Abstract
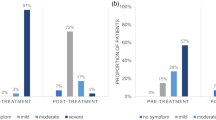
Evaluate the improvement in clinical signs and symptoms in patients with moderate-to-severe meibomian gland dysfunction (MGD) treated with intense pulsed light (IPL) using an acne filter. A retrospective chart review of 70 eyes of 35 patients with moderate-to-severe MGD treated with IPL using the acne filter was performed. IPL treatment was administered using the acne filter four times at 2- to 3-week intervals to upper and lower eyelids. We evaluated tear break-up time (TBUT), matrix metalloproteinase (MMP)-9, Sjögren’s International Clinical Collaborative Alliance (SICCA) staining score, and Oxford staining grade. We performed Schirmer’s test I without topical anesthesia, slit-lamp microscopic examination of lid margin and meibomian gland, and patient’s symptom score assessment and evaluated the incidence of adverse effects in the ocular and periocular areas at baseline and 30 days after the final treatment. Significant improvements (P < 0.001) were observed in TBUT, SICCA staining score, Oxford staining grade, quality of meibum, consistency of meibum, lid margin telangiectasia, MGD grade, and patient’s symptom scores after acne filter IPL treatment. Furthermore, the positivity (100 to 71.43%, P = 0.002) and level (2.43 ± 0.98 to 1.14 ± 0.78, P < 0.001) of MMP-9 significantly decreased after treatment. However, there was no significant improvement in Schirmer’s test I (P = 0.224). No systemic or regional adverse effects were observed in any patient. IPL treatment using the acne filter is an effective and safe therapeutic modality for treating moderate-to-severe MGD, especially for lid margin telangiectasia and MMP-9.


Similar content being viewed by others
Data availability
The data used to support the findings of this study are available from the corresponding author upon request.
Code availability
Not applicable.
References
Knop E, Knop N, Millar T, Obata H, Sullivan DA (2011) The international workshop on meibomian gland dysfunction: report of the subcommittee on anatomy, physiology, and pathophysiology of the meibomian gland. Invest Ophthalmol Vis Sci 52(4):1938–1978
Eom Y, Na KS, Cho KJ, Hwang HS, Kim SW, Chung TY et al (2019) Distribution and characteristics of meibomian gland dysfunction subtypes: a multicenter study in South Korea. Korean J Ophthalmol 33(3):205–213
Nelson JD, Shimazaki J, Benitez-del-Castillo JM, Craig JP, McCulley JP, Den S et al (2011) The international workshop on meibomian gland dysfunction: report of the definition and classification subcommittee. Invest Ophthalmol Vis Sci 52(4):1930–1937
Goto E, Monden Y, Takano Y, Mori A, Shimmura S, Shimazaki J et al (2002) Treatment of non-inflamed obstructive meibomian gland dysfunction by an infrared warm compression device. Br J Ophthalmol 86(12):1403–1407
Arita R, Suehiro J, Haraguchi T, Maeda S, Maeda K, Tokoro H et al (2013) Topical diquafosol for patients with obstructive meibomian gland dysfunction. Br J Ophthalmol 97(6):725–729
Epstein IJ, Rosenberg E, Stuber R, Choi MB, Donnenfeld ED, Perry HD (2020) Double-masked and unmasked prospective study of terpinen-4-ol lid scrubs with microblepharoexfoliation for the treatment of demodex blepharitis. Cornea 39(4):408–416
Tauber J (2020) A 6-week, prospective, randomized, single-masked study of lifitegrast ophthalmic solution 5% versus thermal pulsation procedure for treatment of inflammatory meibomian gland dysfunction. Cornea 39(4):403–407
Lee H, Chung B, Kim KS, Seo KY, Choi BJ, Kim TI (2014) Effects of topical loteprednol etabonate on tear cytokines and clinical outcomes in moderate and severe meibomian gland dysfunction: randomized clinical trial. Am J Ophthalmol 158(6):1172-1183.e1171
Lee H, Min K, Kim EK, Kim TI (2012) Minocycline controls clinical outcomes and inflammatory cytokines in moderate and severe meibomian gland dysfunction. Am J Ophthalmol 154(6):949-957.e941
Lee H, Kim M, Park SY, Kim EK, Seo KY, Kim TI (2017) Mechanical meibomian gland squeezing combined with eyelid scrubs and warm compresses for the treatment of meibomian gland dysfunction. Clin Exp Optom 100(6):598–602
Yoo SE, Lee DC, Chang MH (2005) The effect of low-dose doxycycline therapy in chronic meibomian gland dysfunction. Korean J Ophthalmol 19(4):258–263
Lienert JP, Tarko L, Uchino M, Christen WG, Schaumberg DA (2016) Long-term natural history of dry eye disease from the patient’s perspective. Ophthalmology 123(2):425–433
Alves M, Fonseca EC, Alves MF, Malki LT, Arruda GV, Reinach PS et al (2013) Dry eye disease treatment: a systematic review of published trials and a critical appraisal of therapeutic strategies. Ocul Surf 11(3):181–192
Moon SY, Han SA, Kwon HJ, Park SY, Lee JH, Chung HS et al (2021) Effects of lid debris debridement combined with meibomian gland expression on the ocular surface MMP-9 levels and clinical outcomes in moderate and severe meibomian gland dysfunction. BMC Ophthalmol 21(1):175
Toyos R, McGill W, Briscoe D (2015) Intense pulsed light treatment for dry eye disease due to meibomian gland dysfunction; a 3-year retrospective study. Photomed Laser Surg 33(1):41–46
Vora GK, Gupta PK (2015) Intense pulsed light therapy for the treatment of evaporative dry eye disease. Curr Opin Ophthalmol 26(4):314–318
Craig JP, Chen YH, Turnbull PR (2015) Prospective trial of intense pulsed light for the treatment of meibomian gland dysfunction. Invest Ophthalmol Vis Sci 56(3):1965–1970
Arita R, Fukuoka S, Morishige N (2019) Therapeutic efficacy of intense pulsed light in patients with refractory meibomian gland dysfunction. Ocul Surf 17(1):104–110
Raulin C, Greve B, Grema H (2003) IPL technology: a review. Lasers Surg Med 32(2):78–87
Dell SJ (2017) Intense pulsed light for evaporative dry eye disease. Clin Ophthalmol 11:1167–1173
Lee H, Han YE, Park SY, Lee JH, Chung HS, Moon SY et al (2021) Changes in the expression of matrix metalloproteinase-9 after intense pulsed light therapy combined with meibomian gland expression in moderate and severe meibomian gland dysfunction. Cont Lens Anterior Eye 44(3):101339
Nichols KK, Foulks GN, Bron AJ, Glasgow BJ, Dogru M, Tsubota K et al (2011) The international workshop on meibomian gland dysfunction: executive summary. Invest Ophthalmol Vis Sci 52(4):1922–1929
Tomlinson A, Bron AJ, Korb DR, Amano S, Paugh JR, Pearce EI et al (2011) The international workshop on meibomian gland dysfunction: report of the diagnosis subcommittee. Invest Ophthalmol Vis Sci 52(4):2006–2049
Roberts WE (2009) Skin type classification systems old and new. Dermatol Clin 27(4):529–533
Arita R, Mizoguchi T, Fukuoka S, Morishige N (2018) Multicenter study of intense pulsed light therapy for patients with refractory meibomian gland dysfunction. Cornea 37(12):1566–1571
Rasmussen A, Ice JA, Li H, Grundahl K, Kelly JA, Radfar L et al (2014) Comparison of the American-European Consensus Group Sjogren’s syndrome classification criteria to newly proposed American College of Rheumatology criteria in a large, carefully characterised sicca cohort. Ann Rheum Dis 73(1):31–38
Whitcher JP, Shiboski CH, Shiboski SC, Heidenreich AM, Kitagawa K, Zhang S et al (2010) A simplified quantitative method for assessing keratoconjunctivitis sicca from the Sjogren’s Syndrome International Registry. Am J Ophthalmol 149(3):405–415
Arita R, Minoura I, Morishige N, Shirakawa R, Fukuoka S, Asai K et al (2016) Development of definitive and reliable grading scales for meibomian gland dysfunction. Am J Ophthalmol 169:125–137
Shimazaki J, Sakata M, Tsubota K (1995) Ocular surface changes and discomfort in patients with meibomian gland dysfunction. Arch Ophthalmol 113(10):1266–1270
Green-Church KB, Butovich I, Willcox M, Borchman D, Paulsen F, Barabino S et al (2011) The international workshop on meibomian gland dysfunction: report of the subcommittee on tear film lipids and lipid-protein interactions in health and disease. Invest Ophthalmol Vis Sci 52(4):1979–1993
Stahl U, Willcox M, Stapleton F (2012) Osmolality and tear film dynamics. Clin Exp Optom 95(1):3–11
Baudouin C (2007) A new approach for better comprehension of diseases of the ocular surface. J Fr Ophtalmol 30(3):239–246
Mudgil P (2014) Antimicrobial role of human meibomian lipids at the ocular surface. Invest Ophthalmol Vis Sci 55(11):7272–7277
Borchman D, Foulks GN, Yappert MC, Milliner SE (2012) Differences in human meibum lipid composition with meibomian gland dysfunction using NMR and principal component analysis. Invest Ophthalmol Vis Sci 53(1):337–347
Graham JE, Moore JE, Jiru X, Moore JE, Goodall EA, Dooley JS et al (2007) Ocular pathogen or commensal: a PCR-based study of surface bacterial flora in normal and dry eyes. Invest Ophthalmol Vis Sci 48(12):5616–5623
Baudouin C, Messmer EM, Aragona P, Geerling G, Akova YA, Benitez-del-Castillo J et al (2016) Revisiting the vicious circle of dry eye disease: a focus on the pathophysiology of meibomian gland dysfunction. Br J Ophthalmol 100(3):300–306
Xue AL, Wang MTM, Ormonde SE, Craig JP (2020) Randomised double-masked placebo-controlled trial of the cumulative treatment efficacy profile of intense pulsed light therapy for meibomian gland dysfunction. Ocul Surf 18(2):286–297
Ash C, Dubec M, Donne K, Bashford T (2017) Effect of wavelength and beam width on penetration in light-tissue interaction using computational methods. Lasers Med Sci 32(8):1909–1918
Jiang X, Wang Y, Lv H, Liu Y, Zhang M, Li X (2018) Efficacy of intra-meibomian gland injection of the anti-VEGF agent bevacizumab for the treatment of meibomian gland dysfunction with lid-margin vascularity. Drug Des Devel Ther 12:1269–1279
Kaufman HE (2013) The practical detection of mmp-9 diagnoses ocular surface disease and may help prevent its complications. Cornea 32(2):211–216
Chotikavanich S, de Paiva CS, de Li Q, Chen JJ, Bian F, Farley WJ et al (2009) Production and activity of matrix metalloproteinase-9 on the ocular surface increase in dysfunctional tear syndrome. Invest Ophthalmol Vis Sci 50(7):3203–3209
Ruan F, Zang Y, Sella R, Lu H, Li S, Yang K et al (2019) Intense pulsed light therapy with optimal pulse technology as an adjunct therapy for moderate to severe blepharitis-associated keratoconjunctivitis. J Ophthalmol 2019:3143469
Cheng SN, Jiang FG, Chen H, Gao H, Huang YK (2019) Intense pulsed light therapy for patients with meibomian gland dysfunction and ocular demodex infestation. Curr Med Sci 39(5):800–809
Ibrahimi OA, Avram MM, Hanke CW, Kilmer SL, Anderson RR (2011) Laser hair removal. Dermatol Ther 24(1):94–107
Alexis AF (2013) Lasers and light-based therapies in ethnic skin: treatment options and recommendations for Fitzpatrick skin types V and VI. Br J Dermatol 169(Suppl 3):91–97
Lee WW, Murdock J, Albini TA, O’Brien TP, Levine ML (2011) Ocular damage secondary to intense pulse light therapy to the face. Ophthalmic Plast Reconstr Surg 27(4):263–265
Pang AL, Wells K (2008) Bilateral anterior uveitis after intense pulsed light therapy for pigmented eyelid lesions. Dermatol Surg 34(9):1276–1279
Javey G, Schwartz SG, Albini TA (2010) Ocular complication of intense pulsed light therapy: iris photoablation. Dermatol Surg 36(9):1466–1468
Funding
This work was supported by the Korea Medical Device Development Fund, granted by the Korean government (the Ministry of Science and ICT, the Ministry of Trade, Industry, and Energy; the Ministry of Health and Welfare; the Ministry of Food and Drug Safety) (Project Number: 9991006821, KMDF_PR_20200901_0148), by Korean Fund for Regenerative Medicine funded by Ministry of Science and ICT, and Ministry of Health and Welfare (HH21C0012, Republic of Korea), and by a grant from the Asan Institute for Life Sciences, Asan Medical Center, Seoul, Korea (2021IP0059-1, 2021IP0061-1).
Author information
Authors and Affiliations
Contributions
JYH: Concept and study design. Data collection. Data interpretation. Data analysis and statistics. Drafting of manuscript.
YL: Concept and study design. Data collection. Data interpretation. Data analysis and statistics.
SN: Data collection. Data interpretation. Data analysis and statistics.
SYM: Data collection. Data interpretation. Data analysis and statistics.
JYK: Study supervision. Revision and final approval of manuscript.
HT: Study supervision. Revision and final approval of manuscript.
HL: Study supervision. Concept and study design. Data interpretation. Data analysis and statistics. Drafting of manuscript. Revision and final approval of manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study adhered to the tenets of the Declaration of Helsinki. The Ethics Committee of Asan Medical Center (Seoul, Republic of Korea) approved the study protocol.
Consent to participate
Written informed consent was waived for this study given its retrospective design.
Consent for publication
Written informed consent was waived for this study given its retrospective design.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Han, J.Y., Lee, Y., Nam, S. et al. Effect of intense pulsed light using acne filter on eyelid margin telangiectasia in moderate-to-severe meibomian gland dysfunction. Lasers Med Sci 37, 2185–2192 (2022). https://doi.org/10.1007/s10103-021-03482-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-021-03482-z