Abstract
Aim
The aim of this study was to determine prognostic factors in patients treated with second-line therapy (L2) for locally advanced or metastatic gastric and gastro-esophageal junction (GEJ) adenocarcinoma in a randomized phase III study with predefined L2.
Methods
In the FFCD-0307 study, patients were randomly assigned to receive in L1 either epirubicin, cisplatin, and capecitabine (ECX arm) or fluorouracil, leucovorin, and irinotecan (FOLFIRI arm). L2 treatment was predefined (FOLFIRI for the ECX arm and ECX for the FOLFIRI arm). Chi square tests were used to compare the characteristics of patients treated in L2 with those of patients who did not receive L2. Prognostic factors in L2 for progression-free survival (PFS) and overall survival (OS) were analyzed using a Cox model.
Results
Among 416 patients included, 101/209 (48.3%) patients in the ECX arm received FOLFIRI in L2, and 81/207 (39.1%) patients in the FOLFIRI arm received ECX in L2. Patients treated in L2, compared with those who only received L1 had : a better ECOG score (0–1: 90.4% versus 79.7%; p = 0.0002), more frequent GEJ localization (40.8% versus 27.6%; p = 0.005), and lower platelet count (median: 298000 versus 335000/mm3; p = 0.02). In multivariate analyses, age < 60 years at diagnosis (HR 1.49, 95% CI 1.09–2.03, p = 0.013) and ECOG score 2 before L2 (HR 2.62, 95% CI 1.41–4.84, p = 0.005) were the only significant poor prognostic factors for OS.
Conclusion
Age ≥ 60 years at diagnosis and ECOG score 0/1 before L2 were the only favorable prognostic factors for OS.
Similar content being viewed by others
Introduction
Worldwide, gastric cancer is the third leading cause of cancer-related mortality. Though the incidence has decreased over the last 20 years, the prognosis remains poor [1]. In patients with advanced or metastatic disease, 5-year overall survival remains less than 5%. In first-line, chemotherapy, regimens can improve overall survival. Doublets or triplet chemotherapy regimen, and trastuzumab in patients with human epidermal growth factor receptor (HER)-2 positive tumors, have demonstrated clinical benefits on overall survival and quality of life [2,3,4,5]. Other studies have also demonstrated the potential benefits on overall survival of a second-line treatment, with irinotecan, taxanes, ramucirumab alone or combined with paclitaxel, and more recently nivolumab in third-line therapy and beyond [6,7,8,9,10,11]. In published clinical trials evaluating first-line treatments without pre-planned second line, the percentage of patients receiving a second line, when reported, is heterogenous, e.g., 14% in the REAL-2 trial, 45% in the ToGA trial, 75% in the SPIRITS trial; with a higher proportion in Asian trials compared to non-Asian trials [2,3,4]. Thus, few data are available to help the selection of patients for a second-line treatment. The aim of our study was to evaluate the prognostic factors in patients who received second-line therapy in a randomized prospective trial in which the first- and second-line treatments were planned [12].
Materials and methods
Patients and study design
Patients from the FFCD-0307 trial had locally advanced or metastatic gastric or gastro-esophageal junction (GEJ) locally advanced or metastatic adenocarcinoma and were randomly assigned (1:1) to receive either epirubicin, cisplatin, and capecitabine (ECX) chemotherapy in the first line (ECX arm) with a predefined second-line therapy with fluorouracil, leucovorin, and irinotecan (FOLFIRI) or to receive FOLFIRI in the first line (FOLFIRI arm) with a predefined ECX second-line therapy. Other inclusion criteria were: age 18 years or older, measurable and/or assessable lesions according to RECIST criteria, WHO performance score (PS) ≤ 2, ability to take oral medications, no previous palliative chemotherapy (≥ 6 months from adjuvant chemotherapy was allowed), ≥ 3 weeks from previous radiotherapy, sufficient bone marrow function, creatininemia ≤ 110 μmol/l, and bilirubinemia ≤ 35 μmol/l.
Treatment and evaluation
The ECX regimen consisted of epirubicin 50 mg/m2 [15-min intravenous (IV) infusion] plus cisplatin 60 mg/m2 (1-h IV infusion) on day 1 followed by oral capecitabine 1 g/m2 twice per day from day 2 to day 15 every 3 weeks; the maximum authorized cumulative dose of epirubicin was 900 mg/m2. The FOLFIRI regimen consisted of irinotecan 180 mg/m2 (90-min IV infusion) and leucovorin 400 mg/m2 (2-h IV infusion) followed by a fluorouracil 400 mg/m2 IV bolus and then fluorouracil 2400 mg/m2 as a 46-h continuous infusion every 2 weeks.
Tumor response was evaluated by investigators and classified according to RECIST criteria. CT scans were performed before the start of treatment and then every 8 weeks until disease progression for each treatment line and in each arm.
Statistical analyses
Progression-free survival (PFS) was defined as the time from the start of the second line to the first progression or death (all causes). Patients alive without progression were censored at the last follow-up. Overall survival (OS) was defined as the time between the start of the second line and death (all causes). The disease control rate (DCR) was defined as the proportion of patients with a complete or partial response, or stable diseases during the second line according to RECIST criteria.
Qualitative and continuous variables were described using the usual descriptive statistics: numbers and percentages and medians with min–max, respectively. Comparison of baseline characteristics of the two arms was made with the χ2 test or nonparametric Wilcoxon test, depending on the type and distribution of variables.
Survival analyses (OS, PFS) were done using the Kaplan–Meier method and described using medians with 95% two-sided confidence intervals (95% CI). Cox models were used to estimate hazard ratios (HR) and logistic regressions were performed for DCR. All variables significant at 10% in univariate analyses were included in the multivariate analyses. Two multivariate models were made: the first one with factors assessed before the start of first-line therapy and the second one with factors assessed before the start of second-line therapy. Analyses were performed using SAS software 9.4 (SAS Institute, Cary, NC).
Results
Probability of receiving a second-line chemotherapy according to baseline characteristics
Among the 416 patients included in the FFCD-0307 trial, 182 patients received the preplanned second-line chemotherapy, 101/209 (48.3%) patients in the ECX arm received FOLFIRI in L2, and 81/207 (39.1%) of patients in the FOLFIRI arm received ECX in L2. No other second-line regimen was administered.
The baseline (before first line) clinical characteristics of patients are presented in Table 1. At baseline, patients with GEJ tumors (versus gastric tumors, p = 0.005), ECOG 0–1 (versus ECOG 2, p = 0.0002) were more likely to receive the second-line chemotherapy. There was no significant difference according to the first-line regimen (55.5% ECX, 44.5% FOLFIRI, p = 0.06).
The baseline biological results were analyzed. The group of patients who received the second-line treatment had a lower baseline-platelet count (median 298,000/mm3 versus 335,000/mm3, p = 0.02). There were no significant differences according to the hemoglobin and neutrophils counts, and to serum levels of bilirubin, alkaline phosphatase, carcinoembryonic antigen (CEA) and carbohydrate antigen 19.9 (CA19.9) (Table 2).
Prognostic factors for disease control from the start of second line
The disease control rate (DCR) was assessable in 150 patients. The DCR was 45/83 (54.2%) for patients treated with FOLFIRI L2 versus 31/67 (46.3%) for patients treated with ECX L2.
In univariate analysis, the neutrophil count < 5000/mm3 (p = 0.028) and ECOG score 0/1 before L2 (p = 0.008) were the only significant good prognostic factor (Table 3). There was no correlation between the response rates in first and second lines (p (Fisher) = 0.156 for patients treated with FOLFIRI L2, p (Fisher) = 0.687 for patients treated with ECX L2).
Prognostic factors for PFS from the start of the second-line therapy
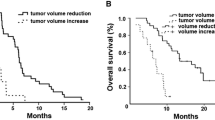
Median PFS was 2.8 months with FOLFIRI L2 and 2.1 months with ECX L2 (Fig. 1a). In univariate analysis, age ≥ 60 years and ECOG score 0/1 before L2 were the only significant good prognostic factors (Table 4).
Prognostic factors for OS from the start of second-line therapy
The median OS was 5.4 months with FOLFIRI L2 and 4.8 months with ECX L2 (Fig. 1b). The median OS in the third quartile (subgroup of longer survivors), was 10.48 months (95% CI 8.84–12.39) for FOLFIRI in L2, and 8.02 months (95% CI 6.80–10.25) for ECX in L2. In univariate analysis, platelet count < 300,000/mm3 (p = 0.025), age ≥ 60 years (p = 0.008) and ECOG score before L2 were the only significant good prognostic factors (Table 5). In multivariate analyses, in the first model, age < 60 years at diagnosis (versus ≥ 60 years) (HR 1.49, 95% CI 1.09–2.03, p = 0.013) and in the second model ECOG score ≥ 2 before L2 (HR 2.62, 95% CI 1.41–4.84, p = 0.005) were the only significant poor prognostic factors (Table 6).
Discussion
Second-line treatment is seldom administered and results in all studies in limited efficacy on tumor growth. In the FFCD-0307 trial, only 43% of patients received a second-line therapy. From baseline, patients more likely to receive this second line more frequently had GEJ tumors and an ECOG score 0–1. Nonetheless, the clinical benefits were still limited, with median overall survival following the second line of around 5 months. For the second line, age ≥ 60 years and ECOG score 0/1 were the only significant good prognostic factors for OS in multivariate analyses.
The proportion of patients receiving a second line was closer to that observed in the ToGA trial (45%), than in the REAL-2 trial (14%), which illustrates the differences in clinical approaches in different centers [3, 5]. A planned second-line therapy in the FFCD-0307 may have favored the prescription of the second-line therapy. Median PFS (2.8 months with FOLFIRI L2 and 2.1 months with ECX L2) are in the same range as other published data: 2.3 months with irinotecan and 3.6 months with docetaxel [13], 2.1 months with ramucirumab alone in the REGARD trial [9], 2.9 months with paclitaxel and 4.4 months with paclitaxel combined with ramucirumab in the RAINBOW trial [10]. Median OS was 5.4 months with FOLFIRI L2 and 4.8 months with ECX L2. In other trials, median OS was 4–8.4 months with irinotecan and 9.5 months with docetaxel, 5.3 months with ramucirumab alone in the REGARD trial, 7.4 months with paclitaxel and 9.4 months with paclitaxel combined with ramucirumab in the RAINBOW trial.
Other studies have investigated prognostic factors in patients with metastatic gastric adenocarcinoma treated in the first or second line. In a large retrospective analysis, ECOG ≥ 2, bone metastases, ascitis, alkaline phosphatase > 85UI/l, albumin < 3.6 g/dl and no resected primary tumor were identified as poor prognostic factors for OS for patients receiving first-line chemotherapy [14]. In a pooled analysis of three randomized trials, ECOG ≥ 2, liver metastases, peritoneal metastases, and alkaline phosphatase ≥ 100UI/l were poor prognostic factors [15]. In second-line therapy, a retrospective analysis identified ECOG ≥ 2, hemoglobin ≤ 11.5 g/dl, CEA > 50 ng/ml, ≥ 3 metastatic sites, and time to progression ≤ 6 months under first-line treatment as independent poor prognostic factors [16]. Another retrospective study identified the following as prognostic factors in second-line chemotherapy: the PFS in the first-line chemotherapy, the performance status, serum levels of albumin and alkaline phosphatase and no resected primary tumor [17]. In a retrospective study that included 126 patients, a good performance status, a higher hemoglobin level and a longer time to progression in the first-line chemotherapy were good prognostic factors in the second-line chemotherapy [18]. More recently, a large retrospective multicenter analysis included 868 patients treated with second-line therapy. Median PFS was 2.8 months and median OS was 5.6 months. Patients received various treatments, but mostly single-agents or doublets with fluoropyrimidines, irinotecan, and taxanes. The ECOG score, an LDH level > 480UI/l, a neutrophil/lymphocyte ratio ≥ 2.7 and PFS ≤ 6.8 months in the first line were the four independent factors for poor OS [19]. In our study, PFS in L1 was not a prognostic factor (HR 0.81 95% IC 0.51–1.29). The relative efficacy of the two investigated regimen may partly explain this result, an efficient second-line therapy may be able to counterbalance a short PFS in L1 in patients in good general condition. Age (≥ 60 years or as a continuous variable) was an independent good prognostic factor for PFS and OS. In a meta-analysis comparing elderly with young patients, elderly patients had more diffuse-type cancer, but better 5-year OS [20]. There are few data in the literature about age as a prognostic factor in L2. In the study investigating prognostic factors in L2 in 868 patients, patients ≥ 40 years had a 5.8 months median OS versus 3.9 for patients < 40 years (p = 0.001 in univariate analysis), and patients ≥ 75 years had a 6.9 median OS versus 5.6 for patients < 75 (p = 0.08). However, there were no significant differences in the multivariate analysis [19]. In our study, our hypothesis is that most patients ≥ 60 years died in L1 (51%, versus 40% of patients < 60 years), leading to the selection of particularly fit elderly patients in L2. The platelet count at baseline was borderline significant in the multivariate analysis for OS (p = 0.056). The prognostic impact of thrombocytosis has also been suggested in other studies, as in the MRC-COIN trial. In this trial including patients with metastatic colorectal cancer, patients with raised baseline-platelet counts receiving intermittent chemotherapy had impaired survival and quality of life [21].
The main strength of our study is that the second-line therapy was planned in the protocol. Our study has some limits. Some data, such as lymphocyte counts and serum LDH levels, are missing from our database. The use of epirubicin in the treatment of gastric cancer is now controversial. A recent study that included 1002 patients from a national registry did not demonstrate any benefit of adding epirubicin to a platinum-fluoropyrimidine doublet chemotherapy, but greater toxicity [22]. There is a need to identify patients who will benefit from antiangiogenic drugs, but no predictive factors have been identified so far.
In conclusion, the benefits of second-line chemotherapy remain limited, with age ≥ 60 years at diagnosis and ECOG score 0/1 before the start of L2 being the only good prognostic factors in this study. Robust prognostic and predictive factors still need to be confirmed in prospective trials.
References
Global Burden of Disease Cancer Collaboration. Fitzmaurice C, Dicker D, Pain A, Hamavid H, Moradi-Lakeh M, et al. The global burden of cancer 2013. JAMA Oncol. 2015;1:505–27. https://doi.org/10.1001/jamaoncol.2015.0735.
Van Cutsem E, Moiseyenko VM, Tjulandin S, Majlis A, Constenla M, Boni C, et al. Phase III study of docetaxel and cisplatin plus fluorouracil compared with cisplatin and fluorouracil as first-line therapy for advanced gastric cancer: a report of the V325 Study Group. J Clin Oncol. 2006;24:4991–7. https://doi.org/10.1200/JCO.2006.06.8429.
Cunningham D, Starling N, Rao S, Iveson T, Nicolson M, Coxon F, et al. Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med. 2008;358:36–46. https://doi.org/10.1056/NEJMoa073149.
Koizumi W, Narahara H, Hara T, Takagane A, Akiya T, Takagi M, et al. S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet Oncol. 2008;9:215–21. https://doi.org/10.1016/S1470-2045(08)70035-4.
Bang Y-J, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet. 2010;376:687–97. https://doi.org/10.1016/S0140-6736(10)61121-X.
Ford HER, Marshall A, Bridgewater JA, Janowitz T, Coxon FY, Wadsley J, et al. Docetaxel versus active symptom control for refractory oesophagogastric adenocarcinoma (COUGAR-02): an open-label, phase 3 randomised controlled trial. Lancet Oncol. 2014;15:78–86. https://doi.org/10.1016/S1470-2045(13)70549-7.
Higuchi K, Tanabe S, Shimada K, Hosaka H, Sasaki E, Nakayama N, et al. Biweekly irinotecan plus cisplatin versus irinotecan alone as second-line treatment for advanced gastric cancer: a randomised phase III trial (TCOG GI-0801/BIRIP trial). Eur J Cancer 1990. 2014;50:1437–45. https://doi.org/10.1016/j.ejca.2014.01.020.
Thuss-Patience PC, Kretzschmar A, Bichev D, Deist T, Hinke A, Breithaupt K, et al. Survival advantage for irinotecan versus best supportive care as second-line chemotherapy in gastric cancer—a randomised phase III study of the Arbeitsgemeinschaft Internistische Onkologie (AIO). Eur J Cancer. 2011;47:2306–14. https://doi.org/10.1016/j.ejca.2011.06.002.
Fuchs CS, Tomasek J, Yong CJ, Dumitru F, Passalacqua R, Goswami C, et al. Ramucirumab monotherapy for previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (REGARD): an international, randomised, multicentre, placebo-controlled, phase 3 trial. Lancet. 2014;383:31–9. https://doi.org/10.1016/S0140-6736(13)61719-5.
Wilke H, Muro K, Van Cutsem E, Oh S-C, Bodoky G, Shimada Y, et al. Ramucirumab plus paclitaxel versus placebo plus paclitaxel in patients with previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (RAINBOW): a double-blind, randomised phase 3 trial. Lancet Oncol. 2014;15:1224–35. https://doi.org/10.1016/S1470-2045(14)70420-6.
Kang Y-K, Boku N, Satoh T, Ryu M-H, Chao Y, Kato K, et al. Nivolumab in patients with advanced gastric or gastro-oesophageal junction cancer refractory to, or intolerant of, at least two previous chemotherapy regimens (ONO-4538-12, ATTRACTION-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;390:2461–71. https://doi.org/10.1016/S0140-6736(17)31827-5.
Guimbaud R, Louvet C, Ries P, Ychou M, Maillard E, André T, et al. Prospective, randomized, multicenter, phase III study of fluorouracil, leucovorin, and irinotecan versus epirubicin, cisplatin, and capecitabine in advanced gastric adenocarcinoma: a French intergroup (Fédération Francophone de Cancérologie Digestive, Fédération Nationale des Centres de Lutte Contre le Cancer, and Groupe Coopérateur Multidisciplinaire en Oncologie) study. J Clin Oncol. 2014;32:3520–6. https://doi.org/10.1200/JCO.2013.54.1011.
Hironaka S, Ueda S, Yasui H, Nishina T, Tsuda M, Tsumura T, et al. Randomized, open-label, phase III study comparing irinotecan with paclitaxel in patients with advanced gastric cancer without severe peritoneal metastasis after failure of prior combination chemotherapy using fluoropyrimidine plus platinum: WJOG 4007 trial. J Clin. 2013;31:4438–44. https://doi.org/10.1200/JCO.2012.48.5805.
Lee J, Lim T, Uhm JE, Park KW, Park SH, Lee SC, et al. Prognostic model to predict survival following first-line chemotherapy in patients with metastatic gastric adenocarcinoma. Ann Oncol. 2007;18:886–91. https://doi.org/10.1093/annonc/mdl501.
Chau I, Norman AR, Cunningham D, Waters JS, Oates J, Ross PJ. Multivariate prognostic factor analysis in locally advanced and metastatic esophago-gastric cancer–pooled analysis from three multicenter, randomized, controlled trials using individual patient data. J Clin Oncol. 2004;22:2395–403. https://doi.org/10.1200/JCO.2004.08.154.
Catalano V, Graziano F, Santini D, D’Emidio S, Baldelli AM, Rossi D, et al. Second-line chemotherapy for patients with advanced gastric cancer: who may benefit? Br J Cancer. 2008;99:1402–7. https://doi.org/10.1038/sj.bjc.6604732.
Hashimoto K, Takashima A, Nagashima K, Okazaki S, Nakajima TE, Kato K, et al. Progression-free survival in first-line chemotherapy is a prognostic factor in second-line chemotherapy in patients with advanced gastric cancer. J Cancer Res Clin Oncol. 2010;136:1059–64. https://doi.org/10.1007/s00432-009-0752-8.
Kanagavel D, Pokataev IA, Fedyanin MY, Tryakin AA, Bazin IS, Narimanov MN, et al. A prognostic model in patients treated for metastatic gastric cancer with second-line chemotherapy. Ann Oncol. 2010;21:1779–85. https://doi.org/10.1093/annonc/mdq032.
Fanotto V, Cordio S, Pasquini G, Fontanella C, Rimassa L, Leone F, et al. Prognostic factors in 868 advanced gastric cancer patients treated with second-line chemotherapy in the real world. Gastric Cancer. 2016. https://doi.org/10.1007/s10120-016-0681-6.
Kong X, Wang J-L, Chen H-M, Fang J-Y. Comparison of the clinicopathological characteristics of young and elderly patients with gastric carcinoma: a meta analysis. J Surg Oncol. 2012;106:346–52. https://doi.org/10.1002/jso.23004.
Adams RA, Meade AM, Seymour MT, Wilson RH, Madi A, Fisher D, et al. Intermittent versus continuous oxaliplatin and fluoropyrimidine combination chemotherapy for first-line treatment of advanced colorectal cancer: results of the randomised phase 3 MRC COIN trial. Lancet Oncol. 2011;12:642–53. https://doi.org/10.1016/S1470-2045(11)70102-4.
Carmona-Bayonas A, Jiménez-Fonseca P, Custodio A, Sánchez Cánovas M, Hernández R, Pericay C, et al. Anthracycline-based triplets do not improve the efficacy of platinum-fluoropyrimidine doublets in first-line treatment of advanced gastric cancer: real-world data from the AGAMEMON National Cancer Registry. Gastric Cancer. 2017. https://doi.org/10.1007/s10120-017-0718-5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
All participants gave their written informed consent before inclusion in the FFCD-0307 trial. The study was approved by relevant ethics committees.
Rights and permissions
About this article
Cite this article
Touchefeu, Y., Guimbaud, R., Louvet, C. et al. Prognostic factors in patients treated with second-line chemotherapy for advanced gastric cancer: results from the randomized prospective phase III FFCD-0307 trial. Gastric Cancer 22, 577–586 (2019). https://doi.org/10.1007/s10120-018-0885-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-018-0885-z