Abstract
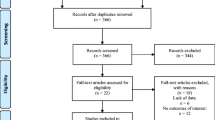
Tissue injuries that affect the skin and/or adjacent tissues and are usually over a bony prominence are called pressure injuries. The prevalence of these dysfunctions remains high, and despite technological advances, there is no consensus on the most appropriate treatment. The objective of this review was to evaluate the efficacy of photobiomodulation (PBM), ultrasound, and high-frequency electrophysical agents in the healing of pressure injuries in adults and the elderly. The search was conducted in the PubMed, Embase, Cochrane Library, Web of Science, and PEDro databases; in clinical trial records, a list of references of the selected articles, as well as through manual search (Google), of the last 5 years in humans in English and Portuguese. Nine thousand and sixty-seven studies were identified, 13 pre-selected, and 6 were included in this systematic review. PBM showed similar efficacy to other technologies indicated in other studies in healing pressure injuries. PBM with red wavelength (660 nm) in stages 2 and 3 pressure injuries effectively promoted healing compared to standard care. It was observed that the use of PBM accelerates tissue repair in pressure injuries; therapeutic ultrasound showed similar efficacy to other electrophysical agents but was effective in reducing the area of pressure injuries when comparing pre- and post-intervention. No clinical studies using the high-frequency electrophysical agent have been described in the last 5 years.


Similar content being viewed by others
References
Edsberg LE, Black JM, Goldberg M, McNichol L, Moore L, Sieggreen M (2016) Revised National Pressure Ulcer Advisory Panel pressure injury staging system. J Wound Ostomy Continence Nurs 43(6):585–597. https://doi.org/10.1097/WON.0000000000000281
Kayser SA, Vangilder CA, Ayello EA, Lachenbruch C (2018) Prevalence and analysis of medical device-related pressure injuries: results from the International Pressure Ulcer Prevalence Survey. Adv Skin Wound Care 31(6):276–285. https://doi.org/10.1097/01.ASW.0000532475.11971.aa
Brito PA, Generoso SV, Correia MITD (2013) Prevalence of pressure ulcers in hospitals in Brazil and association with nutritional status-a multicenter, cross-sectional study. Nutrition 29(4):646–649. https://doi.org/10.1016/j.nut.2012.11.008
Pereira ÂL, Bachion MM (2005) Tratamento de feridas: análise da produção científica publicada na Revista Brasileira de Enfermagem de 1970–2003. Rev Bras Enferm 58(2):208–213. https://doi.org/10.1590/s0034-71672005000200016
Qaseem A, Humphrey LL, Forciea MA, Starkey M, Denberg TD (2015) Treatment of pressure ulcers: a clinical practice guideline from the American College of Physicians. Ann Intern Med 162(5):370–379. https://doi.org/10.7326/M14-1568
Oliveira A, Simões S, Ascenso A, Reis CP (2022) Therapeutic advances in wound healing. J Dermatol Treat 33(1):2–22. https://doi.org/10.1080/09546634.2020.1730296
Ennis WJ, Lee C, Plummer M, Meneses P (2011) Current status of the use of modalities in wound care: electrical stimulation and ultrasound therapy. Plastic Reconstr Surg 127(SUPPL. 1 S):93–102. https://doi.org/10.1097/PRS.0b013e3181fbe2fd
Machado RS, Viana S, Sbruzzi G (2017) Low-level laser therapy in the treatment of pressure ulcers: systematic review. Lasers Med Sci 32(4):937–944. https://doi.org/10.1007/s10103-017-2150-9
Petz FFC, Félix JVC, Roehrs H, Pott FS, Stocco JGD, Marcos RL, Meier MJ (2020) Effect of photobiomodulation on repairing pressure ulcers in adult and elderly patients: a systematic review. Photochem Photobiol 96(1):191–199. https://doi.org/10.1111/php.13162
Karsli PB, Gurcay E, Karaahmet OZ, Cakci A (2017) High-voltage electrical stimulation versus ultrasound in the treatment of pressure ulcers. Adv Skin Wound Care 30(12):565–570. https://doi.org/10.1097/01.ASW.0000526606.72489.99
Fyfe MC, Bullock MI (1985) Therapeutic ultrasound: some historical background and development in knowledge of its effect on healing. Aust J Physiother 31(6):220–224
de Oliveira PD, Oliveira DAAP, Martinago CC, Frederico RCP, Soares CP, de Oliveira RF (2015) Effect of low-intensity pulsed ultrasound therapy on a fibroblasts cell culture. Fisioter Pesq 22(2):112–118. https://doi.org/10.0590/1809-2950/12860222022015
Cullum N, Liu Z (2017) Therapeutic ultrasound for venous leg ulcers. Cochrane Database Syst Rev 5:CD001180. https://doi.org/10.1002/14651858.CD001180.pub4
Korelo RIG, Fernandes LC (2017) Ultrassom terapêutico para cicatrização de feridas: revisão sistemática. ConScientiae Saúde 15(3):518–529. https://doi.org/10.5585/conssaude.v15n3.6421
Gupta A (2018) Augmenting wound healing with photobiomodulation therapy, Chap 10; 135–146. In Hamblin MR, Ferraresi C, Huang Y, de Freitas LF, Carroll JD. Low-Level Light Therapy: Photobiomodulation. Tutorial Texts in Optical Engineering Volume TT115; Ed. Spie Press, Bellingham, Washington USA,p. 390.
Mosca RC, Ong AA, Albasha O, Bass K, Arany P (2019) Photobiomodulation therapy for wound care: a potent, noninvasive, photoceutical approach. Adv Skin Wound Care 32(4):157–167. https://doi.org/10.1097/01.ASW.0000553600.97572.d2
de Lucas B, Pérez LM, Bernal A, Gálvez BG (2020) Ultrasound therapy: experiences and perspectives for regenerative medicine. Genes 11(1086):2–20. https://doi.org/10.3390/genes11091086
Yadollahpour A, Mostafa J, Samaneh R, Zohreh R (2014) Ultrasound therapy for wound healing: a review of current techniques and mechanisms of action. J Pure Appl Microbiol 8(5):4071–4085
Leng X, Shang J, Gao D, Wu J (2018) Low-intensity pulsed ultrasound promotes proliferation and migration of HaCaT keratinocytes through the PI3K/AKT and JNK pathways. Braz J Med Biol Res 51(12):e7862. https://doi.org/10.1590/1414-431X20187862
Goyal M, Kothiyal S (2021) Efficacy of deep tissue laser therapy in pressure ulcer healing in patient with quadriplegia: case report. J Physiother Res 11(3):593–598. https://doi.org/10.17267/2238-2704rpf.v11i3.3784
Macedo SPR, Mota MSA, Fagundes CF, de Souza MR, Navarro RS (2021) Effects of photobiomodulation in the treatment of pressure ulcers: integrative review. Res Soc Dev 10(2):e32810212597. https://doi.org/10.33448/rsd-v10i2.12597
Silva JRM, Fernandes MAL, Neiva LM (2021) Comparative analysis of the effects of low power laser on the healing of skin lesions: a systematic review. Braz J Health Rev 4(3):13949–13960. https://doi.org/10.34119/bjhrv4n3-330
Lu Q, Yin Z, Shen X, Li J, Su P, Feng M, Xu X, Li W, He C, Shen Y (2021) Clinical effects of high-intensity laser therapy on patients with chronic refractory wounds: a randomized controlled trial. BMJ Open 11:e045866. https://doi.org/10.1136/bmjopen-2020-045866
Romanelli M, Piaggesi A, Scapagnini G, Dini V, Janowska A, Iacopi E, Scarpa C, Fauverghe S, Bassetto F (2017) EUREKA study - The evaluation of real-life use of a biophotonic system in chronic wound management: an interim analysis. Drug Des Dev Ther 11:3551–3558. https://doi.org/10.2147/DDDT.S142580
Polak A, Taradaj J, Nawrat-Szoltysik A, Stania M, Dolibog P, Blaszczak E, Zarzeczny R, Juras G, Franek A, Kucio C (2016) Reduction of pressure ulcer size with high-voltage pulsed current and high-frequency ultrasound: a randomized trial. J Wound Care 25(12):742–754. https://doi.org/10.12968/jowc.2016.25.12.742
Ruh AC, Frigo L, Cavalcanti MFXB, Svidnicki P, Vicari VN, Lopes-Martins RAB, Leal ECP, De Isla N, Diomede F, Trubiani O, Favero GM (2018) Laser photobiomodulation in pressure ulcer healing of human diabetic patients: gene expression analysis of inflammatory biochemical markers. Lasers Med Sci 33(1):165–171. https://doi.org/10.1007/s10103-017-2384-6
Bortoli I, Prado AL, Kroth A (2016) A efetividade do laser associado a diferentes tipos de curativos na cicatrização de úlceras de pressão. 16 (1), Evidência, Ciência e Biotecnologia 45–58. https://doi.org/10.18593/eba.v16i1.9774
Chaves MEA, Silva FS, Soares VPC, Ferreira RAM, Gomes FSL, Andrade RM, Pinotti M (2015) Evaluation of healing of pressure ulcers through thermography: a preliminary study. Res Biomed Eng 31(1):3–9. https://doi.org/10.1590/2446-4740.0571
Chaves MEA, Piancastelli ACC, Araujo AR, Pinotti M (2014) Effects of low-power light therapy on wound healing. An Bras Dermatol 89(4):616–623
Fitzpatrick RB (2008) PEDro: A physiotherapy evidence database. Med Ref Serv Q 27(2):188–197. https://doi.org/10.1080/02763860802114397
Delavary BM, Van Der Veer WM, Van Egmond M, Niessen FB, Beelen RHJ (2011) Macrophages in skin injury and repair. Immunobiology 216(7):753–762. https://doi.org/10.1016/j.imbio.2011.01.001
Arora M, Harvey LA, Glinsky JV, Nier L, Lavrencic L, Kifley A, Cameron ID (2020) Electrical stimulation for treating pressure ulcers. Cochrane Database Syst Rev 2020(1). https://doi.org/10.1002/14651858.CD012196.pub2
Coltro PS, Ferreira MC, Batista BPSN, Nakamoto HA, Milcheski DA, Tuma Júnior P (2010) Tratamento cirúrgico das feridas complexas: experiência da cirurgia plástica no Hospital das Clínicas da FMUSP TT - Surgical treatment of complex wounds: experience of plastic surgery in the “Hospital das Clínicas – FMUSP”. Rev. Med. (Säo Paulo), 89(3/4), 153–157. http://www.revistas.usp.br/revistadc/article/view/46290/49946
Das Neves LMS, Guirro ECO, Albuquerque FLA, Marcolino AM (2016) Effects of high-voltage electrical stimulation in improving the viability of musculocutaneous flaps in rats. Ann Plast Surg 77(4):e50–e54. https://doi.org/10.1097/SAP.0000000000000621
Korelo RIG, Oliveira JJJ, Souza RSA, Hullek RF, Fernandes LC (2013) Gerador de alta frequência como recurso para tratamento de úlceras por pressão: estudo piloto. Fisioterapia Em Movimento 26(4):715–724. https://doi.org/10.1590/s0103-51502013000400002
Chen C, Hou WH, Chan ES, Yeh ML, Lo HL (2014) Phototherapy for treating pressure ulcers. Cochrane Database Syst Rev 11(7):CD009224. https://doi.org/10.1002/14651858.CD009224.pub2
Al-Wattar WM, Abdulluh BH, Mahmmod AS (2013) Irradiation effect of 780–805nm diode laser on wound healing in mice. J Bagh College Dentistry 25(1):48–52
Hendler KG, Canever JB, de Souza LG, das Neves LMS, Fonseca MCR, Kuriki HU, Aguiar Junior AS, Barbosa RI, Marcolino AM (2021) Comparison of photobiomodulation in the treatment of skin injury with an open wound in mice. Lasers Med Sci 36:1845–1854. https://doi.org/10.1007/s10103-020-03216-7
Silveira PCL, Ferreira KB, Rocha FR, Pieri BLS, Pedroso GS, De Souza CT, Nesi RT, Pinho RA (2016) Effect of low-power laser (LPL) and light-emitting diode (LED) on inflammatory response in burn wound healing. Inflammation 39(4):1395–1404. https://doi.org/10.1007/s10753-016-0371-x
Brauncajs M, Ksiąszczyk K, Lewandowska-Polak A, Gorzela K, Grzegorczyk J (2018) Impact of low-level laser therapy on the dynamics of pressure ulcer-induced changes considering an infectious agent and cathelicidin LL-37 concentration: a preliminary study. Adv Dermatol Allergol 35(6):582–586. https://doi.org/10.5114/ada.2018.77609
Andrade FSSD, Clark RMO, Ferreira ML (2014) Efeitos da laserterapia de baixa potência na cicatrização de feridas cutâneas. Revista Do Colegio Brasileiro de Cirurgioes 41(2):129–133. https://doi.org/10.1590/s0100-69912014000200010
Greatrex-White S, Moxey H (2015) Wound assessment tools and nurses’ needs: an evaluation study. Int Wound J 12(3):293–301. https://doi.org/10.1111/iwj.12100
Santo PFE, de Almeida SA, Silveira MM, Salomé GM, Ferreira LM (2013) Use of the Pressure Ulcer Scale for Healing tool to evaluate the healing of chronic leg ulcers. Rev Bras Cir Plásti 28(1):133–141
Iizaka S, Kaitani T, Sugama J, Nakagami G, Naito A, Koyanagi H, Konya C, Sanada H (2013) Predictive validity of granulation tissue color measured by digital image analysis for deep pressure ulcer healing: a multicenter prospective cohort study. Wound Repair Regen 21(1):25–34. https://doi.org/10.1111/j.1524-475X.2012.00841.x
Bates-Jensen BM, McCreath HE, Harputlu D, Patlan A (2020) Reliability of the Bates-Jensen wound assessment tool for pressure injury assessment: the pressure ulcer detection study. HHS Public Access 27(4):386–395. https://doi.org/10.1111/wrr.12714
Kavros SJ, Liedl DA, Boon AJ, Miller JL, Hobbs JA, Andrews KL (2008) Expedited wound healing with noncontact, low-frequency ultrasound therapy in chronic wounds: a retrospective analysis. Adv Skin Wound Care 21(9):416–423. https://doi.org/10.1097/01.ASW.0000323546.04734.31
Beheshti A, Shafigh Y, Parsa H, Zangivand AA (2014) Comparison of high-frequency and MIST ultrasound therapy for the healing of venous leg ulcers. Adv Clin Exp Med 23(6):969–975. https://doi.org/10.17219/acem/37353
Cullum N, Nelson EA, Flemming K, Sheldon T (2001) Systematic reviews of wound care management: (5) beds; (6) compression; (7) laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy. Health Technol Assess 5(9). https://doi.org/10.3310/hta5090
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Registration number
The present study was approved by the PROSPERO and is registered under CRD42020178792 and can be accessed at https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=178792.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vieceli, A.S., Martins, J.C., Hendler, K.G. et al. Effectiveness of electrophysical agents for treating pressure injuries: a systematic review. Lasers Med Sci 37, 3363–3377 (2022). https://doi.org/10.1007/s10103-022-03648-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-022-03648-3