Abstract
Purpose
To identify the surgical instrument that allows for optimal healing of tongue incisions.
Methods
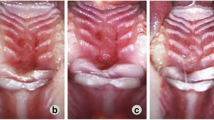
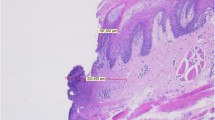
An Er:YAG laser was compared with different pulse energies to a conventional scalpel for the incision of mouse tongue tissues. Mice were sacrificed through cervical dislocation at 24, 48, and 72 h postoperatively, followed by extraction of their tongues for incision experiments. The healing of the incisions and expression of inflammation- and pain-related factors in the tongues were compared between the surgical procedure groups.
Results
In laser-treated mice, tongue incisions healed the fastest when the laser output energy was 60 MJ per pulse. Macrophage chemotaxis toward the incisional area was triggered on the first postoperative day for the 60-MJ group, while the time for macrophage chemotaxis to the surgical area was later in the 80-MJ group. Tumor necrosis factor-alpha expression increased and then decreased in the 80-MJ group; however, it gradually decreased in the 60-MJ and conventional scalpel groups. Prostaglandin E2 expression increased and then decreased in the 80-MJ and conventional scalpel groups but gradually decreased in the 60-MJ group. The expression of transforming growth factor beta 1 gradually decreased in the 60-MJ and 80-MJ groups but gradually increased in the conventional scalpel group.
Conclusion
Compared with surgical procedures using conventional scalpels, those using an Er:YAG laser with appropriate pulse energies can inhibit inflammation in the incisional area and promote incision healing. The use of an Er:YAG laser with appropriate pulse energies can alleviate intraoperative and postoperative pain in the incisional area.





Similar content being viewed by others
Data availability
Data are available on request to the authors.
References
Liboon J, Funkhouser W, Terris DJ (1997) A com-parison of mucosal incisions made by scale-pel, CO2 laser, electrocautery, and constant-voltage. Otolaryngol Head Neck Surg 116:379–385. https://doi.org/10.1016/S0194-5998977027
Morosolli AC, Veeck EB, Niccoli-Filho W, Gomes MF, Goulart MV (2010) Healing process after surgical treatment with scalpel, electrocautery and laser radiation: histomorphologic and histomorphometric analysis. Lasers Med Sci 25:93–100. https://doi.org/10.1007/s10103-009-0674-3
Matsumoto K, Suzuki H, Usami Y, Hattori M, Komoro T (2008) Histological evaluation of artifacts in tongue tissue produced by the CO2 laser and the electrotome. Photomed Laser Surg 26:573–577. https://doi.org/10.1089/pho.2007.2217
Pick RM, Pecaro BC (1987) Use of the CO2 laser in soft tissue dental surgery. Lasers Surg Med 7:207–213. https://doi.org/10.1002/lsm.1900070213
Featherstone JD, Nelson DG (1987) Laser effects on dental hard tissues. Adv Dent Res 1:21–26. https://doi.org/10.1177/08959374870010010701
Goldman L, Hornby P, Meyer R, Goldman B (1964) Impact of the laser on dental caries. Nature 203:417. https://doi.org/10.1038/203417a0
Taylor R, Shklar G, Roeber F (1965) The effects on laser radiation on teeth dental pulp on oral mucosa on experimental animals. Oral Surg Oral Med Pathol 19:786–795. https://doi.org/10.1016/0030-4220(65)90351-8
Stern E, Sognnaes RF, Goodman NF (1966) Laser effects on in vitro enamel permeability and solubility. J Am Dent Assoc 73:838–843. https://doi.org/10.14219/jada.archive.1966.0319
Anić I, Segović S, Katanec D, Prskalo K, Najzar-Fleger D (1998) Scanning electron microscopic study of dentin lased with argon, CO2, and Nd:YAG laser. J Endod 24:77–81. https://doi.org/10.1016/S0099-2399(98)80081-2
Loh HS (1992) A clinical investigation of the management of oral lichen planus with CO2 laser surgery. J Clin Laser Med Surg 10:445–449. https://doi.org/10.1089/clm.1992.10.445
Salama FS (1998) Effect of laser pretreated enamel and dentin of primary teeth on microleakage of different restorative materials. J Clin Pediatr Dent 22:285–291
Schwarz F, Sculean A, Georg T, Reich E (2001) Periodontal treatment with an Er:YAG laser compared to scaling and root planing. A controlled clinical study. J Periodontol 72:361–367. https://doi.org/10.1902/jop.2001.72.3.361
Kellesarian SV, Ros MV, Aldosary KM, Javed F (2018) Laser-assisted removal of all ceramic fixed dental prostheses: a comprehensive review. J Esthet Restor Dent 30:216–222. https://doi.org/10.1111/jerd.12360
Zhang Y, Jiang A (2020) The influence of Er: YAG laser treatment on the shear bond strength of enamel and dentin: a systematic review and meta-analysis. Quintessence Int 51:8–16
Van As G (2004) Erbium lasers in dentistry. Dent Clin N Am 48:1017–1059. https://doi.org/10.1016/j.cden.2004.06.001
Zaffe D, Vitale MC, Martignone A, Scarpelli F, Botticelli AR (2004) Morphological, histochemical, and immunocytochemical study of CO2 and Er:YAG laser effect on oral soft tissues. Photomed Laser Surg 22:185–189. https://doi.org/10.1089/1549541041438678
Romeo U, Libotte F, Palaia G, Del Vecchio A, Tenore G, Visca P, Nammour S, Polimeni A (2012) Histological in vitro evaluation of the effects of Er:YAG laser on oral soft tissues. Lasers Med Sci 27:749–753. https://doi.org/10.1007/s10103-011-0969-z
Merigo E, Clini F, Fornaini C, Oppici A, Paties C, Zangrandi A, Fontana M, Rocca JP, Meleti M, Manfredi M, Cella L, Vescovi P (2013) Laser-assisted surgery with different wavelengths: a preliminary ex vivo study on thermal increase and histological evaluation. Lasers Med Sci 28:497–504. https://doi.org/10.1007/s10103-012-1081-8
Tamarit Borrás M, Delgado Molina E, Berini Aytés L, Gay Escoda C (2005) Removal of hyperplastic lesions of the oral cavity. a retrospective study of 128 cases. Med Oral Patol Oral Cir Bucal 10:151–162
Yagüe-García J, Espa-a-Tost AJ, Berini-Aytés L, Gay-Escoda C (2009) Treatment of oral mucocele - scalpel versus CO2 Laser. Med Oral Patol Oral Cir Bucal 14:e469–e474
Vescovi P, Manfredi M, Merigo E, Meleti M, Fornaini C, Rocca JP, Nammour S (2010) Surgical approach with Er:YAG laser on osteonecrosis of the jaws (ONJ) in patients under bisphosphonate therapy (BPT). Lasers Med Sci 25:101–113. https://doi.org/10.1007/s10103-009-0687-y
Nammour S, Zeinoun T, Namour A, Vanheusden A, Vescovi P (2017) Evaluation of different laser-supported surgical protocols for the treatment of oral leukoplakia: a long-term follow-up. Photomed Laser Surg 35:629–638. https://doi.org/10.1089/pho.2016.4256
Jerjes W, Upile T, Hamdoon Z, Mosse CA, Akram S, Hopper C (2011) Prospective evaluation of outcome after transoral CO2 laser resection of T1/T2 oral squamous cell carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112:180–187. https://doi.org/10.1016/j.tripleo.2010.09.078
Schwarz F, Aoki A, Becker J, Sculean A (2008) Laser application in non-surgical periodontal therapy: a systematic review. J Clin Periodontol 35:29–44. https://doi.org/10.1111/j.1600-051X.2008.01259.x
Ishikawa I, Aoki A, Takasaki AA, Mizutani K, Sasaki KM (2000) Izumi Y (2009) Application of lasers in periodontics: true innovation or myth? Periodontol 50:90–126
Schwarz F, Schmucker A, Becker J (2015) Efficacy of alternative or adjunctive measures to conventional treatment of peri-implant mucositis and peri-implantitis: a systematic review and meta-analysis. Int J Implant Dent 1:22. https://doi.org/10.1186/s40729-015-0023-1
Weber JB, Camilotti RS, Ponte ME (2016) Efficacy of laser therapy in the management of bis-phosphonate-related osteonecrosis of the jaw (BRONJ): a systematic review. Lasers Med Sci 31:1261–1272. https://doi.org/10.1007/s10103-016-1929-4
Giovannacci I, Giunta G, Pedrazzi G, Meleti M, Manfredi M, Migliario M, Brucoli M, Greco Lucchina A, Mortellaro C, Vescovi P (2018) Erbium yttrium -aluminum-garnet laser versus traditional bur in the extraction of impacted mandibular third molars: analysis of intra- and postoperative differences. J Craniofac Surg 29:2282–2286. https://doi.org/10.1097/SCS.0000000000004574
Li H, Liu Y, Li X, Juan D, Guo L, Liu Y (2022) A histological evaluation of the mice oral mucosal tissue incisions excised with diode laser, Er:YAG laser, and cold scalpel. Lasers Med Sci 37:2707–2715. https://doi.org/10.1007/s10103-022-03544-w
Yen-Chun Koh, Guliang Yang, Ching-Shu Lai, Monthana Weerawatanakorn, Min-Hsiung Pan (2018) Chemopreventive Effects of Phytochemicals and Medicines on M1/M2 Polarized Macrophage Role in Inflammation-Related Diseases. Int J Mol Sci 19(8):2208. https://doi.org/10.3390/ijms19082208
Shapouri-Moghaddam A, Mohammadian S, Vazini H, Taghadosi M, Esmaeili S-A, Mardani F, Seifi B, Mohammadi A, Afshari JT, Sahebkar A (2018) Macrophage plasticity, polarization, and function in health and disease. J Cell Physiol 233(9):6425–6440. https://doi.org/10.1002/jcp.26429
Author et al (2009)
Liu JY, Chen B, Bao J, Zhang YH, Lei L, Yan FH (2019) Macrophage polarization in periodontal ligament stem cells enhanced periodontal regeneration. Stem Cell Res Ther 10:320. https://doi.org/10.1186/s13287-019-1409-4
Vogel DS, Glim JE, Stavenuiter AD, Breur M, Priscilla HP, Amor S, Dijkstra CD, Beelen RJ (2014) Human macrophage polarization in vitro: maturation and activation methods compared. Immunobiology 219:695–703. https://doi.org/10.1016/j.imbio.2014.05.002
Zhang ZY, Huang SS, Wu SF, Qi JJ, Li WC, Liu SS, Cong Y, Chen HW, Lu LW, Shi ST, Wang DD, Chen WJ, Sun LY (2019) Clearance of apoptotic cells by mesenchymal stem cells contributes to immunosuppression via PGE2. EBioMedicine 45:341–350. https://doi.org/10.1016/j.ebiom.2019.06.016
Yan XJ, Pan Q, Xin HH, Chen YX, Ping Y (2021) Genome-editing prodrug: targeted delivery and conditional stabilization of CRISPR-Cas9 for precision therapy of inflammatory disease. Sci Adv 7:eabj0624. https://doi.org/10.1126/sciadv.abj0624
Liao CH, Fei W, Shen ZH, Yin MP, Lu C (2014) Expression and distribution of TNF-α and PGE2 of periodontal tissues in rat periodontitis model. Asian Pac J Trop Med 7:412–416. https://doi.org/10.1016/S1995-7645(14)60067-5
Oliveira RD, Wilson SE (2020) Fibrocytes, wound healing, and corneal fibrosis. Invest Ophthalmol Vis Sci 61:28. https://doi.org/10.1167/iovs.61.2.28
Lodyga M, Hinz B (2020) TGF-β1 – a truly transforming growth factor in fibrosis and immunity. Semin Cell Dev Biol 101:123–139. https://doi.org/10.1016/j.semcdb.2019.12.010
Kaya GS, Yavuz YG, Sümbüllü MA, Dayi E (2012) A comparison of diode laser and Er:YAG lasers in the treatment of gingival melanin pigmentation. Oral Surg Oral Med Oral Pathol Oral Radiol 113:293–299. https://doi.org/10.1016/j.tripleo.2011.03.005
Ishikawa I, Aoki A, Takasaki AA (2008) Clinical application of erbium: YAG laser in periodontology. J Int Acad Periodontol 10:22–30
Merigo E, Clini F, Fornaini C, Oppici A, Paties C, Zangrandi A, Fontana M, Rocca JP, Meleti M, Manfredi M, Cella L, Vescovi P (2013) Laser-assisted surgery with different wave-lengths: a preliminary ex vivo study on thermal increase and histological evaluation. Lasers Med Sci 28:497–504. https://doi.org/10.1007/s10103-012-1081-8
Azevedo AS, Monteiro LS, Ferreira F, Delgado ML, Garcês F, Carreira S, Martins M, Suarez-Quintanilla J (2016) In vitro histological evaluation of the surgical edges made by different laser wavelengths in tongue tissues. J Clin Exp Dent 8:e388–e396. https://doi.org/10.4317/jced.52830
Suter VG, Altermatt HJ, Bornstein MM (2017) A randomized controlled clinical and histo-pathological trial comparing excisional biopsies of oral fibrous hyperplasias using CO2 and Er:YAG laser. Lasers Med Sci 32:573–581. https://doi.org/10.1007/s10103-017-2151-8
Monteiro L, Delgado ML, Garcês F, Machado M, Ferreira F, Martins M, Salazar F, Pacheco JJ (2019) A histological evaluation of the surgical edges from human oral fibrous-epithelial lesions excised with CO2 laser, Diode laser, Er:YAG laser, Nd:YAG laser, electrosurgical scalpel and cold scalpel. Med Oral Patol Oral Cir Bucal 24:e271–e280
Moalem G, Tracey DJ (2006) Immune and inflammatory mechanisms in neuropathic pain. Brain Res Rev 51:240–264. https://doi.org/10.1016/j.brainresrev.2005.11.004
Mantovani A, Schioppa T, Biswas SK, Marchesi F, Allavena P, Sica A (2003) Tumor-associated macrophages and dendritic cells as prototypic type II polarized myeloid populations. Tumori 89:459–468. https://doi.org/10.1177/030089160308900501
Lucas T, Waisman A, Ranjan R, Roes J, Krieg T, Müller W, Roers A, Eming SA (2010) Differential roles of macrophages in diverse phases of skin repair. J Immunol 184:3964–3977. https://doi.org/10.4049/jimmunol.0903356
Labonte AC, Tosello-Trampont AC, Hahn YS (2014) The role of macrophage polarization in infectious and inflammatory diseases. Molecules and Cells 37:275–285. https://doi.org/10.14348/molcells.2014.2374
Bertasso AS, Léon JE, Silva RA, Silva LA, de Queiroz AM, Pucinelli CM, Romualdo PC, Nelson-Filho P (2020) Immunophenotypic quantification of M1 and M2 macrophage polarization in radicular cysts of primary and permanent teeth. Int Endod J 53:627–635. https://doi.org/10.1111/iej.13257
Vogel DS, Glim JE, Stavenuiter AD, Breur M, Heijnen P, Amor S, Christine D, Dijkstra CD, Beelen RJ (2014) Human macrophage polarization in vitro: maturation and activation methods compared. Immunobiology 219:695–703. https://doi.org/10.1016/j.imbio.2014.05.002
Adams DO, Hamilton TA (1984) The cell biology of macrophage activation. Annu Rev Immunol 2:283–318
Feldmann M, Brennan FM, Elliott M, Katsikis P, Maini RN (1994) TNF alpha as a therapeutic target in rheumatoid arthritis. Circ Shock 43:179–184
Yarilina A, Park-Min KH, Antoniv T, Hu X, Ivashkiv LB (2008) TNF activates an IRF1-dependent autocrine loop leading to sustained expression of chemokines and STAT1-dependent type I interferon-response genes. Nat Immunol 9:378–387. https://doi.org/10.1038/ni1576
Tacke F, Zimmermann HW (2014) Macrophage heterogeneity in liver injury and fibrosis. J Hepatol 60:1090–1096. https://doi.org/10.1016/j.jhep.2013.12.025
Broccoletti R, Arduino PG, Vescovi P, Mergoni G, Mattiuzzi M, Merigo E, DiLupo M, Manfredi M (2014) Quantic molecular resonance scalpel vs traditional scalpel in the treatment of labial mucocele: a two-center randomized controlled trial. Quintessence Int 45:331–338
Chen CK, Chang NJ, Ke JH, Fu E, Lan WH (2013) Er:YAG laser application for removal of keratosis using topical anesthesia. J Dent Sci 8:196–199. https://doi.org/10.1016/j.jds.2012.11.003
Broccoletti R, Cafaro A, Gambino A, Romagnoli E, Arduino PG (2015) Er:YAG laser versus cold knife excision in the treatment of nondysplastic oral lesions: a randomized comparative study for the postoperative period. Photomed Laser Surg 33:604–609. https://doi.org/10.1089/pho.2015.3967
Arnabat-Domínguez J, Bragado-Novel M, España-Tost AJ, Berini-Aytés L, Gay-Escoda C (2010) Advantages and esthetic results of erbium, chromium: yttrium-scandiumgallium-garnet laser application in second-stage implant surgery in patients with insufficient gingival attachment: a report of three cases. Lasers Med Sci 25:459–464. https://doi.org/10.1007/s10103-009-0728-6
Rosa DS, Aranha AC, Eduardo Cde P, Aoki A (2007) Esthetic treatment of gingival melanin hyperpigmentation with Er:YAG laser: short-term clinical observations and patient follow-up. J Periodontol 78:2018–2025. https://doi.org/10.1902/jop.2007.070041
Schwarz F, Maraki D, Yalcinkaya S, Bieling K, Böcking A, Becker J (2005) Cytologic and DNA-cytometric follow-up of oral leukoplakia after CO2- and Er :YAG-laser assisted ablation: a pilot study. Lasers Surg Med 37:29–36. https://doi.org/10.1002/lsm.20188
Matys J, Dominiak M (2016) Assessment of pain when uncovering implants with Er:YAG laser or scalpel for second stage surgery. Adv Clin Exp Med 25:1179–1184. https://doi.org/10.17219/acem/62456
Fornaini C, Rocca JP, Merigo E, Meleti M, Manfredi M, Nammour S, Vescovi P (2012) Low energy KTP laser in oral soft tissue surgery: a 52 patients clinical study. Med Oral Patol Oral Cir Bucal 17:287–291
Berger JW, Amico DJ (1997) Modeling of erbium: YAG laser-mediated explosive photovaporization: implications for vitreoretinal surgery. Ophthalmic Surg Lasers 28:133–139. https://doi.org/10.3928/1542-8877-19970201-09
Qu W, Shang J, Liu L, Xu D, Du P, Liu Z (2018) Comparative study on the incision healing of the palatal mucosa by using Er:YAG laser or traditional scalpel in the SD rats. Lasers Med Sci 33:1019–1024. https://doi.org/10.1007/s10103-018-2450-8
Kawabata A (2011) Prostaglandin E2 and pain-an update. Biol Pharm Bull 34:1170–1173. https://doi.org/10.1248/bpb.34.1170
Chang YH, Lee ST, Lin WW (2001) Effects of cannabinoids on LPS-stimulated inflammatory mediator release from macrophages: involvement of eicosanoids. J Cell Biochem 81:715–723. https://doi.org/10.1002/jcb.1103
Panaro MA, Brandonisio O, Sisto M, Acquafredda A, Leogrande D, Fumarola L, Mitolo V (2001) Nitric oxide production by Leishmania-infected macrophages and modulation by prostaglandin E2. Clin Exp Med 1:137–143. https://doi.org/10.1007/s10238-001-8025-0
Levy D, Kubes P, Zochodne DW (2001) Delayed peripheral nerve degeneration, regeneration, and pain in mice lacking inducible nitric oxide synthase. J Neuropathol Exp Neurol 60:411–421. https://doi.org/10.1093/jnen/60.5.411
Levy D, Hoke A, Zochodne DW (1999) Local expression of inducible nitric oxide synthase in an animal model of neuropathic pain. Neurosci Lett 260:207–209. https://doi.org/10.1016/S0304-3940(98)00982-3
Ma WY, Quirion R (2006) Targeting invading macrophage-derived PGE2, IL-6 and calcitonin gene-related peptide in injured nerve to treat neuropathic pain. Expert Opin Ther Targets 10:533–546. https://doi.org/10.1517/14728222.10.4.533
Mester E, Spiry T, Szende B (1973) Effect of laser rays on incision healing. Bull Soc Int Chir 32:169–173
Seoane J, González-Mosquera A, López-Niño J, García-Caballero L, Aliste C, Seoane-Romero JM, Varela-Centelles P (2013) Er,Cr:YSGG laser therapy for oral leukoplakia minimizes thermal artifacts on surgical edges: a pilot study. Lasers Med Sci 28:1591–1597. https://doi.org/10.1007/s10103-013-1266-9
Lichtman MK, Otero-Vinas M, Falanga V (2016) Transforming growth factor beta (TGF-β) isoforms in incision healing and fibrosis. Incision Repair Regen 24:215–222. https://doi.org/10.1111/wrr.12398
Funding
This work was supported by the National Natural Science Foundation of China (No. 82071141) to X. H.
Author information
Authors and Affiliations
Contributions
Both the authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by M. O and X.H; The first draft of the manuscript was written by M.O and deeply revised by X. H. Both the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
All animal experiments were approved by the Animal Experimentation Committee of Beijing Friendship Hospital, Capital Medical University and were performed according to the institution's guidelines for the care and use of laboratory animals (No.20-2005). We complied with the Helsinki Declaration on animal experiment and the Hospital Review Board approved the study.
Conflict of interest
The authors have no conflict of interest to declare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ou, M., Huang, X. Histological evaluation of mouse tongue incisions after Er:YAG laser surgery with different pulse energies versus after conventional scalpel surgery. Lasers Med Sci 38, 181 (2023). https://doi.org/10.1007/s10103-023-03852-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-023-03852-9