Abstract
Introduction
Onychomycosis is a common fungal infection of the nail. Laser and topical antifungal agent combination therapy is an emerging treatment for onychomycosis. The objective of this study was to systematically evaluate the efficacy and safety of laser and topical antifungal agent combination therapy for onychomycosis.
Methods
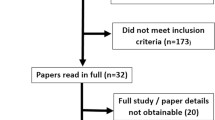
The PubMed, Embase, Cochrane Library, China National Knowledge Infrastructure, Wanfang and VIP databases were searched from inception to November 2021. Randomised controlled trials (RCTs) on laser therapy combined with topical antifungal agents for onychomycosis were included. The Cochrane Collaboration tool was used to assess the risk of bias, and Revman 5.3 software was used in the meta-analysis.
Results
Twelve studies involving 869 patients were included in this meta-analysis. The results showed that compared with topical antifungal agents alone, laser and topical antifungal agent combination therapy was superior in terms of the complete cure rate (RR 6.04,95% CI (2.17, 16.85), P = 0.0006), mycological cure rate (RR 1.27, 95% CI (1.10, 1.48), P = 0.001), clinical effective rate (RR 1.38, 95% CI (1.20, 1.57), P < 0.00001) and patient satisfaction rate (RR 1.47,95% CI (1.17, 1.84), P = 0.0009).The subgroup analysis of outcome indicators, including mycological cure rate and clinical effective rate, demonstrated that both carbon dioxide (CO2) laser therapy combined with topical antifungal therapy and 1064-nm neodymium-doped:yttrium aluminium garnet (Nd:YAG) laser therapy combined with topical antifungal therapy showed better results than topical antifungal therapy alone. No adverse events were identified except for three studies reporting transient burning sensation without treatment and mild to moderate pain, both of which were well tolerated.
Conclusion
The present study indicated that laser and topical antifungal agent combination therapy is effective for onychomycosis. However, more large-scale and well-designed RCTs are warranted.





Similar content being viewed by others
References
Lipner SR, Scher RK (2019) Onychomycosis: clinical overview and diagnosis. J Am Acad Dermatol 80(4):835–851. https://doi.org/10.1016/j.jaad.2018.03.062
Gupta AK, Stec N, Summerbell RC, Shear NH, Piguet V, Tosti A, Piraccini BM (2020) Onychomycosis: a review. J Eur Acad Dermatol Venereol 34(9):1972–1990. https://doi.org/10.1111/jdv.16394
Ghannoum MA, Hajjeh RA, Scher R, Konnikov N, Gupta AK, Summerbell R, Sullivan S, Daniel R, Krusinski P, Fleckman P, Rich P, Odom R, Aly R, Pariser D, Zaiac M, Rebell G, Lesher J, Gerlach B, Ponce-De-Leon GF, Ghannoum A, Warner J, Isham N, Elewski B (2020) A large-scale North American study of fungal isolates from nails: the frequency of onychomycosis, fungal distribution, and antifungal susceptibility patterns. J Am Acad Dermatol 43(4):641–648. https://doi.org/10.1067/mjd.2000.107754
Lipner SR, Scher RK (2014) Onychomycosis: current and investigational therapies. Cutis 94:E21–E24
Crawford F, Young P, Godfrey C, Bell-Syer SE, Hart R, Brunt E, Russell I (2002) Oral treatments for toenail onychomycosis: a systematic review. Arch Dermatol 138(6):811–816. https://doi.org/10.1001/archderm.138.6.811
Ameen M, Lear JT, Madan V, Mohd Mustapa MF, Richardson M (2014) British Association of Dermatologists’ guidelines for the management of onychomycosis. Br J Dermatol 171(5):937–958. https://doi.org/10.1111/bjd.13358
Aggarwal R, Targhotra M, Kumar B, Sahoo PK, Chauhan MK (2020) Treatment and management strategies of onychomycosis. J Mycol Med 30(2):100949. https://doi.org/10.1016/j.mycmed.2020.100949
Elewski BE, Rich P, Pollak R, Pariser DM, Watanabe S, Senda H, Ieda C, Smith K, Pillai R, Ramakrishna T, Olin JT (2013) Efinaconazole 10% solution in the treatment of toenail onychomycosis: two phase III multicenter, randomized, double-blind studies. J Am Acad Dermatol 68(4):600–608. https://doi.org/10.1016/j.jaad.2012.10.013
Gupta AK, Venkataraman M, Anbalagan N, Guenin EP (2021) One size does not fit all: the need for individualized treatment based on factors that may affect the therapeutic outcome of efinaconazole 10% solution for the treatment of toenail onychomycosis. Int J Dermatol 60(10):1296–1302. https://doi.org/10.1111/ijd.15739
Yeung K, Ortner VK, Martinussen T, Paasch U, Haedersdal M (2019) Efficacy of laser treatment for onychomycotic nails: a systematic review and meta-analysis of prospective clinical trials. Lasers Med Sci 34(8):1513–1525. https://doi.org/10.1007/s10103-019-02802-8
FDA. (2016) Medical devices and clinical trial design for the treatment or improvement in the appearance of fungally-infected nails; draft guidance for Industry and Food and Drug Administration Staff; Availability. 81(44):29
Gupta AK, Mays RR, Versteeg SG, Shear NH, Piguet V (2018) Update on current approaches to diagnosis and treatment of onychomycosis. Expert Rev Anti Infect Ther 16(12):929–938. https://doi.org/10.1080/14787210.2018.1544891
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269, W64. https://doi.org/10.7326/0003-4819-151-4-200908180-00135
Han Y, Wang Y, Zhang XR, Chen J, Li XD (2021) The effects of CO2 laser and topical agent combination therapy for onychomycosis: a meta-analysis. Dermatol Ther 34(6):e15136. https://doi.org/10.1111/dth.15136
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (2019) Cochrane handbook for systematic reviews of interventions, 2nd edn. John Wiley & Sons, Chichester
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, Jaeschke R, Rind D, Meerpohl J, Dahm P, Schunemann HJ (2011) GRADE guidelines:1. Introduction-GRADE evidence profles and summary of fndings tables. J Clin Epidemiol 64(4):383–394. https://doi.org/10.1016/j.jclinepi.2010.04.026
Wang JH, Jia YQ, Chen YL, Wang YP (2019) Effect of lattice carbon dioxide laser combined with local medication on treating onychomycosis. J Clin Med Pract 23(7):32–36
Jing WW, Liang YH, Zhou YA (2018) Clinical efficacy of fractional CO2 laser combined with naftifine hydrochloride and ketoconazole cream for the treatment of onychomycosis. China Med Cosmet 263(11):46–49. https://doi.org/10.15909/j.cnki.cn61-1347/r.002686
Bonhert K, Dorizas A, Sadick NS (2019) Efficacy of combination therapy with efinaconazole 10% solution and 1064 nm Nd:YAG laser for treatment of toenail onychomycosis. J Cosmet Laser Ther 21(3):179–183. https://doi.org/10.1080/14764172.2018.1502451
Bunyaratavej S, Wanitphakdeedecha R, Ungaksornpairote C, Kobwanthanakun W, Chanyachailert P, Nokdhes YN, Patthamalai P, Tantrapornpong P, Suphatsathienkul P, Kiratiwongwan R, Limphoka P, Leeyaphan C (2020) Randomized controlled trial comparing long-pulsed 1064-Nm neodymium: Yttrium-aluminum-garnet laser alone, topical amorolfine nail lacquer alone, and a combination for nondermatophyte onychomycosis treatment. J Cosmet Dermatol 19(9):2333–2338. https://doi.org/10.1111/jocd.13291
Song ZJ, Li Z (2016) Clinical efficacy of long-pulsed 1064nm laser combined with amorolfine hydrochloride in the treatment of patients with onychomycosis. China Pharm 19(10):1919–1921
Zhang XL, Zhang HP, Yang LJ (2016) Observation of efficacy of CO2 laser combined with amorolfine hydrochloride liniment in treatment of 27 patients with onychomycosis. China Med Cosmet 25(5):74–76. https://doi.org/10.15909/j.cnki.cn61-1347/r.001157
Kim TI, Shin MK, Jeong KH, Suh DH, Lee SJ, Oh IH, Lee MH (2016) A randomised comparative study of 1064 nm neodymium-doped yttrium aluminium garnet (Nd:YAG) laser and topical antifungal treatment of onychomycosis. Mycoses 59(12):803–810. https://doi.org/10.1111/myc.12534
Rajbanshi B, Shen L, Jiang M, Gao Q, Huang X, Ma J, Wang J, Hu Y, Lv H, Wu X, Zhao J (2020) Comparative study of traditional ablative CO2 laser-assisted topical antifungal with only topical antifungal for treating onychomycosis: a multicenter study. Clin Drug Investig 40(6):575–582. https://doi.org/10.1007/s40261-020-00914-6
Liu Q, Zheng KP, Jiang S, Ling P (2021) Clinical efficacy of CO2 fractional laser combined with topical amorolfine cream in the treatment of superficial white onychomycosis and distal and lateral subungual onychomycosis. Cnki.net. https://kns.cnki.net/kcms/detail/42.1677.R.20210930.1324.001.html. Accessed 07 October 2021. https://doi.org/10.14188/j.1671-8852.2021.0263
Bi XD, Song MA, Zhai L (2015) The efficacy of 1064nm long-pulse laser combined with amorolfine regimen for patients with onychomycosis. China J Derm Venereol 29(5):475–477. https://doi.org/10.13735/j.cjdv.1001-7089.201408134
Zaki AM, Abdo HM, Ebadah MA, Ibrahim SM (2020) Fractional CO2 laser plus topical antifungal versus fractional CO2 laser versus topical antifungal in the treatment of onychomycosis. Dermatol Ther 33(1):e13155. https://doi.org/10.1111/dth.13155
Zhang J, Zhang Y, Qin J, Lu S, Cai W, Li J, Huang H, Yang S, Xi L (2021) Comparison of a fractional 2940-nm Er:YAG laser and 5% amorolfine lacquer combination therapy versus a 5% amorolfine lacquer monotherapy for the treatment of onychomycosis: a randomized controlled trial. Lasers Med Sci 36(1):147–152. https://doi.org/10.1007/s10103-020-03054-7
Dars S, Banwell HA, Matricciani L (2019) The use of urea for the treatment of onychomycosis: a systematic review. J Foot Ankle Res 12:22. https://doi.org/10.1186/s13047-019-0332-3
Morais OO, Costa IM, Gomes CM, Shinzato DH, Ayres GM, Cardoso RM (2013) The use of the Er:YAG 2940nm laser associated with amorolfine lacquer in the treatment of onychomycosis. An Bras Dermatol 88(5):847–849. https://doi.org/10.1590/abd1806-4841.20131932
Shi J, Li J, Huang H, Permatasari F, Liu J, Xu Y, Wu D, Zhou BR, Luo D (2017) The efficacy of fractional carbon dioxide (CO 2) laser combined with terbinafine hydrochloride 1% cream for the treatment of onychomycosis. J Cosmet Laser Ther 19(6):353–359. https://doi.org/10.1080/14764172.2017.1334925
Gupta AK, Foley KA, Versteeg SG (2017) Lasers for onychomycosis. J Cutan Med Surg 21(2):114–116. https://doi.org/10.1177/1203475416677722
Zhang RN, Zhao JY, Li LF (2020) Morphological and transcriptome analyses provide insights into growth inhibition of trichophyton rubrum caused by laser irradiation. Evid Based Complement Alternat Med 2020:6052461. https://doi.org/10.1155/2020/6052461
El-Tatawy RA, Aliweh HA, Hegab DS, Talaat RAZ, Shams Eldeen MA (2019) Fractional carbon dioxide laser and topical tioconazole in the treatment of fingernail onychomycosis. Lasers Med Sci 34(9):1873–1880. https://doi.org/10.1007/s10103-019-02789-2
Kreutz T, de Matos SP, Koester LS (2019) Recent patents containing permeation enhancers for nail delivery. Recent Pat Drug Deliv Formul 13(3):203–218. https://doi.org/10.2174/1872211313666191030155837
Guan XH, Xu TH, Chen X, Mu QS, Suo JF, Xu RX, Chen J, Xiao T, Hua GX, Chen HD (2021) Fractionated carbon dioxide (CO2) laser treatment contributes to trans-nail penetration of rhodamine B and changes of cytokine microenvironment. Lasers Med Sci 36(8):1619–1623. https://doi.org/10.1007/s10103-020-03232-7
Imrigha NAA, Bidin N, Lau PS, Musa N, Zakaria N, Krishnan G (2017) Photobiomodulation therapy on wound treatment subsequent to Q-switched Nd: YAG laser tattoo removal in rat model. J Biophotonics 10(10):1287–1291. https://doi.org/10.1002/jbio.201600295
Nestor M, Andriessen A, Berman B, Katz BE, Gilbert D, Goldberg DJ, Gold MH, Kirsner RS, Lorenc PZ (2017) Photobiomodulation with non-thermal lasers: mechanisms of action and therapeutic uses in dermatology and aesthetic medicine. J Cosmet Laser Ther 19(4):190–198. https://doi.org/10.1080/14764172.2017.1293828
Elewski BE, Ghannoum MA, Mayser P, Gupta AK, Korting HC, Shouey RJ, Baker DR, Rich PA, Ling M, Hugot S, Damaj B, Nyirady J, Thangavelu K, Notter M, Parneix-Spake A, Sigurgeirsson B (2013) Efficacy, safety and tolerability of topical terbinafine nail solution in patients with mild-to-moderate toenail onychomycosis: results from three randomized studies using double-blind vehicle-controlled and open-label active-controlled designs. J Eur Acad Dermatol Venereol 27(3):287–294. https://doi.org/10.1111/j.1468-3083.2011.04373.x
Ricardo JW, Lipner SR (2020) Safety of current therapies for onychomycosis. Expert Opin Drug Saf 19(11):1395–1408. https://doi.org/10.1080/14740338.2020.1829592
Ma W, Si C, Kasyanju Carrero LM, Liu HF, Yin XF, Liu J, Xu Y, Zhou B (2019) Laser treatment for onychomycosis: a systematic review and meta-analysis. Medicine (Baltimore) 98(48):e17948. https://doi.org/10.1097/MD.0000000000017948
Funding
This work was supported by the Tianjin Municipal Health Commission-Research Projects in Key Areas of Traditional Chinese Medicine (grant no.2019002), Tianjin Municipal Health Commission Health Science and Technology Project (grant no. zc20127).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, J., Lin, P., Li, J. et al. Efficacy of laser therapy combined with topical antifungal agents for onychomycosis: a systematic review and meta-analysis of randomised controlled trials. Lasers Med Sci 37, 2557–2569 (2022). https://doi.org/10.1007/s10103-022-03561-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-022-03561-9