinical significance for G-SMT patients who undergo ER [19]. Preoperative evaluations such as endoscopy, ultrasound endoscopy (EUS), and computed tomography (CT) assessment are useful for avoiding clinical misjudgments and in guiding G-SMT treatment strategies [20,21,22,23]. With the continuous expansion of the indications for the ER of G-SMTs [24], more challenging cases of G-SMTs have been attempted, and ER failure has become an emerging issue. In these cases, emergency surgery is required to manage bleeding or even to save the patient’s life. This situation not only increases medical risks but also increases the patient burden. The combination of EUS and CT examination before ER could allow for a more reliable preoperative assessment of the risk factors for ER failure. However, to date, few studies have analyzed the risk factors for ER failure in G-SMT patients. Thus, we performed this study to summarize the characteristics of G-SMT patients who underwent ER from 2013 to 2020 at our hospital and aimed to identify reliable risk factors for ER failure in these patients.
Materials and methods
Patient recruitment
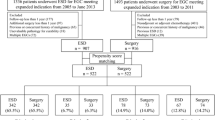
This study was a retrospective case–control study. A total of 1041 G-SMT patients who underwent ER in the Department of Gastroenterology, the First Affiliated Hospital of Nanjing Medical University, from January 2013 to December 2020 were included (Fig. 1). This work was approved by the Ethics Committee of the First Affiliated Hospital of Nanjing Medical University (2021-SR-449).
Patients diagnosed with G-SMTs who underwent ER were considered for inclusion. The principal inclusion criteria were as follows: (1) tumors originating from the MP according to EUS; (2) no evidence of lymph node involvement, intraperitoneal implantation or distant metastasis; and (3) written informed consent to undergo ER. Exclusion criteria were as follows: (1) patients with nonneoplastic lesions; (2) patients with missing data. All patients without any coagulation dysfunction and could tolerate anesthesia intubation.
Standard definitions were used, as follows: ER failure: The tumor could not be removed by ER (including ESD and EFTR), and the patient required emergency surgery for further surgical remediation. Successful ER: The tumor could be completely removed by ER.
The groups and selection strategy were as follows: The case group included patients who experienced ER failure. A total of 25 patients were included in this group through the continuous enrollment method. The control group included patients who successfully underwent ER. A total of 1016 patients were included in this group through the continuous enrollment method. The 1041 G-SMTs included GISTs (709 cases), leiomyomas (106 cases), heterotopic pancreas (82 cases), lipomas (76 cases), neuroendocrine tumors (17 cases), schwannomas (12 cases), glomus tumors (8 cases) and others (31 cases). Except for one neuroendocrine tumor (G3), most of the other tumors were benign, and this patient underwent additional surgery.
Surgical instruments, surgical methods and pathological examinations
Instruments
The instruments used included an electronic gastro-scope (Olympus GIFQ260J), dual channel endoscopy (Olympus GIF-2T0260M), radial-scanning echo endoscopy unit (Olympus UM 240), ultrasonic micro probe (OlympusUM-2R), linear array endoscope (EG-3830, Pentax), color doppler ultrasound (Hitachi Vision Avius L, Japan), IT knife (Olympus KD-611L), dual knife (Olympus KD-650Q/L), single use injector (Olympus NM-400L-0423), electrosurgical hemostatic forceps (Olympus FD-410LR), disposable electrosurgical snare (Olympus SD-210U-25), metal clamp (micro-tech (Nanjing) ROCC-D-26-195-C), rotatable grasping forceps (Olympus FG-44NR-1), endoloop (MAJ-254; Olympus), ERBE electric cutting device and CO2 gas pump, micro probe (Olympus UMDP12-25R), etc.
Endoscopic resection methods
ER was performed in all cases under intravenous anesthesia and with tracheal intubation. The patients were placed in the left decubitus position for all procedures.
Endoscopic ultrasonography (EUS) was used to record the echo intensity, echo uniformity, origin level, and tumor size. The superficial MP layer was defined as the upper half of the fourth layer with the tumor capsule located in the upper half of the fourth layer. The deep MP layer was defined as the lower half of the fourth layer with the tumor capsule located in the lower half of the fourth layer or tightly adhered to the fifth layer [20].
Endoscopic submucosal dissection (ESD) was performed according to Xin-gang Shi et al. [24]: Marking dots were placed around the tumors with an argon plasma coagulation (APC)/dual knife, and a submucosal injection of 100 ml saline + 2 ml indigo carmine + 1 ml adrenaline was administered near the marking dots. A dual knife was used to cut around the lesion to the submucosa. The submucosal layer was dissected until the tumor was exposed. Separation was continued until the tumor was completely removed while keeping the MP layer intact. After hemostasis on the wound surface was performed with hot forceps, the wound surface was clamped by metal clips.
For endoscopic full-thickness resection (EFTR) [24], marking dots were placed, cuts were made around the dots, and then submucosal layer dissection was performed in the same manner as in the ESD procedure. When the tumor was located in the deep MP layer or close to the serosa, a circumferential incision into the serous membrane around the tumor was performed with an IT knife, and an “artificial” perforation was made. Metal clips were used to close the wound surface in some easy cases.
For patients with SMTs originating from deep MP or exophytic growth, the “traction” method was necessary [25, 26]. The main “traction” method used is described as follows: Using a dual-channel endoscopy to perform ER, rotatable grasping forceps and a snare were placed separately using the two channels. The snare was enlarged and anchored to the bottom of the SMT, and then rotatable grasping forceps were used to grasp the tumor before the final resection cut. Thus, the tumor could be freed from the GI wall while preventing it from falling into the peritoneal cavity (Fig. 2). For cases with defects larger than 20 mm, a purse-string suture is usually required, as follows [27,28,29]: an endoloop is made, and clips are placed at the proximal edge of the defect, with the endoloop anchored by the endoclips at the edges around the defect. After the endoloop is tightened, the wound surface is closed simultaneously from the rim to the center. Additional clips can be placed to obtain complete wound closure if necessary. If a pneumoperitoneum develops, a 20-gauge needle can be used to insect into the right lower quadrant to release gas [30].
Complete tumor resection assisted by the “traction” method. a Foreign-body forceps and snares were inserted through the double cavity mirror channel. b SMT of the gastric fundus was separated to the serosa layer, and perforation occurred. c Snare was opened, and the foreign-body forceps were ready. d, e Foreign-body forceps were used to grasp the tumor, lift or push it to fully expose the bottom of the tumor, and then the snare was tightened and the tumor was removed. f Tumor was removed from the body
a, b Endoluminal growth pattern: CT scan showed dominant tumor located in the gastric cavity; c, d Exophytic growth pattern: CT scan showed dominant tumor was outside the gastric cavity; e–g Superficial-MP tumor: endoscopic ultrasound shows tumor capsule was in the upper half of the mucosal propria layer; h deep-MP tumor: endoscopic ultrasound showed tumor capsule tightly adhered to the serosal layer
Postoperative pathology
The excised specimens were fixed with neutral formalin and sent for pathological examination and immunohistochemical staining. All tissues were stained with hematoxylin–eosin (HE) in the pathology department of our hospital. Patients with gastric stromal tumors were subjected to immunohistochemical methods to determine the expression of CD34, CD117, DOG-1, SMA, S-100, Desmin, and Ki-67 and the mitotic figure count to further clarify the pathological diagnosis and assess the degree of risk.
Research methods
General patient data were retrieved from the electronic medical record HIS system, which included sex, age, and other hospitalization information.
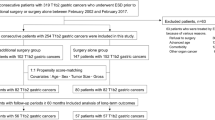
Other data collected herein included (1) the origin layer of the G-SMTs (superficial MP/deep MP); (2) the tumor location (fundus, greater/lesser curvature, anterior/posterior side); (3) the tumor size (the maximum cross-sectional diameter of the tumor was divided according to a size of ≥ 3 cm or < 3 cm); (4) ultrasonic echo characteristics (high/low, uniform/nonuniform); (5) growth pattern, namely, intraluminal growth versus exophytic growth (intraluminal growth means that > 50% of the tumor body protrudes into the lumen under EUS and/or CT evaluation, while exophytic growth means that > 50% of the tumor protrudes out of the lumen under EUS and/or CT evaluation); (6) boundary (regular or irregular); and (7) endoscopist experience level (endoscopists are considered to be experienced after performing more than 40 ESD cases independently, because adverse events related to ESD were found to be significantly reduced after 40 cases [31]).
The growth pattern was defined according to CT examination. Exophytic growth pattern accounted for over half of the SMT outside the radian of gastric wall. Otherwise, it was classified as intraluminal growth pattern. The tumor origin was defined according to EUS when tumor size was less than 2 cm (Fig. 3). However, for those G-SMTs larger than 2 cm, the muscularis propria was almost completely occupied by the tumor; therefore, tumor origin was decided based on CT. In these cases, the intraluminal tumor was classified as originating from the superficial-MP and the exophytic tumors were defined as deep-MP.
Statistical analysis
Data analysis was performed with SPSS 26.0 statistical software package (SPSS Inc, Chicago, Illinois, USA). The tumor characteristics of the case group and control group were compared, and the characteristics of the G-SMT patients in each group based on the success and failure of the operation were analyzed. The variables with P ≤ 0.1 in the univariate analysis were incorporated into the multivariate model. Multivariate logistic regression analysis was used to detect the relationship between surgical failure and G-SMT characteristics and to calculate the odds ratio and 95% confidence interval. The dependent variables were the success of ER and the failure of ER, and the independent variables were tumor lesion location, size, level of origin, irregular boundaries, ultrasonic echo characteristics and doctor experience. P < 0.05 was considered statistically significant.
Considering possible reverse causality, we conducted a sensitivity analysis by excluding subjects whose receive endoscopic resection during the first 2 years. Furthermore, we conducted further sensitivity analysis to investigate whether endoscopists' experience affect the risk of endoscopic resection.
Results
Flow chart
A total of 1095 tumors originating from the submucosa and muscularis propria were treated with ER (Fig. 1). Of those, 54 patients were excluded, 2 patients without sufficient information, and 52 patients were diagnosed with nonneoplastic lesions after ER. Therefore, 1041 patients were ultimately included in this case–control study.
Baseline characteristics of the subjects and clinicopathological characteristics of lesions
The baseline and clinicopathological characteristics of the study subjects and lesions are shown in Table 1. The mean age of the patients was 65.9 ± 11.3 years, and 62.6% were female. Among them, 1041 had G-SMTs, with 562 (54.0%) located in the fundus, 340 (32.9%) located in the greater/lesser curvature and 137 (13.1%) located on the anterior/posterior side. The mean diameter was 1.54 ± 1.04 cm, and most tumors had a diameter of ≤ 3 cm (87.7%). In the control group, the mean size was 1.50 ± 0.99 cm (range, 0.4 cm to 5 cm). In the research group, the median size was 3.30 ± 1.36 cm (range, 1.2 cm to 6 cm). A total of 985 patients were classified as having superficial MP (97.2%), and 128 were classified as having deep MP (12.3%) according to the relationship between tumor location and the MP layer by EUS examination. Tumor borders in 962 patients (92.4%) were irregular. The dominant growth pattern was intraluminal (94.6%). In addition, 97.2% of the procedures were performed by experienced endoscopists.
G-SMTs with endoscopic resection (ER) failure
ER failure occurred for 25 G-SMTs (Table 2). The main reasons for ER failure included serous membrane damage or adhesions (60%), exophytic growth (52%), intraoperative bleeding (52%), and a large tumor size (20%). There were 3 cases (12%) of tumors less than 2 cm in size and 17 cases (68%) of tumors larger than 3 cm. In one case, the tumor was located in the cavity and had a regular shape, but it was difficult to control intraoperative bleeding due to the abundance of tumor vessels. On the other hand, tumors that extensively adhere to extragastric structures can also cause ER failure. In addition, the actual tumor size during ER was found to larger than that evaluated prior to surgery in a few cases, especially for schwannoma, which was another reason for failure. ER failure occurred for all 6 cases of schwannoma and was related to unclear demarcation between the tumor and muscle, the large base of the tumor and serous membrane damage (Fig. 4). A total of 12 G-SMTs in the failure group had irregular borders, and 5 cases (41.7%) were schwannoma and 7 cases (58.3%) were GIST (Fig. 5).
Partial endoscopic manifestations of the failed endoscopic excision of SMTs. A: Female, 62 years. a-1 anterior wall of the gastric antrum body junction, 3.0 × 3.0 cm. a-2 reason for failure of endoscopic excision: adhesion between the tumor and gallbladder. Pathological: GIST, CD34( +), CD117(−), S-100(−), Low risk. B: Male, 47 years. b-1, Fundus fornix, 4.0 × 5.0 cm, with ulcer. b-2, reason for failure of endoscopic excision: bleeding. Pathological: GIST. CD34 ( +), CD117 ( +), DGO-1 (+), Low risk. C: Male, 47 years. c-1, Anterior wall of the gastric antrum, 2.0 × 2.0 cm, extracavity. c-2, reason for failure of endoscopic excision: unclear tumor boundary. Pathological: Schwannoma. D: Female, 77 years. d-1, Anterior wall of the gastric antrum, 2.0 × 2.0 cm, extracavity. d-2, reason for failure of endoscopic excision: bleeding and adhesion between the tumor and omentum. Pathological: GIST. CD34 ( +), CD117 ( +), Medium risk
Gastric submucosal tumors with irregular borders. a–d Female, 76 years, gastric fundus, 3.5 × 3.5 cm, with ulcer on surface and an irregular border, hypoechoic changes on EUS, Pathological: schwannoma. e–h male, 51 years, gastric fundus, 3.5 × 4.0 cm, with ulcer on surface and an irregular border, uneven echo on EUS. Pathological: GIST, mitotic image < 5/50HPF, CD34(+), CD117(+),DOG-1(+), Low risk
Risk factors for ER failure
We analyzed the risk factors for ER failure by univariate analysis. The results showed that the tumor growth pattern (OR = 35.671, 95% CI 15.110–84.211), size (OR = 18.053, 95% CI 7.610–42.827), layer of origin (OR = 33.630, 95% CI 12.371–91.422), irregular boundaries (OR = 13.075, 95% CI 5.742–29.769), echo uniformity (OR = 11.567, 95% CI 4.280–31.264) and endoscopist’s level of experience (OR = 5.192, 95% CI 1.462–18.444) were related to ER failure (all P < 0.05) (Table 3).
Binary logistic regression was performed on all of the above variables showing significant differences in univariate analysis, and the risk factors found to affect ER failure were determined through the regression pattern. The results of the multivariate analysis showed that independent risk factors for ER failure included tumors originating from a deep MP layer (OR = 14.42, 95% CI 4.47–46.52, P < 0.001), tumor size Φ > 3 cm (OR = 7.75, 95% CI 2.64–22.70, P < 0.001), exophytic growth pattern (OR = 4.98, 95% CI 1.62–15.29, P = 0.005), endoscopists with less experience (OR = 5.99, 95% CI 1.07–12.19, P = 0.042), and irregular borders (OR = 4.13, 95% CI 1.40–12.19, P = 0.010). Of these, the most significant independent risk factor was tumors originating from a deep MP layer, yielding an ER failure rate 14.422 times that of tumors originating from a superficial MP layer (Fig. 4).
ROC curve analysis of independent diagnostic value indicators
According to the result of multivariate Logistic regression analysis, the diagnostic value of risk factors for endoscopic resection failure was evaluated by constructing ROC curve. The result showed that combination of tumor size, layer of origin, dominant growth pattern, irregular borders and endoscopists’ experience indicators had high predictive value, with an AUC of 0.953 (95% CI 0.901–1.000). Separately, tumor size, layer of origin, dominant growth pattern and irregular border have moderate predictive value for endoscopic treatment, while the diagnostic performance of endoscopists’ experience was less satisfactory (0.5 < AUC ≤ 0.7). This model presented good goodness of fit by Hosmer and Lemeshow Test (P = 0.827).
Sensitivity analysis
Sensitivity analysis results showed that tumor size, tumor origin and growth pattern were similar to the original results, presenting good stable and reliable. However, irregular borders and endoscopists’ experience were different from the original results when excluding cases of the first 2 years of the study. In addition, in the other model, in condition of excluding the case study of inexperienced endoscopists, irregular boundaries was different from the original results (Table 4), indicating irregular borders and endoscopists’ experience were not stable enough. This result may be related to the insufficient events.
Discussion
G-SMTs are usually a diagnostic and therapeutic challenge. To date, the most reliable measures are EUS and CT; however, it is sometimes difficult to differentiate subepithelial from mesenchymal tumors and benign from malignant lesions using these modalities. The NCCN guidelines (2016) suggest that patients who have GISTs < 2 cm should undergo periodic endoscopy and/or EUS every 6 months, which will increase the cost of treatment, patient anxiety, and the risks associated with repeated endoscopic procedures [32]. ER is an endoscopic method used to remove G-SMTs from the stomach wall; this approach not only reduces trauma while providing a histological diagnosis but also allows for complete tumor resection. However, the endoscopic resection of SMTs should be performed only as part of a clinical trial in specialized centers due to the difficulty of operation [32].
When the tumor originates from the deep MP layer, the bottom is usually tightly connected with the muscle layer or serosa, and some tumors even adhere to the tissue outside the gastric wall [33]. Thus, it is quite possible to damage the serosa during tumor dissection, which can result in ER failure [34]. This study found that the ER failure rate increased by 14.422 times when the tumor originated from the deep MP layer, which is consistent with the results of previous studies. In addition, Białek found that patients with submucosal tumors derived from the muscle layer have a lower rate of complete resection with endoscopic mucosal resection (EMR) and have a higher risk of recurrence [35]. In our study, we found that tumors originating from the deep MP layer were more likely to grow extraluminally, thereby increasing difficulty of ER. In addition, Won Min showed that G-SMTs with extracavity growth are more likely to be GISTs [36]. As GISTs enlarge, exophytic GISTs may invade adjacent structures, such as the pancreas, colon, or diaphragm [37]. Therefore, endoscopists should always closely monitor such giant tumors.
There are few studies on the relationship between endoscopic resection failure and intraoperative bleeding. In the present retrospective case–control study, 25 patients with G-SMTs experienced ER failure, with intraoperative bleeding being the main reason for failure (52%). In this situation, large nutrient vessels of the G-SMT ruptured, and endoscopic visualization was impacted. Severe hemorrhage may result in uncontrollable abdominal hemorrhage because of defects in the gastric wall. Thus, these patients need to be immediately converted to surgery to manage bleeding, as described in previous reports [38]. ER may be a technically feasible, safe, less invasive and oncologically suitable option for GISTs less than 3 cm [11]. However, GISTs larger than 3 cm in diameter may need to be resected in slices, which could cause greater damage to the serosal layer, increasing not only the difficulty of the operation but also the risk of incomplete resection [39]. Although previous studies have shown that the risk of malignant transformation of GISTs larger than 3 cm is elevated [40, 41], in this study, even GISTs with a diameter of 6 cm were found to be pathologically low risk. On the other hand, some GISTs with a tumor diameter of 2 cm appeared to have a moderate risk of transformation, but none of the 25 G-SMT patients experiencing ER failure were found to have a high risk. Similar to previous reports, even for GISTs with a general malignant potential, the best tumor cutoff value related to tumor progression was found to be merely 1.4 cm [42], which is similar to the 1.7 cm value reported by Lachter et al. [43]. In addition, we found that 6 cases couldn’t remove from mouth after successful ER and need the assistance of laparoscopy to remove tumor through abdominal wall, among them 5 cases were larger than 3 cm.
Hoteya et al. reported that noncurative resection (72.0%) of G-SMTs with a maximum size of more than 3 cm did not result in local recurrence and metastasis, and the prognosis was good [44]. This is why patients are more willing to undergo endoscopic resection for larger G-SMTs. In this study, in cases exhibiting an extracavity growth pattern, most of the tumors measured by preoperative endoscopy in the failed cases were smaller than the true size after surgical resection. Therefore, it is necessary to comprehensively evaluate the true size of the tumor using a combination of endoscopy, EUS and CT. Tumors with irregular borders showed a trend of progressive change. In our study, a total of 12 G-SMTs in the failure group had irregular borders, and 5 cases (41.7%) were schwannoma and 7 cases (58.3%) were GIST. The tumor and the surrounding boundary were not clear during surgical separation in 2 patients, which increased the difficulty of ER and resulted in ER failure. Although 2 patients with GISTs in the ER failure group had regular borders, they had a moderate risk of malignancy. One of them had a tumor smaller than 5 cm but with a mitotic count of 6 (per 50 HPFs), and the other patient had a tumor that was larger in size (5 × 5 cm). EUS plays an important role in judging the origin of G-SMTs and can help to distinguish the tumor origin and growth pattern. Although a previous prospective study on the malignant risk of GIST found that tumor size and EUS characteristics cannot be used to predict the malignant risk of gastric GIST before surgery [40], our study showed that the ER failure rate of SMTs originating from the deep MP layer is much higher, indicating the important role of preoperative EUS. Regarding the tumor growth site, previous studies have shown that the endoscope can easily reach the lower part of the stomach for surgery, so it seems easier to stop interoperation bleeding using this approach [45]. Studies have also shown that the upper gastric muscularis propria is thinner, so it is more likely to perforate [39]. There are abundant omental attachments on the greater and lesser curvature sides of the stomach, but there is no omental attachment on the anterior and posterior walls and fundus. We subdivided the patients into three groups according to the tumor location and the presence of omental attachments, but we did not find a significant difference among the three groups in our study. This finding is based on real data from our center, and we look forward to conducting more research in this area in the future.
Physician experience is a risk factor for ER failure. In this study, ESD/EFTR was performed by experienced or inexperienced endoscopists under the supervision of experts. Thus, the incidence of unfavorable ESD/EFTR results may vary. Moreover, experienced endoscopists tend to treat larger or more complicated cases. This reflects the actual clinical significance of our research, and the results of this study provide a reference of the risk factors that should be considered by clinicians managing these patients.
To minimize the effect of reverse causality, we repeated all analyses after excluding study cases in the previous 2 years, the association of irregular borders and endoscopists’ experience with endoscopic resection failure changed in this model. In addition, irregular borders showed instability in the sensitivity analysis when excluding less experienced endoscopists. These findings suggest that irregular boundaries and endoscopists’ experience outcomes were less stable, this result may be ascribed to reverse causality or be related to less ER failure cases. In both models above, tumors origin, tumor size and growth pattern were presented good stability.
There are several shortcomings of this study that should be mentioned: (1) this was a retrospective study, so the included subjects were limited to patients undergoing ER (ESD and EFTR) at our hospital. In addition, the sample range was relatively small. (2) The accuracy of EUS diagnosis is highly dependent on the endoscopist, and the difference between observers represents an important challenge to be addressed. (3) The consideration of the influencing factors of the results was limited, and not all possible influencing factors were included in the statistical analysis. Therefore, it is necessary to expand the sample size and try to consider and analyze the factors that may cause bias. (4) Finally, our institution is the Jiangsu Provincial Tertiary Endoscopy Center, so 97.2% of endoscopic operations are performed by experienced endoscopists. Therefore, it is necessary to consider the abovementioned risk factors with regard to the endoscopist level of experience.
Conclusions
In this study, patients with gastric submucosal tumors treated by gastroscopy at our hospital were used as the research subjects to analyze the risk factors for ER failure. The analysis of single factors and a combination of multiple factors showed that tumors originating from the deep MP layer, a maximum tumor diameter Φ > 3 cm, an exophytic growth pattern, the experience level of the endoscopist, and irregular borders are independent risk factors for ER failure.
References
Hedenbro JL, Ekelund M, Wetterberg P. Endoscopic diagnosis of submucosal gastric lesions. The results after routine endoscopy. Surg Endosc. 1991;5(1):20–3.
Iorio N, Sawaya RA, Friedenberg FK. Review article: the biology, diagnosis and management of gastrointestinal stromal tumours. Aliment Pharmacol Ther. 2014;39(12):1376–86.
Ponsaing LG, Kiss K, Hansen MB. Classification of submucosal tumors in the gastrointestinal tract. World J Gastroenterol. 2007;13(24):3311–5.
Lee HL. Advances in the management of upper gastrointestinal subepithelial tumor: pathologic diagnosis using endoscopy without endoscopic ultrasound-guided biopsy. Clin Endosc. 2016;49(3):216–9.
Gu M, Ghafari S, Nguyen PT, Lin F. Cytologic diagnosis of gastrointestinal stromal tumors of the stomach by endoscopic ultrasound-guided fine-needle aspiration biopsy: cytomorphologic and immunohistochemical study of 12 cases. Diagn Cytopathol. 2001;25(6):343–50.
Nishida T, Kawai N, Yamaguchi S, Nishida Y. Submucosal tumors: comprehensive guide for the diagnosis and therapy of gastrointestinal submucosal tumors. Dig Endosc. 2013;25(5):479–89.
Demetri GD, von Mehren M, Antonescu CR, DeMatteo RP, Ganjoo KN, Maki RG, et al. NCCN Task Force report: update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw. 2010;8 Suppl 2(2):S1-41.
Cai MY, Martin Carreras-Presas F, Zhou PH. Endoscopic full-thickness resection for gastrointestinal submucosal tumors. Dig Endosc. 2018;30(Suppl 1):17–24.
Jeon HK, Kim GH, Lee BE, Park DY, Song GA, Kim DH, et al. Long-term outcome of endoscopic submucosal dissection is comparable to that of surgery for early gastric cancer: a propensity-matched analysis. Gastric Cancer. 2018;21(1):133–43.
Meng FS, Zhang ZH, Shan GD, Chen YP, Ji F. Endoscopic submucosal dissection for the treatment of large gastric submucosal tumors originating from the muscularis propria layer: a single center study. Z Gastroenterol. 2015;53(7):655–9.
Abe N, Takeuchi H, Ohki A, Hashimoto Y, Mori T, Sugiyama M. Comparison between endoscopic and laparoscopic removal of gastric submucosal tumor. Dig Endosc. 2018;30(Suppl 1):7–16.
Meng FS, Zhang ZH, Hong YY, Li DJ, Lin JQ, Chen X, et al. Comparison of endoscopic submucosal dissection and surgery for the treatment of gastric submucosal tumors originating from the muscularis propria layer: a single-center study (with video). Surg Endosc. 2016;30(11):5099–107.
Yu C, Liao G, Fan C, Yu J, Nie X, Yang S, et al. Long-term outcomes of endoscopic resection of gastric GISTs. Surg Endosc. 2017;31(11):4799–804.
Tashiro T, Hasegawa T, Omatsu M, Sekine S, Shimoda T, Katai H. Gastrointestinal stromal tumour of the stomach showing lymph node metastases. Histopathology. 2005;47(4):438–9.
Aparicio T, Boige V, Sabourin JC, Crenn P, Ducreux M, Le Cesne A, et al. Prognostic factors after surgery of primary resectable gastrointestinal stromal tumours. Eur J Surg Oncol. 2004;30(10):1098–103.
Yamao T, Shirao K, Ono H, Kondo H, Saito D, Yamaguchi H, et al. Risk factors for lymph node metastasis from intramucosal gastric carcinoma. Cancer. 1996;77(4):602–6.
Toyonaga T, Man-i M, East JE, Nishino E, Ono W, Hirooka T, et al. 1,635 Endoscopic submucosal dissection cases in the esophagus, stomach, and colorectum: complication rates and long-term outcomes. Surg Endosc. 2013;27(3):1000–8.
Goto O, Uraoka T, Horii J, Yahagi N. Expanding indications for ESD: submucosal disease (SMT/carcinoid tumors). Gastrointest Endosc Clin N Am. 2014;24(2):169–81.
Nagami Y, Ominami M, Sakai T, Maruyama H, Fukunaga S, Otani K, et al. Predictive factors for difficult endoscopic submucosal dissection for esophageal neoplasia including failure of en bloc resection or perforation. Surg Endosc. 2021;35(7):3361–9.
Zhang Y, Wang Z, Jin T, Li KQ, Hao K, Zhang W, et al. Hyperechoic demarcation line between a tumor and the muscularis propria layer as a marker for deciding the endoscopic treatment of gastric submucosal tumor. J Zhejiang Univ Sci B. 2017;18(8):707–16.
Aida K, Yoshikawa H, Mochizuki C, Mori A, Muto S, Fukuda T, et al. Clinicopathological features of gastric cancer detected by endoscopy as part of annual health checkup. J Gastroenterol Hepatol. 2008;23(4):632–7.
Kim J, Kim SG, Chung H, Lim JH, Choi JM, Park JY, et al. Clinical efficacy of endoscopic ultrasonography for decision of treatment strategy of gastric cancer. Surg Endosc. 2018;32(9):3789–97.
Kumano S, Murakami T, Kim T, Hori M, Iannaccone R, Nakata S, et al. T staging of gastric cancer: role of multi-detector row CT. Radiology. 2005;237(3):961–6.
An W, Sun PB, Gao J, Jiang F, Liu F, Chen J, et al. Endoscopic submucosal dissection for gastric gastrointestinal stromal tumors: a retrospective cohort study. Surg Endosc. 2017;31(11):4522–31.
Fukuda H, Uedo N, Shichijo S. Traction-assisted endoscopic full-thickness resection for extraluminal type gastrointestinal stromal tumor. Endosc Int Open. 2021;9(8):E1243–5.
Hu J, Liu W, Chen Z, Lin D, Su M, Lan P. A novel snare traction-assisted method during endoscopic resection for upper gastrointestinal submucosal tumors. J Laparoendosc Adv Surg Tech A. 2021;31(4):416–22.
Shi Q, Chen T, Zhong YS, Zhou PH, Ren Z, Xu MD, et al. Complete closure of large gastric defects after endoscopic full-thickness resection, using endoloop and metallic clip interrupted suture. Endoscopy. 2013;45(5):329–34.
Matsuda T, Fujii T, Emura F, Kozu T, Saito Y, Ikematsu H, et al. Complete closure of a large defect after EMR of a lateral spreading colorectal tumor when using a two-channel colonoscope. Gastrointest Endosc. 2004;60(5):836–8.
Chen Q, Yu M, Lei Y, Zhong C, Liu Z, Zhou X, et al. Efficacy and safety of endoscopic submucosal dissection for large gastric stromal tumors. Clin Res Hepatol Gastroenterol. 2020;44(1):90–100.
Xu MD, Cai MY, Zhou PH, Qin XY, Zhong YS, Chen WF, et al. Submucosal tunneling endoscopic resection: a new technique for treating upper GI submucosal tumors originating from the muscularis propria layer (with videos). Gastrointest Endosc. 2012;75(1):195–9.
Choi IJ, Kim CG, Chang HJ, Kim SG, Kook MC, Bae JM. The learning curve for EMR with circumferential mucosal incision in treating intramucosal gastric neoplasm. Gastrointest Endosc. 2005;62(6):860–5.
Nishida T, Blay JY, Hirota S, Kitagawa Y, Kang YK. The standard diagnosis, treatment, and follow-up of gastrointestinal stromal tumors based on guidelines. Gastric Cancer. 2016;19(1):3–14.
Chun SY, Kim KO, Park DS, Lee IJ, Park JW, Moon SH, et al. Endoscopic submucosal dissection as a treatment for gastric subepithelial tumors that originate from the muscularis propria layer: a preliminary analysis of appropriate indications. Surg Endosc. 2013;27(9):3271–9.
Liu BR, Song JT, Qu B, Wen JF, Yin JB, Liu W. Endoscopic muscularis dissection for upper gastrointestinal subepithelial tumors originating from the muscularis propria. Surg Endosc. 2012;26(11):3141–8.
Białek A, Wiechowska-Kozłowska A, Pertkiewicz J, Karpińska K, Marlicz W, Milkiewicz P, et al. Endoscopic submucosal dissection for the treatment of neoplastic lesions in the gastrointestinal tract. World J Gastroenterol. 2013;19(12):1953–61.
Min YW, Park HN, Min BH, Choi D, Kim KM, Kim S. Preoperative predictive factors for gastrointestinal stromal tumors: analysis of 375 surgically resected gastric subepithelial tumors. J Gastrointest Surg. 2015;19(4):631–8.
Kang HC, Menias CO, Gaballah AH, Shroff S, Taggart MW, Garg N, et al. Beyond the GIST: mesenchymal tumors of the stomach. Radiographics. 2013;33(6):1673–90.
Li QL, Yao LQ, Zhou PH, Xu MD, Chen SY, Zhong YS, et al. Submucosal tumors of the esophagogastric junction originating from the muscularis propria layer: a large study of endoscopic submucosal dissection (with video). Gastrointest Endosc. 2012;75(6):1153–8.
Ohta T, Ishihara R, Uedo N, Takeuchi Y, Nagai K, Matsui F, et al. Factors predicting perforation during endoscopic submucosal dissection for gastric cancer. Gastrointest Endosc. 2012;75(6):1159–65.
Kim MN, Kang SJ, Kim SG, Im JP, Kim JS, Jung HC, et al. Prediction of risk of malignancy of gastrointestinal stromal tumors by endoscopic ultrasonography. Gut Liver. 2013;7(6):642–7.
Chak A, Canto MI, Rösch T, Dittler HJ, Hawes RH, Tio TL, et al. Endosonographic differentiation of benign and malignant stromal cell tumors. Gastrointest Endosc. 1997;45(6):468–73.
Hu ML, Wu KL, Changchien CS, Chuah SK, Chiu YC. Endosonographic surveillance of 1–3 cm gastric submucosal tumors originating from muscularis propria. World J Gastroenterol. 2017;23(12):2194–200.
Lachter J, Bishara N, Rahimi E, Shiller M, Cohen H, Reshef R. EUS clarifies the natural history and ideal management of GISTs. Hepatogastroenterology. 2008;55(86–87):1653–6.
Hoteya S, Yamashita S, Kikuchi D, Nakamura M, Fujimoto A, Matsui A, et al. Endoscopic submucosal dissection for submucosal invasive gastric cancer and curability criteria. Dig Endosc. 2011;23(1):30–6.
Shimoda R, Iwakiri R, Sakata H, Ogata S, Kikkawa A, Ootani H, et al. Evaluation of endoscopic hemostasis with metallic hemoclips for bleeding gastric ulcer: comparison with endoscopic injection of absolute ethanol in a prospective, randomized study. Am J Gastroenterol. 2003;98(10):2198–202.
Acknowledgements
We would like to thank Shaowen Tang and Jin Liu for Statistical help.
Funding
This work was supported by a grant from National Natural Science Foundation of China (NO. 81873084), key project for Social Development in Jiangsu Province of China (NO. BE2020784) and the Medical Innovation Team of Jiangsu Province of China (NO. CXTDA2017033).
Author information
Authors and Affiliations
Contributions
The data sets used and analyzed during the current study are available from the corresponding author on reasonable request. Conception and design: CJ, LS; Development of methodology: YY, XZ; Acquisition of data: HC, XS, NT; Analysis and interpretation of data: WZ, YW, BY; Writing, review, and/or revision of the manuscript: CJ, YY, XZ; Study supervision: XL, GZ, HZ, LS, CJ.
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yuan, Y., Sun, L., Zhou, X. et al. Risk factors for the failure of endoscopic resection of gastric submucosal tumors: a long-term retrospective case–control study. Gastric Cancer 25, 929–942 (2022). https://doi.org/10.1007/s10120-022-01306-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-022-01306-9