Abstract
Laparoscopic gastrectomy is a widely used minimally invasive surgery for gastric cancer. However, skillful techniques are required to perform lymph node dissection using straight shaped forceps, particularly for D2 dissection. Robotic surgery using the da Vinci surgical system is anticipated to be a powerful tool for performing difficult techniques using high-resolution three-dimensional (3D) images and the EndoWrist equipped with seven degrees of freedom. Attempts are being made to apply robotic surgery in gastrectomy procedures mainly in Japan, South Korea, and Europe. Although definite superiority to laparoscopic gastrectomy is yet to be proven, robotic surgery has been reported to have a shorter learning curve and offer more precise dissection for total gastrectomy. Hence, its oncological efficacy needs to be verified in a clinical trial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The da Vinci Surgical System, a widely used surgical robot, was developed in 1988. High-resolution 3D images and an EndoWrist with seven degrees of freedom enabled overcoming the lack of perspectives and the restriction of maneuverability in laparoscopic surgery. Since the first model was approved in 2000 by the US Food and Drug Administration, it has undergone repeated improvements, and the fourth-generation model is currently available. As of the end of 2014, over 3000 such systems have been delivered to countries throughout the world, including 2185 in the US, 188 in Japan, 82 in France, 72 in Italy, 72 in Germany, and 46 in South Korea. The most common surgical procedures it is used for are total hysterectomy and prostatectomy, accounting for 40 and 32 % of all robotic surgical procedures, respectively. In the US, most prostate cancer cases eligible for surgical treatment undergo robotic surgery [1]. In addition, ever since robotic surgery for total hysterectomy was approved by the FDA in 2005, it has rapidly become widely used, particularly in the US [2]. Robotic surgery has also been applied to procedures for areas other than the pelvic viscera [3]. Although the surgery time and cost issues remain unresolved, robotic surgery is anticipated to become increasingly useful for more advanced types of surgery. This report outlines the state of robotic gastrectomy for gastric cancer and its future outlook.
Introduction of minimally invasive surgery for gastric cancer
Surgery for gastric cancer has followed several transitional pathways in western countries compared to those in Asian countries including Japan. In western countries, cancer accompanied by lymph node metastasis has been strongly perceived to already have evolved into a systemic disease; thus, it was generally thought that the expansion of surgery would not result in improved treatment outcomes for advanced gastric cancer. Because comparative trials involving typical D2 dissection and smaller D1 dissection indicated high rates of postoperative complications and operative mortality rates after D2 dissection, but no difference in survival outcomes, D1 dissection had been established as the standard treatment [4, 5]. In contrast, in Japan it was believed that it was local control of the cancer that could improve treatment outcomes; therefore, a comparative trial involving D2 dissection and the larger D2 + para-aortic lymph node dissection (PAND) was conducted [6]. Because results indicated no difference in survival between the D2 dissection group and expanded dissection group, D2 dissection became the standard treatment for advanced gastric cancer. Meanwhile, when the long-term follow-up results of a trial conducted in the West indicated that gastric cancer-specific survival was clearly better in the D2 dissection group than in the D1 dissection group, the significance of D2 dissection was reacknowledged [7]. Thus, it is suggested that a balance between the extent of dissection and level of surgical invasiveness is important in surgery for gastric cancer and minimally invasive surgery is therefore recognized as being highly significant.
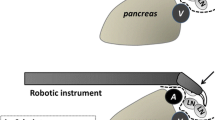
Laparoscopic gastrectomy (LG) is a minimally invasive surgery for gastric cancer. Since LG was first performed by Kitano et al. in 1991 [8], it has rapidly become widespread as a procedure to treat, in particular, early gastric cancer in Japan and South Korea. The Japanese Gastric Cancer Treatment Guidelines recommend D1 or D1 + dissection be performed on cases of early gastric cancer with no imaging study findings suggestive of nodal metastasis. For early gastric cancer with lymph node metastasis or advanced gastric cancer, the said guidelines recommend D2 dissection. With the spread of laparoscopic surgery and technological improvements, D2 dissection has come to be performed at many facilities. However, with regard to lymph node dissection of the superior border of the pancreas, which is most crucial when treating gastric cancer, dissection must include the tissues behind the pancreas, common hepatic artery, and splenic artery. This is very difficult to perform with straight forceps. Various techniques have been devised for the dissection approach [9, 10]; however, all require a high level of skill.
Robotic surgery, in which forceps with seven degrees of freedom can be used, is anticipated to be useful in overcoming the motion restrictions brought about by the use of straight forceps.
Robotic gastrectomy for gastric cancer
Since the first report by Hashizume et al. in 2003 [11], robotic gastrectomy has been investigated as an experimental procedure mainly in Japan, Italy, and South Korea. Relevant papers published before January 2015 were searched using the electronic database PubMed using the search terms robot PLUS gastric cancer OR robotic gastrectomy. A total of 186 articles were identified using this search. Case reports, non-English language manuscripts, and studies not focusing on gastric cancer were excluded. Additional relevant articles were manually searched and included. As a result, 42 original articles and 8 meta-analyses were included in this review. Table 1 shows a list of previously published original articles [11–52]. Most of these were case series studies compiling clinical experiences or retrospective case-control studies and are of very low level evidence. The prospective trials that have been performed comprise only two cohort studies conducted by the National Cancer Center of South Korea and our phase IIa study [32, 42, 48]. The cohort studies, which compared robotic surgery with laparoscopic surgery according to surgical invasiveness and cost, reported no difference for the level of invasiveness [32]. The phase IIa study that we conducted evaluated 18 cases with the incidence of intra-abdominal infectious complications as the primary endpoint. As results indicated no cases of intra-abdominal infectious complications, the study was determined to be positive, and we are now proceeding to the phase IIb study [42]. Although few reports have stated that robotic surgery leads to fewer postoperative complications than laparoscopic surgery, Seo et al. [49] recently reported that the onset rate of pancreatic juice leakage was significantly lower in robotic surgery than in laparoscopic surgery.
Most studies comparing open and laparoscopic surgery are retrospective case-control studies. As almost all of these studies have sample sizes of fewer than 100 cases and significant bias with regard to background factors, the reliability of the data is somewhat questionable. There have recently been eight reports released that conducted meta-analysis on the aforementioned reports altogether [53–60], which are listed in Table 2. However, since there have been no randomized comparative studies, it appears difficult to reach a clear conclusion even if a meta-analysis is performed. Moreover, many of the reports only include dozens of robotic surgery cases, with the only exception of the studies conducted by Yonsei University and Ajou University in South Korea, which included more than 100 cases. Accordingly, even if many reports are analyzed, there is not much point in performing meta-analysis because the results will be greatly influenced by the results from the studies with larger sample sizes. Compared to open surgery, nonetheless, robotic surgery has been shown to have longer surgery duration, lesser bleeding, and a shorter hospital stay. Furthermore, compared to laparoscopic surgery, robotic surgery has been shown to have longer surgery duration, lesser bleeding, and longer distal margins. Analysis of other factors including the number of lymph nodes dissected and the frequency of postoperative complications revealed no differences. Blood loss is generally considered to be minimal with laparoscopic surgery; however, the observed increase in distal margins with robotic surgery compared with laparoscopic surgery has been difficult to explain. As these meta-analyses were performed using non-randomized retrospective case control studies, the level of evidence is quite low, and the observed differences may have been due to chance alone. However, considering the fact that at many facilities these study outcomes were compared between when robotic surgery was first introduced and when laparoscopic surgery had already been a well-practiced technique, it appears that robotic surgery is at the least a relatively safe and reliable method. In the future, mid- to long-term studies that also assess the survival period need to be conducted.
Learning curve of robotic surgery
One significant advantage of robotic surgery is its short learning curve compared to laparoscopic surgery. Four reports have investigated the learning curve of robotic gastrectomy. One hundred cases of robotic gastrectomy at Korea University [30] were divided into the first 20 cases and subsequent 80 cases, and significant differences were observed in surgery duration and the number of days spent in hospital, leading to the conclusion that good outcomes may be achieved after a surgeon has performed the procedure on at least 20 cases. Park et al. [33] investigated the robotic gastrectomy learning curve for surgeons with sufficient experience performing laparoscopic gastrectomy at three facilities in Korea and found that surgeons needed to perform the procedure on an average of 8.2 cases before the surgery time stabilized. Because laparoscopic gastrectomy normally needs to be performed on at least 50 cases before surgery time stabilizes [30], the learning curve for the da Vinci Surgical System has been shown to be extremely short for surgeons with sufficient experience performing laparoscopic gastrectomy. Furthermore, Kim et al. [39] compared the learning curves for robotic surgery and laparoscopic surgery with the same surgeon and found that while the surgery time stabilized at 261 cases for laparoscopic surgery, it stabilized at 121 cases for robotic surgery. They also analyzed the surgical success rate with the Cumulative Summation (CUSUM) score and revealed a cutoff at the 81st case for laparoscopic surgery, but no cutoff for robotic surgery. Thus, it suggests that robotic surgery can be performed safely from the first case if conducted by a surgeon experienced in laparoscopic surgery. Zhou et al. [52] also used the CUSUM score to investigate the learning curves for two surgeons experienced in laparoscopic surgery and found that both had three phases in the curves. These were namely the initial phase (12–14 cases), well-developed phase (15–29 cases), and mastery phase (30 cases), which indicates that if surgeons had sufficient experience in laparoscopic surgery, advanced robotic surgery can be performed after experiencing approximately 30 cases. This appears logical considering the fact that the current robotic gastrectomy technique basically follows that of laparoscopic gastrectomy. Learning curves in surgeons with no prior experience of laparoscopic surgery may be shorter for robotic gastrectomy than for laparoscopic gastrectomy, possibly because of the improved ergonomics and dexterity provided by robotic surgery. However, this issue remains to be fully elucidated. During the early introduction of laparoscopic gastrectomy, the majority of practicing surgeons had previous experience in laparoscopic procedures such as cholecystectomy or colectomy. Should robotic surgery become widespread in the field of general surgery, robotic gastrectomy could be introduced through stepwise robotic surgery training, allowing accurate assessment of the learning curve for this procedure.
Total gastrectomy
In robotic surgery, forceps can be maneuvered with a higher degree of freedom than in laparoscopic surgery; hence, it may prove its superiority in procedures that require more advanced techniques. In the surgical treatment of gastric cancer, more advanced skills are needed for total gastrectomy. In laparoscopic total gastrectomy, reconstructive techniques and lymph node dissection around the splenic artery and splenic hilum area, in particular, are considered highly difficult. There have been two reports from South Korea that compared robotic surgery and laparoscopic surgery only for total gastrectomy (Table 3) [37, 50]. Neither report found any significant differences between the procedures apart from longer surgery time for robotic surgery. However, a study on D2 dissections conducted at Yonsei University demonstrated that the number of dissected lymph nodes in the splenic artery and splenic hilum areas was significantly higher with robotic surgery [50]. As mentioned above, considering the fact that reports used outcomes in the early stage of the introduction of robotic surgery, it is suggested that robotic surgery may become a more effective procedure than laparoscopic surgery at sites where a high level of skill is required.
Current issues and outlook for the future of robotic gastrectomy
The clear superiority of robotic to laparoscopic gastrectomy has not been proven at present. However, as forceps with seven degrees of freedom in robotic surgery have an undeniably strong advantage compared to laparoscopic surgery, it is likely to become an even more useful surgery procedure with the future development of devices and ingenious techniques. The greatest disadvantage of robotic surgery, however, is the loss of sensation. To compensate for this loss, visual correction is considered extremely useful and a visual tactile learning style appears to exist where by a certain level of familiarity allows the surgeon to discern the degree of pressure being placed on tissue from the movements of the master controller and forceps.
In addition, with regard to the cost issues, although robotic surgery is currently monopolized by one company, it is hoped that the cost will reduce when similar devices are developed and sold by other companies in future. As the equipment is currently extremely expensive, it appears that it is mainly used for research in the field of gastrectomies. However, as observed with laparoscopic cholecystectomy, which was introduced in the 1980s, when a significant scale merit is generated once robotic surgery has spread in popularity to some extent, it is anticipated that cost-related problems may be quickly resolved.
Increased operative duration is a further major drawback of robotic gastrectomy. A shortage in energy-based devices, such as ultrasonically activated devices, is the predominant cause of increased operative durations, particularly in Japan. However, several novel devices and systems are currently under development. Issues surrounding operative duration are likely to be resolved with the introduction of these new devices.
The possibility of reducing postoperative complications with robotic surgery was reported by Seo et al. [49]. During our initial experience, we also observed no cases of postoperative intra-abdominal infectious complications. Robotic surgery may increase the ease of reconstruction and reduce postoperative complications in meticulous procedures, particularly peripancreatic lymph node dissection. In Japan, a multi-institutional prospective clinical trial evaluating the feasibility and efficacy of robotic gastrectomy is now being conducted under the advanced medical care system. The primary outcome of this study is the incidence of postoperative complications. The incidence of postoperative complications in robotic gastrectomy is presumed to be less than half of that in laparoscopic gastrectomy. Although this trial is a single-arm phase II study, this is the first prospective multi-institutional study evaluating the feasibility of robotic gastrectomy. Once the feasibility of robotic gastrectomy has been established, the application of robotic surgery to more complex procedures, such as surgical resection of tumors of the esophagogastric junction and pancreaticoduodenectomy, is likely as the advantages of robotic surgery may be more pronounced in complex surgical procedures. From there, the survival benefit of robotic surgery, counterbalanced by the increased cost, should be evaluated by well-designed clinical trials.
Parts of this report have already been published in Japanese (Rinsho-Geka vol. 69, 12: 1382–1388, 2014).
References
Sohn W, Lee HJ, Ahlering TE. Robotic surgery: review of prostate and bladder cancer. Cancer J. 2013;19:133–9.
Sinha R, Sanjay M, Rupa B, Kumari S. Robotic surgery in gynecology. J Minim Access Surg. 2015;11:50–9.
Diana M, Marescaux J. Robotic surgery. Br J Surg. 2015;102:e15–28.
Cuschieri A, Fayers P, Fielding J, Craven J, Bancewicz J, Joypaul V, et al. Postoperative morbidity and mortality after D1 and D2 resections for gastric cancer: preliminary results of the MRC randomised controlled surgical trial. The Surgical Cooperative Group. Lancet. 1996;347:995–9.
Bonenkamp JJ, Hermans J, Sasako M, van de Velde CJ, Welvaart K, Songun I, et al. Extended lymph-node dissection for gastric cancer. N Engl J Med. 1999;340:908–14.
Sasako M, Sano T, Yamamoto S, Kurokawa Y, Nashimoto A, Kurita A, et al. D2 lymphadenectomy alone or with para-aortic nodal dissection for gastric cancer. N Engl J Med. 2008;359:453–62.
Songun I, Putter H, Kranenbarg EM, Sasako M, van de Velde CJ. Surgical treatment of gastric cancer: 15-year follow-up results of the randomised nationwide Dutch D1D2 trial. Lancet Oncol. 2010;11:439–49.
Kitano S, Iso Y, Moriyama M, Sugimachi K. Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc. 1994;4:146–8.
Kanaya S, Haruta S, Kawamura Y, Yoshimura F, Inaba K, Hiramatsu Y, et al. Video: laparoscopy distinctive technique for suprapancreatic lymph node dissection: medial approach for laparoscopic gastric cancer surgery. Surg Eendsc. 2011;25:3928–9.
Fukunaga T, Hiki N, Tokunaga M, Nohara K, Akashi Y, Katayama H, et al. Left-sided approach for suprapancreatic lymph node dissection in laparoscopy-assisted distal gastrectomy without duodenal transection. Gastric Cancer. 2009;12:106–12.
Hashizume M, Sugimachi K. Robot-assisted gastric surgery. Surg Clin North Am. 2003;83:1429–44.
Kakeji Y, Konishi K, Ieiri S, Yasunaga T, Nakamoto M, Tanoue K, et al. Robotic laparoscopic distal gastrectomy: a comparison of the da Vinci and Zeus systems. Int J Med Robot. 2006;2:299–304.
Anderson C, Ellenhorn J, Hellan M, Pigazzi A. Pilot series of robot-assisted laparoscopic subtotal gastrectomy with extended lymphadenectomy for gastric cancer. Surg Endosc. 2007;21:1662–6.
Patriti A, Ceccarelli G, Bellochi R, Bartoli A, Spaziani A, Di Zitti L, et al. Robot-assisted laparoscopic total and partial gastric resection with D2 lymph node dissection for adenocarcinoma. Surg Eendsc. 2008;22:2753–60.
Pugliese R, Maggioni D, Sansonna F, Ferrari GC, Forgione A, Costanzi A, et al. Outcomes and survival after laparoscopic gastrectomy for adenocarcinoma. Analysis on 65 patients operated on by conventional or robot-assisted minimal access procedures. Eur J Surg Oncol. 2009;35:281–8.
Song J, Kang WH, Oh SJ, Hyung WJ, Choi SH, Noh SH. Role of robotic gastrectomy using da Vinci system compared with laparoscopic gastrectomy: initial experience of 20 consecutive cases. Surg Endsc. 2009;23:1204–11.
Song J, Oh SJ, Kang WH, Hyung WJ, Choi SH, Noh SH. Robot-assisted gastrectomy with lymph node dissection for gastric cancer: lessons learned from an initial 100 consecutive procedures. Ann Surg. 2009;249:927–32.
Tomulescu V, Stanciulea O, Balescu I, Vasile S, Tudor S, Gheorghe C, et al. First year experience of robotic-assisted laparoscopic surgery with 153 cases in a general surgery department: indications, technique and results. Chirurgia (Bucur). 2009;104:141–50.
Hur H, Kim JY, Cho YK, Han SU. Technical feasibility of robot-sewn anastomosis in robotic surgery for gastric cancer. J Laparoendosc Adv Surg Tech A. 2010;20:693–7.
Kim MC, Heo GU, Jung GJ. Robotic gastrectomy for gastric cancer: surgical techniques and clinical merits. Surg Endsc. 2010;24:610–5.
Pugliese R, Maggioni D, Sansonna F, Costanzi A, Ferrari GC, Di Lernia S, et al. Subtotal gastrectomy with D2 dissection by minimally invasive surgery for distal adenocarcinoma of the stomach: results and 5-year survival. Surg Endsc. 2010;24:2594–602.
Caruso S, Patriti A, Marrelli D, Ceccarelli G, Ceribelli C, Roviello F, et al. Open vs robot-assisted laparoscopic gastric resection with D2 lymph node dissection for adenocarcinoma: a case-control study. Int J Med Robot. 2011;7:452–8.
D’Annibale A, Pende V, Pernazza G, Monsellato I, Mazzocchi P, Lucandri G, et al. Full robotic gastrectomy with extended (D2) lymphadenectomy for gastric cancer: surgical technique and preliminary results. J Surg Res. 2011;166:e113–20.
Isogaki J, Haruta S, Man IM, Suda K, Kawamura Y, Yoshimura F, et al. Robot-assisted surgery for gastric cancer: experience at our institute. Pathobiology. 2011;78:328–33.
Lee HH, Hur H, Jung H, Jeon HM, Park CH, Song KY. Robot-assisted distal gastrectomy for gastric cancer: initial experience. Am J Surg. 2011;201:841–5.
Patriti A, Ceccarelli G, Ceribelli C, Bartoli A, Spaziani A, Cisano C, et al. Robot-assisted laparoscopic management of cardia carcinoma according to Siewert recommendations. Int J Med Robot. 2011;7:170–7.
Woo Y, Hyung WJ, Pak KH, Inaba K, Obama K, Choi SH, et al. Robotic gastrectomy as an oncologically sound alternative to laparoscopic resections for the treatment of early-stage gastric cancers. Arch Surg. 2011;146:1086–92.
Eom BW, Yoon HM, Ryu KW, Lee JH, Cho SJ, Lee JY, et al. Comparison of surgical performance and short-term clinical outcomes between laparoscopic and robotic surgery in distal gastric cancer. Eur J Surg Oncol. 2012;38:57–63.
Huang KH, Lan YT, Fang WL, Chen JH, Lo SS, Hsieh MC, et al. Initial experience of robotic gastrectomy and comparison with open and laparoscopic gastrectomy for gastric cancer. J Gastrointest Surg. 2012;16:1303–10.
Kang BH, Xuan Y, Hur H, Ahn CW, Cho YK, Han SU. Comparison of surgical outcomes between robotic and laparoscopic gastrectomy for gastric cancer: the learning curve of robotic surgery. J Gastric Cancer. 2012;12:156–63.
Kim KM, An JY, Kim HI, Cheong JH, Hyung WJ, Noh SH. Major early complications following open, laparoscopic and robotic gastrectomy. Br J Surg. 2012;99:1681–7.
Park JY, Jo MJ, Nam BH, Kim Y, Eom BW, Yoon HM, et al. Surgical stress after robot-assisted distal gastrectomy and its economic implications. Br J Surg. 2012;99:1554–61.
Park SS, Kim MC, Park MS, Hyung WJ. Rapid adaptation of robotic gastrectomy for gastric cancer by experienced laparoscopic surgeons. Surg Endsc. 2012;26:60–7.
Uyama I, Kanaya S, Ishida Y, Inaba K, Suda K, Satoh S. Novel integrated robotic approach for suprapancreatic D2 nodal dissection for treating gastric cancer: technique and initial experience. World J Surg. 2012;36:331–7.
Vasilescu C, Popa M, Tudor S, Manuc M, Diculescu M. Robotic surgery of locally advanced gastric cancer—an initial experience. Acta Chir Belg. 2012;112:209–12.
Vasilescu C, Procopiuc L. Robotic surgery of locally advanced gastric cancer: a single-surgeon experience of 41 cases. Chirurgia (Bucur). 2012;107:510–7.
Yoon HM, Kim YW, Lee JH, Ryu KW, Eom BW, Park JY, et al. Robot-assisted total gastrectomy is comparable with laparoscopically assisted total gastrectomy for early gastric cancer. Surg Endsc. 2012;26:1377–81.
Hyun MH, Lee CH, Kwon YJ, Cho SI, Jang YJ, Kim DH, et al. Robot versus laparoscopic gastrectomy for cancer by an experienced surgeon: comparisons of surgery, complications, and surgical stress. Ann Surg Oncol. 2013;20:1258–65.
Kim HI, Park MS, Song KJ, Woo Y, Hyung WJ. Rapid and safe learning of robotic gastrectomy for gastric cancer: multidimensional analysis in a comparison with laparoscopic gastrectomy. Eur J Surg Oncol. 2013;40:1346–54.
Liu XX, Jiang ZW, Chen P, Zhao Y, Pan HF, Li JS. Full robot-assisted gastrectomy with intracorporeal robot-sewn anastomosis produces satisfying outcomes. World J Gastroenterol. 2013;19:6427–37.
Park JY, Kim YW, Ryu KW, Eom BW, Yoon HM, Reim D. Emerging Role of Robot-assisted Gastrectomy: analysis of Consecutive 200 Cases. J Gastric Cancer. 2013;13:255–62.
Tokunaga M, Sugisawa N, Kondo J, Tanizawa Y, Bando E, Kawamura T, et al. Early phase II study of robot-assisted distal gastrectomy with nodal dissection for clinical stage IA gastric cancer. Gastric Cancer. 2013;17:542–7.
Han DS, Suh YS, Ahn HS, Kong SH, Lee HJ, Kim WH, et al. Comparison of surgical outcomes of robot-assisted and laparoscopy-assisted pylorus-preserving gastrectomy for gastric cancer: a propensity score matching analysis. Ann Surg Oncol. 2014. doi:10.1245/s10434-014-4204-6
Huang KH, Lan YT, Fang WL, Chen JH, Lo SS, Li AF, et al. Comparison of the operative outcomes and learning curves between laparoscopic and robotic gastrectomy for gastric cancer. PLoS ONE. 2014;9:e111499.
Junfeng Z, Yan S, Bo T, Yingxue H, Dongzhu Z, Yongliang Z, et al. Robotic gastrectomy versus laparoscopic gastrectomy for gastric cancer: comparison of surgical performance and short-term outcomes. Surg Endsc. 2014;28:1779–87.
Kwon IG, Cho I, Guner A, Choi YY, Shin HB, Kim HI, et al. Minimally invasive surgery for remnant gastric cancer: a comparison with open surgery. Surg Endosc. 2014;28:2452–8
Noshiro H, Ikeda O, Urata M. Robotically-enhanced surgical anatomy enables surgeons to perform distal gastrectomy for gastric cancer using electric cautery devices alone. Surg Endsc. 2014;28:1180–7.
Park JY, Eom BW, Jo MJ, Yoon HM, Ryu KW, Kim YW, et al. Health-related quality of life after robot-assisted distal gastrectomy in early gastric cancer. World J Surg. 2014;38:1112–20.
Seo HS, Shim JH, Jeon HM, Park CH, Song KY. Postoperative pancreatic fistula after robot distal gastrectomy. J Surg Res. 2014. doi:10.1016/j.jss.2014.10.022.
Son T, Lee JH, Kim YM, Kim HI, Noh SH, Hyung WJ. Robotic spleen-preserving total gastrectomy for gastric cancer: comparison with conventional laparoscopic procedure. Surg Endsc. 2014;28:2606–15.
Lee J, Kim YM, Woo Y, Obama K, Noh SH, Hyung WJ. Robotic distal subtotal gastrectomy with D2 lymphadenectomy for gastric cancer patients with high body mass index: comparison with conventional laparoscopic distal subtotal gastrectomy with D2 lymphadenectomy. Surg Endosc. 2015. doi:10.1007/s00464-015-4069-1
Zhou J, Shi Y, Qian F, Tang B, Hao Y, Zhao Y, et al. Cumulative summation analysis of learning curve for robot-assisted gastrectomy in gastric cancer. J Surg Oncol. 2015. doi:10.1002/jso.23876.
Liao G, Chen J, Ren C, Li R, Du S, Xie G, et al. Robotic versus open gastrectomy for gastric cancer: a meta-analysis. PLoS ONE. 2013;8:e81946.
Xiong B, Ma L, Zhang C. Robotic versus laparoscopic gastrectomy for gastric cancer: a meta-analysis of short outcomes. Surg Oncol. 2012;21:274–80.
Xiong J, Nunes QM, Tan C, Ke N, Chen Y, Hu W, et al. Comparison of short-term clinical outcomes between robotic and laparoscopic gastrectomy for gastric cancer: a meta-analysis of 2495 patients. J Laparoendosc Adv Surg Tech A. 2013;23:965–76.
Liao GX, Xie GZ, Li R, Zhao ZH, Sun QQ, Du SS, et al. Meta-analysis of outcomes compared between robotic and laparoscopic gastrectomy for gastric cancer. Asian Pac J Cancer Prev. 2013;14:4871–5.
Shen WS, Xi HQ, Chen L, Wei B. A meta-analysis of robotic versus laparoscopic gastrectomy for gastric cancer. Surg Endsc. 2014;28:2795–802.
Hyun MH, Lee CH, Kim HJ, Tong Y, Park SS. Systematic review and meta-analysis of robotic surgery compared with conventional laparoscopic and open resections for gastric carcinoma. Br J Surg. 2013;100:1566–78.
Marano A, Choi YY, Hyung WJ, Kim YM, Kim J, Noh SH. Robotic versus laparoscopic versus open gastrectomy: a meta-analysis. J Gastric Cancer. 2013;13:136–48.
Zong L, Seto Y, Aikou S, Takahashi T. Efficacy evaluation of subtotal and total gastrectomies in robotic surgery for gastric cancer compared with that in open and laparoscopic resections: a meta-analysis. PLoS ONE. 2014;9:e103312.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Terashima, M., Tokunaga, M., Tanizawa, Y. et al. Robotic surgery for gastric cancer. Gastric Cancer 18, 449–457 (2015). https://doi.org/10.1007/s10120-015-0501-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-015-0501-4