Abstract
Background
Gastroesophageal junction (GEJ) cancers can be treated with equipoise using neoadjuvant chemoradiation (NACRT) or chemotherapy alone (NAC), but the comparative outcomes are unclear.
Methods
Patients with non-metastatic T2-4 or N1-3 GEJ adenocarcinoma who underwent definitive surgery and NAC or NACRT were selected from the National Cancer Database. The primary outcome was overall survival (OS). Multivariable regression and propensity score analysis were used to adjust for age, comorbidity, and other characteristics.
Results
We identified 2435 patients treated with NACRT and 648 patients treated with NAC. OS was not significantly different between NACRT and NAC (51% versus 54% at 3 years, respectively, P = 0.11). Extent of pathological downstaging (complete, partial/mixed, none) after NACRT or NAC was highly prognostic of survival. Patients with no response did equally poorly after either preoperative regimen, and NAC was significantly less likely than NACRT to produce any response (adjusted odds ratio 0.62, P < 0.0001). Rate of adjuvant chemotherapy usage was significantly lower after NACRT than after NAC (12% versus 34%, P < 0.0001). In patients with residual tumor and nodal disease, adjuvant chemotherapy was associated with higher OS after NACRT (adjusted hazard ratio 0.81, P = 0.05), but not after NAC. These results were further validated by propensity score analysis.
Conclusions
NACRT had similar survival to NAC despite superior pathological downstaging. Adjuvant chemotherapy is relatively underused after NACRT and warrants further study as a risk-adapted means to improve survival, especially in patients with larger burden of residual disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The combined incidence of esophageal and gastric cancers in the United States is projected to be approximately 44,000 for 2018, with nearly 27,000 deaths [1]. Worldwide, gastroesophageal cancers are the second leading cause of cancer mortality, behind only deaths from lung cancer and more than breast and prostate cancer deaths combined [2]. Most patients with operable and locally or regionally advanced disease require multimodality treatment. In randomized clinical trials of patients with resectable esophageal and gastroesophageal junction (GEJ) tumors, neoadjuvant chemoradiation [3,4,5,6,7,8] and pre/perioperative chemotherapy [8,9,10] are both superior to surgery alone. Likewise, pre/perioperative chemotherapy increases survival compared to surgery alone in trials of patients with gastric and GEJ cancer [10,11,12].
However, the optimal preoperative approach for upper gastrointestinal cancers remains unclear. To date, 3 completed randomized trials have directly compared neoadjuvant chemoradiation (NACRT) to neoadjuvant chemotherapy (NAC), finding that NACRT increases rates of pathological complete response and margin-negative resection, but not overall survival [13,14,15]. However, these trials were limited by poor accrual and non-contemporary treatment techniques. Furthermore, meta-analyses have yielded conflicting results, suggesting either no survival difference [7, 8] or an advantage to NACRT [3, 4]. At least 4 active clinical trials are currently comparing NACRT versus NAC in gastric and/or esophageal cancers, underscoring the critical importance of this question [16,17,18,19].
To address these uncertainties, we analyzed national patterns of care, pathological downstaging, and survival outcomes for patients in the United States with GEJ adenocarcinoma treated with NACRT or NAC and definitive surgical resection. Due to their location, GEJ tumors have been included in clinical trials of esophageal and gastric cancers, and thus may be treated using NACRT or NAC with equipoise. Therefore, GEJ cancers represent a unique opportunity to compare the different neoadjuvant approaches used in esophageal and gastric cancers.
Materials and methods
Data source
The National Cancer Database (NCDB) is a hospital-based registry sponsored by the American College of Surgeons and the American Cancer Society. It includes patient-level data from over 1500 Commission on Cancer-accredited facilities, capturing more than 70% of all incident cancers in the United States [20]. Reporting institutions are expected to have at least 90% patient follow-up over a 5-year period [20]. All data were de-identified, and this study was deemed exempt by the institutional review board. Our results have not been verified by the NCDB, and the NCDB is not responsible for the statistical validity of our conclusions.
Cohort identification
The NCDB gastric cancer registry was used, because it includes a variable [Site-Specific Factor 25 (SSF25)], indicating explicit involvement of the GEJ; the esophagus registry does not include this variable. The NCDB was queried for non-metastatic, clinical stage T2–4, and/or N1–3 GEJ adenocarcinoma. GEJ tumors were identified by ICD-O-3 primary site code C160 (gastric cardia), or ICD-O-3 primary site C161-162 (gastric fundus or body) with SSF25 of 010 (tumor located in cardia or GEJ), 020 (tumor involves esophagus or GEJ and distance of tumor midpoint to GEJ ≤ 5 cm), 040 (tumor involves esophagus or GEJ and distance to GEJ unknown), or 982 (primary site coded to C160). Although these cases were identified in the gastric cancer file, they were staged according to the esophagus/gastroesophageal junction schema, as indicated by the collaborative stage documentation regarding the values of SSF25 included in this study [21].
Inclusion criteria were diagnosis of GEJ adenocarcinoma between 2004 and 2014, receipt of definitive surgery within 180 days of diagnosis, and receipt of chemotherapy prior to surgery. The neoadjuvant chemotherapy (NAC) cohort comprised patients who received no radiation. The neoadjuvant chemoradiation (NACRT) cohort comprised patients who received external beam radiation prior to surgery to a dose of 30–60 Gy over 15–35 fractions. Patients were excluded if they were missing demographic (age, sex, race, and comorbidity), outcome (follow-up duration and vital status), or tumor data (clinical or pathological tumor and nodal stage). Figure 1 summarizes the cohort identification procedure.
Study variables and outcomes
The extent of pathological response was determined by comparing the pretreatment and pathological stages: complete response (CR) was defined as ypT0/ypTis and ypN0; partial/mixed response was defined as any downstaging (ypT < cT and/or ypN < cN) but not meeting CR criteria; and no response (NR) was defined as no downstaging (ypT ≥ cT and ypN ≥ cN). All other study variables were obtained directly from NCDB. Analyses involving adjuvant chemotherapy were restricted to patients diagnosed since 2006 when coding for postoperative chemotherapy became available. The primary outcome was overall survival, which was measured from the time of diagnosis. NCDB does not contain data regarding relapses or recurrence. Secondary outcomes were unplanned readmissions to the same facility within 30 days postoperatively, mortality within 90 days postoperatively, and margin-negative (R0) resection rate.
Statistical analysis
Baseline characteristics were compared using the Chi-squared or Wilcoxon rank-sum test. Median follow-up was calculated using the reverse Kaplan–Meier method [22]. Proportions of pathological response, adjuvant chemotherapy usage, 30-day readmission, and 90-day mortality were compared using the Chi-squared test. Linear trend of pathological complete response as a function of radiation dose was evaluated using the Cochran–Armitage test. Multivariable logistic regression was used to identify predictors of pathological response and receipt of adjuvant chemotherapy. Overall survival was estimated using the Kaplan–Meier method and compared using the log-rank test and Cox proportional hazards multivariable regression. We performed sensitivity analyses using 1:1 propensity score matching as previously described [22]. For analyses involving adjuvant chemotherapy, a landmark analysis was used that required at least 3 months of follow-up after surgery to address immortal time bias. MATLAB version R2018a (MathWorks, Inc.; Natick, MA, USA) was used for calculations. All tests were two-sided, and 0.05 was the threshold for statistical significance.
Results
Patient cohort
In total, 2435 patients were treated with NACRT, and 648 patients were treated with NAC. The relative usage of NAC generally increased from 2004 to 2009 when it reached a peak of 33%, followed by a consistent decline to 16% in 2014, which is the most recent available year of diagnosis (Supplemental Fig. 1). Baseline patient characteristics are listed in Table 1. Usage of NACRT versus NAC varied significantly among different geographic regions and between academic and non-academic centers. Median follow-up was 3.9 years.
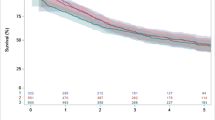
Survival and perioperative outcomes by neoadjuvant approach
Overall survival (OS) was not significantly different for NACRT versus NAC (51% and 54% at 3 years, respectively, P = 0.11). In multivariable analysis, OS modestly favored the NAC cohort [adjusted hazard ratio (HR) 0.88; 95% confidence interval (CI) 0.77–0.99, P = 0.04; Table 1]. Propensity score-matched analysis, in which 647 NAC patients were matched to 647 NACRT patients (Supplemental Table 1), yielded similar non-significant trends (univariable P = 0.12; adjusted HR 0.90, 95% CI 0.77–1.04, P = 0.15). Predictors for overall survival based on Cox regression are listed in Table 1.
The time from diagnosis to surgery was not significantly different between the NACRT and NAC cohorts (median 128.5 days versus 126 days; P = 0.08), and the survival results were unchanged whether survival was measured from time of diagnosis or time of surgery. There were no differences between NACRT and NAC for the rate of unplanned hospital readmissions within 30 days (6.5% versus 7.4%, P = 0.43) or mortality within 90 days (6.4% versus 6.2%, P = 0.86) of surgery. The R0 resection rate was higher for NACRT (93% versus 89%, P = 0.003).
Pathologic downstaging
Both the complete response rate and the overall response rate were significantly higher after NACRT than after NAC (complete: 15% versus 7%; overall: 61% versus 47%; P < 0.0001 for both; Table 2). The percentage of patients in each cohort stratified by post-neoadjuvant pathological tumor and nodal stage is listed in Supplemental Table 2. Predictors of pathological response are listed in Supplemental Table 3. NAC was significantly less likely to produce any response than NACRT [adjusted odds ratio (OR) 0.62; 95% CI 0.51–0.76, P < 0.0001).
Within the NACRT cohort, the overall response rate according to radiation dose was 55% for 30–40 Gy (n = 195), 60% for 40–50 Gy (n = 1,316), and 63% for 50–60 Gy (n = 924) (P = 0.025 for trend). Median overall survival was increased in patients who received at least 40 Gy preoperative radiation compared to patients who received less than 40 Gy preoperative radiation (37 versus 28 months), but this did not reach statistical significance (P = 0.08).
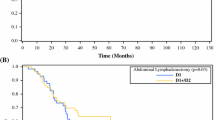
The extent of pathological response after both NACRT and NAC was significantly prognostic for survival. In the NACRT cohort, the 3-year OS for patients who had complete, partial/mixed, or no response was 62%, 55%, and 42%, respectively (P < 0.0001; Fig. 2a). In the NAC cohort, the 3-year OS for patients who had complete, partial/mixed, or no response was 91%, 64%, and 41%, respectively (P < 0.0001; Fig. 2b). Supplemental Fig. 2 shows a consolidated display of all OS curves according to the preoperative regimen and extent of pathological response, and Table 2 lists their adjusted hazard ratios.
Use and impact of adjuvant chemotherapy
Since NACRT had increased pathological downstaging but not survival compared to NAC, we analyzed the use of adjuvant chemotherapy. The rate of adjuvant chemotherapy use was significantly less after NACRT than after NAC (12% versus 34%, P < 0.0001), even after poor pathological response (Supplemental Fig. 3). Furthermore, use of adjuvant chemotherapy after NAC is increasing over time (consistent with a perioperative chemotherapy approach), nearing 40–50% in recent years (Supplemental Fig. 4), while use of adjuvant chemotherapy after NACRT has remained steady or slightly declined. Extent of pathological response was one of the strongest predictors of receiving adjuvant chemotherapy after NACRT, but was not predictive of adjuvant chemotherapy after NAC (Supplemental Tables 4, 5).
In the NACRT cohort, patients with residual disease in both tumor and lymph nodes had higher survival with adjuvant chemotherapy than without (3-year OS 47% versus 39% P = 0.05), which persisted in multivariable analysis (adjusted HR 0.81; 95% CI 0.65–1.00, P = 0.05). Yet, only 19% of such patients received adjuvant chemotherapy. Propensity score analysis, which included 171 patients per matched cohort (Supplemental Table 6), showed the same advantage for adjuvant chemotherapy (Fig. 3, univariable P = 0.02; adjusted HR 0.74, 95% CI 0.56–0.97, P = 0.03). By contrast, adjuvant chemotherapy in such patients after NAC was not associated with a survival advantage (univariable P = 0.41; adjusted HR 0.89, 95% CI 0.63–1.25, P = 0.50). In addition, patients without residual disease in both tumor and lymph nodes after NACRT (i.e., ypT0 and/or ypN0) did not have a survival benefit with adjuvant chemotherapy (univariable P = 0.26; adjusted HR 0.78, 95% CI 0.54–1.11, P = 0.17).
Discussion
In this national hospital-based study of neoadjuvant approaches for gastroesophageal (GEJ) adenocarcinomas, NACRT was much more commonly utilized, although use of NAC increased in the early to mid-2000s, perhaps due to publication of chemotherapy-only trials such as MAGIC (2006), and then declined in the later period of the study, which may reflect the publication of NACRT trials such as CALGB 9781 (2008) and CROSS (2012). However, we found no survival difference between neoadjuvant chemoradiotherapy (NACRT) and neoadjuvant chemotherapy (NAC), even though NACRT had significantly increased pathological downstaging and R0 resection rate. Interestingly, the NACRT cohort was significantly less likely to receive adjuvant chemotherapy, suggesting lower overall intensity of systemic therapy compared to the NAC cohort. Finally, we found that adjuvant chemotherapy use is associated with improved survival among patients who had poor pathological response following NACRT, but it is rarely used.
Our results are consistent with the findings of three completed randomized trials directly comparing NACRT and NAC [13,14,15]. Of these, the POET trial is most relevant to our study, as it focused exclusively on GEJ tumors, and it was the only one to report a near-significant OS trend favoring NACRT (40% versus 24% at 5 years; P = 0.055), although all three trials were limited by sample size. POET also showed that NACRT increased the pathological complete response rate (16% versus 2%; P = 0.03) and decreased the incidence of local failure (18% versus 38%; P = 0.04), despite using a radiation dose (30 Gy) that is widely considered to be suboptimal. Notably, the two treatment arms in POET delivered the same intensity of full-dose preoperative chemotherapy, whereas patients treated with NACRT in the United States are typically given lower intensity chemotherapy compared to patients receiving preoperative or perioperative chemotherapy without radiation [23].
Our work is also consistent with several single and multi-institution retrospective series, nearly all of which have demonstrated increased pathological complete response and/or R0 resection with NACRT, but no difference in disease-free or overall survival [24,25,26]. The largest series included 608 propensity score-matched patients with stage II–III esophageal/GEJ adenocarcinoma from 10 European centers treated with NACRT (CROSS regimen) or NAC (MAGIC, OEO2, or OEO5 regimens) [24]. NACRT was associated with increased ypT0 stage (27% versus 5%, P < 0.001), ypN0 stage (63% versus 32%, P < 0.001), and R0 resection (92% versus 78%, P < 0.001), but no difference in 3-year OS (58% versus 53%, P = 0.39) or disease-free survival (53% versus 49%, P = 0.44). On the other hand, one of the only retrospective studies to show a survival difference was a single-institution analysis of 157 patients enrolled sequentially onto phase II–III trials of NACRT or NAC, with 3-year OS favoring NACRT (48% versus 29%, P = 0.04) [27], similar to the survival results from the POET trial.
We showed that NACRT was associated with significantly higher rates of pathological response than NAC. Pathological complete response for esophageal/GEJ cancers after NACRT has been associated with a two-to-threefold higher survival, or approximately 30% absolute OS benefit [28]. Similarly, pathological complete response after neoadjuvant treatment of gastric cancer is prognostic [29]. Most prior studies have classified pathological response in a binary fashion as complete or incomplete. Here, we established a three-tiered classification system in which incomplete responses are further stratified as partial/mixed response or no response. Our classification scheme was highly prognostic for survival after either NACRT or NAC, can be applied easily to existing patients and data sets, and warrants further validation as a useful predictive tool for clinical and research use.
To understand why the increased pathological downstaging of NACRT did not translate into increased OS, we found that adjuvant chemotherapy was used rarely after NACRT (12% overall). By contrast, adjuvant chemotherapy use after NAC was 40–50% in recent years, similar to the therapy completion rates in MAGIC and FLOT4-AIO [11, 12], indicating stark differences in overall intensity of systemic therapy between the NAC and NACRT cohorts. Interestingly, we identified a population of patients with larger burden of residual disease after NACRT that had a survival benefit associated with adjuvant chemotherapy, yet less than 20% of such patients received adjuvant chemotherapy. Thus, we speculate that the lower intensity of systemic treatment in the NACRT cohort leads to lesser treatment of micrometastatic disease and has limited the locoregional benefit of NACRT. In the United States, patients treated with NACRT typically receive less intensive doses of chemotherapy compared to patients treated with preoperative or perioperative chemotherapy alone, and there are no standard guidelines for administering additional (adjuvant) chemotherapy after NACRT [23, 30]. The crucial importance of systemic therapy intensity for gastroesophageal cancer was recently highlighted by the FLOT4-AIO trial, in which survival was improved by perioperative FLOT versus ECF/ECX chemotherapy [11]. Our results are bolstered by other retrospective studies, suggesting a benefit of adjuvant chemotherapy after NACRT [30], especially with macroscopic residual disease [31].
Furthermore, we showed that equivalent responses after NACRT or NAC can have very different prognostic significance. For example, survival after a complete response to NAC was superior to survival after a complete response to NACRT (which, in turn, was similar to survival after a mixed/partial response to NAC). Since NAC is a less locally intensive therapy than NACRT, a tumor that responds to the same extent after NAC likely reflects a more favorable, treatment-responsive biology. Thus, not all responses are alike: its value as a surrogate endpoint for survival may vary based on the treatment. Our work suggests that comparing response rates between regimens of inherently different intensity must be done carefully, as the treatment regimen should be considered when interpreting the prognostic significance of response. In addition, the increased pathological response rate (and presumed locoregional benefit) of NACRT may be offset by increased distant recurrences due to lower intensity of systemic treatment.
To minimize selection bias inherent with retrospective studies, we limited our analyses to GEJ tumors, because they are commonly treated with both neoadjuvant chemoradiotherapy and chemotherapy alone given their inclusion in trials of both esophageal and gastric cancers. However, our findings might also extend to non-GEJ tumors of the esophagus and stomach. Most cases of operable esophageal/GEJ cancer in the United States are treated with NACRT [National Comprehensive Cancer Network (NCCN) category 1] [23], but national guidelines also list pre/perioperative chemotherapy as an option for distal esophageal and GEJ tumors, and this approach is standard for esophageal cancer in some European countries [32]. For non-cardia gastric cancer, perioperative chemotherapy is preferred (NCCN category 1). NACRT for gastric cancers has not been studied in a completed phase III trial, but has been studied in the phase II setting [33] and is NCCN category 2B. Currently, at least 4 active trials are comparing NACRT to NAC: 2 in esophageal/GEJ cancers (ESOPEC, Neo-AEGIS) [16, 17] and 2 in gastric/GEJ cancers (TOPGEAR, CRITICS-II) [18, 19].
The strengths of our study include its national scope, the specific focus on GEJ tumors given that they can be treated with NAC or NACRT with equipoise, and use of multivariable and propensity score analyses to address confounding. Our results should also be considered in the context of its limitations, which reflect the intrinsic aspects of the NCDB. The primary limitation is the retrospective design and possibility of residual selection bias; our results, while provocative, remain hypothesis-generating. In addition, the NCDB lacks data regarding relapses/recurrence, and sites of failure (e.g., local versus distant) are not available. We surmise that the NACRT cohort had decreased locoregional relapse, as evidenced by increased pathological response, increased margin-negative resection, and prior results of the POET trial, but also increased distant recurrence due to lower intensity of systemic therapy. However, this remains speculative, and patterns of recurrence in the ongoing trials comparing NACRT versus NAC will be of particular interest, especially as only one (TOPGEAR) includes the planned use of adjuvant chemotherapy in the NACRT arm.
Another limitation is that the NCDB does not contain information related to specific chemotherapy agents or doses. Thus, the lower intensity of systemic therapy in the NACRT cohort was inferred from the low utilization of adjuvant chemotherapy, as well as standard practices in the United States. This study does not compare different surgical procedures (e.g., partial versus total gastrectomy), since surgical decision-making may depend at least partially on the clinical response to neoadjuvant therapy and the intraoperative findings. The levels of lymphadenectomy (e.g., D1 versus D2 dissection) are also not available in the NCDB. Finally, the extent of staging studies (such as use of diagnostic laparoscopy, positron emission tomography [PET], or endoscopic ultrasound [EUS]) is not available, and such studies can be operator-dependent. Pretreatment workup is crucial towards accurate clinical staging, which was the basis for our analysis of pathological response, as well as ensuring correct treatment decision making. While this is a potential for misclassification of stage, it is unlikely that one cohort (NACRT or NAC) was consistently under- or over-staged at a national level to explain the highly significant differences in pathological response observed between NACRT and NAC. Ultimately, our study embodies real-world patterns of care across the United States in terms of workup, chemotherapy administration, and surgical practices.
In summary, NACRT was associated with increased pathological downstaging and margin-negative resection, but not improved survival, compared to NAC. This indicates a pressing need for further research, both to determine the true added benefit of preoperative radiation through adequately powered randomized trials and to find ways to optimize outcomes after NACRT. We contend that adjuvant chemotherapy warrants further investigation as a risk-adapted means of treatment intensification to improve survival after NACRT, especially in patients with larger burden of residual disease.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin [Internet]. [cited 2018 Oct 20];0. Available from: https://onlinelibrary.wiley.com/doi/abs/10.3322/caac.21492
Pasquali S, Yim G, Vohra RS, Mocellin S, Nyanhongo D, Marriott P, et al. Survival After neoadjuvant and adjuvant treatments compared to surgery alone for resectable esophageal carcinoma: a network meta-analysis. Ann Surg. 2017;265:481–91.
Zhao X, Ren Y, Hu Y, Cui N, Wang X, Cui Y. Neoadjuvant chemotherapy versus neoadjuvant chemoradiotherapy for cancer of the esophagus or the gastroesophageal junction: a meta-analysis based on clinical trials. PLoS ONE. 2018;13:e0202185.
Shapiro J, van Lanschot JJB, Hulshof MCCM, van Hagen P, van Berge Henegouwen MI, Wijnhoven BPL, et al. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial. Lancet Oncol. 2015;16:1090–8.
Tepper J, Krasna MJ, Niedzwiecki D, Hollis D, Reed CE, Goldberg R, et al. Phase III trial of trimodality therapy with cisplatin, fluorouracil, radiotherapy, and surgery compared with surgery alone for esophageal cancer: CALGB 9781. J Clin Oncol Off J Am Soc Clin Oncol. 2008;26:1086–92.
Fu T, Bu Z-D, Li Z-Y, Zhang L-H, Wu X-J, Wu A-W, et al. Neoadjuvant chemoradiation therapy for resectable esophago-gastric adenocarcinoma: a meta-analysis of randomized clinical trials. BMC Cancer. 2015;15:322.
Sjoquist KM, Burmeister BH, Smithers BM, Zalcberg JR, Simes RJ, Barbour A, et al. Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: an updated meta-analysis. Lancet Oncol. 2011;12:681–92.
Kidane B, Coughlin S, Vogt K, Malthaner R. Preoperative chemotherapy for resectable thoracic esophageal cancer. Cochrane Database Syst Rev. 2015;CD001556.
Ychou M, Boige V, Pignon J-P, Conroy T, Bouché O, Lebreton G, et al. Perioperative chemotherapy compared with surgery alone for resectable gastroesophageal adenocarcinoma: an FNCLCC and FFCD multicenter phase III trial. J Clin Oncol Off J Am Soc Clin Oncol. 2011;29:1715–21.
Al-Batran S-E, Homann N, Pauligk C, Goetze TO, Meiler J, Kasper S, et al. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): a randomised, phase 2/3 trial. Lancet Lond Engl. 2019;393:1948–57.
Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJH, Nicolson M, et al. Perioperative Chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355:11–20.
Stahl M, Walz MK, Stuschke M, Lehmann N, Meyer H-J, Riera-Knorrenschild J, et al. Phase III comparison of preoperative chemotherapy compared with chemoradiotherapy in patients with locally advanced adenocarcinoma of the esophagogastric junction. J Clin Oncol Off J Am Soc Clin Oncol. 2009;27:851–6.
Burmeister BH, Thomas JM, Burmeister EA, Walpole ET, Harvey JA, Thomson DB, et al. Is concurrent radiation therapy required in patients receiving preoperative chemotherapy for adenocarcinoma of the oesophagus? A randomised phase II trial. Eur J Cancer Oxf Engl. 1990;2011(47):354–60.
von Döbeln GA, Klevebro F, Jacobsen A-B, Johannessen H-O, Nielsen NH, Johnsen G, et al. Neoadjuvant chemotherapy versus neoadjuvant chemoradiotherapy for cancer of the esophagus or gastroesophageal junction: long-term results of a randomized clinical trial. Dis Esophagus Off J Int Soc Dis Esophagus. 2018. https://doi.org/10.1093/dote/doy078.
Hoeppner J, Lordick F, Brunner T, Glatz T, Bronsert P, Röthling N, et al. ESOPEC: prospective randomized controlled multicenter phase III trial comparing perioperative chemotherapy (FLOT protocol) to neoadjuvant chemoradiation (CROSS protocol) in patients with adenocarcinoma of the esophagus (NCT02509286). BMC Cancer. 2016;16:503.
Reynolds J, Preston S, O’Neill B, Baeksgaard L, Griffin S, Mariette C, et al. ICORG 10–14: NEO adjuvant trial in adenocarcinoma of the oEsophagus and oesophago Gastric junction international study (Neo-AEGIS). BMC Cancer. 2017;17:401.
Leong T, Smithers BM, Haustermans K, Michael M, Gebski V, Miller D, et al. TOPGEAR: A randomized, phase III Trial of perioperative ecf chemotherapy with or without preoperative chemoradiation for resectable gastric cancer: Interim results from an international, intergroup trial of the AGITG, TROG. EORTC and CCTG. Ann Surg Oncol. 2017;24:2252–8.
Slagter AE, Jansen EPM, van Laarhoven HWM, van Sandick JW, van Grieken NCT, Sikorska K, et al. CRITICS-II: a multicentre randomised phase II trial of neo-adjuvant chemotherapy followed by surgery versus neo-adjuvant chemotherapy and subsequent chemoradiotherapy followed by surgery versus neo-adjuvant chemoradiotherapy followed by surgery in resectable gastric cancer. BMC Cancer [Internet]. 2018 [cited 2018 Oct 18];18. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6131797/
Boffa DJ, Rosen JE, Mallin K, Loomis A, Gay G, Palis B, et al. Using the National cancer database for outcomes research: a review. JAMA Oncol. 2017;3:1722–8.
Stomach-CS Site-Specific Factor 25 [Internet]. [cited 2019 May 10]. Available from: https://web2.facs.org/cstage0205/stomach/Stomach_spv.html
Xiang M, Nguyen PL. Significant association of brachytherapy boost with reduced prostate cancer-specific mortality in contemporary patients with localized, unfavorable-risk prostate cancer. Brachytherapy. 2015;14:773–80.
National Comprehensive Cancer Network. Esophageal and Esophagogastric Junction Cancers (Version 2.2018) [Internet]. [cited 2018 Oct 21]. Available from: https://www.nccn.org/professionals/physician_gls/pdf/esophageal.pdf
Markar SR, Noordman BJ, Mackenzie H, Findlay JM, Boshier PR, Ni M, et al. Multimodality treatment for esophageal adenocarcinoma: multi-center propensity-score matched study. Ann Oncol Off J Eur Soc Med Oncol. 2017;28:519–27.
Anderegg MCJ, van der Sluis PC, Ruurda JP, Gisbertz SS, Hulshof MCCM, van Vulpen M, et al. Preoperative Chemoradiotherapy versus perioperative chemotherapy for patients with resectable esophageal or gastroesophageal junction adenocarcinoma. Ann Surg Oncol. 2017;24:2282–90.
Visser E, Edholm D, Smithers BM, Thomson IG, Burmeister BH, Walpole ET, et al. Neoadjuvant chemotherapy or chemoradiotherapy for adenocarcinoma of the esophagus. J Surg Oncol. 2018;117:1687–96.
Swisher SG, Hofstetter W, Komaki R, Correa AM, Erasmus J, Lee JH, et al. Improved long-term outcome with chemoradiotherapy strategies in esophageal cancer. Ann Thorac Surg. 2010;90:892–8 (Discussion 898–899).
Scheer RV, Fakiris AJ, Johnstone PAS. Quantifying the benefit of a pathologic complete response after neoadjuvant chemoradiotherapy in the treatment of esophageal cancer. Int J Radiat Oncol Biol Phys. 2011;80:996–1001.
Ajani JA, Mansfield PF, Crane CH, Wu TT, Lunagomez S, Lynch PM, et al. Paclitaxel-based chemoradiotherapy in localized gastric carcinoma: degree of pathologic response and not clinical parameters dictated patient outcome. J Clin Oncol Off J Am Soc Clin Oncol. 2005;23:1237–44.
Mokdad AA, Yopp AC, Polanco PM, Mansour JC, Reznik SI, Heitjan DF, et al. Adjuvant Chemotherapy vs postoperative observation following preoperative chemoradiotherapy and resection in gastroesophageal cancer: a propensity score-matched analysis. JAMA Oncol. 2018;4:31–8.
Kim GJ, Koshy M, Hanlon AL, Horiba MN, Edelman MJ, Burrows WM, et al. The Benefit of Chemotherapy in esophageal cancer patients with residual disease after trimodality therapy. Am J Clin Oncol. 2016;39:136–41.
Messager M, de Steur WO, van Sandick JW, Reynolds J, Pera M, Mariette C, et al. Variations among five European countries for curative treatment of resectable oesophageal and gastric cancer: a survey from the EURECCA Upper GI Group (European Registration of Cancer Care). Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol. 2016;42:116–22.
Ajani JA, Winter K, Okawara GS, Donohue JH, Pisters PWT, Crane CH, et al. Phase II trial of preoperative chemoradiation in patients with localized gastric adenocarcinoma (RTOG 9904): quality of combined modality therapy and pathologic response. J Clin Oncol Off J Am Soc Clin Oncol. 2006;24:3953–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Xiang, M., Chang, D.T., Heestand, G.M. et al. Survival after neoadjuvant approaches to gastroesophageal junction cancer. Gastric Cancer 23, 175–183 (2020). https://doi.org/10.1007/s10120-019-00980-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-019-00980-6