Abstract
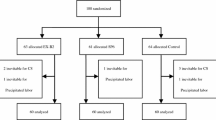
This study aimed to evaluate the effect of low-level laser therapy (LLLT) on immediate postpartum pain relief during cesarean section. A randomized, parallel controlled trial was carried out. In total, 88 women with immediate postpartum were divided into 4 groups: control group (n = 22), placebo group (n = 22), experimental group I (n = 22, dose of 4 J/cm2), and experimental group II (n = 22, dose of 2 J/cm2). The pain measured by Numeric Rating Scale (NRS), algometry, and Global Change Perception Scale (GCPS) was assessed at 12, 20–24, and 44–48 h postpartum. Two LLLT sessions were performed at 12 and 24 h postpartum. A significant interaction was observed between time versus group for NRS F (2.40) = 36.80, p < 0.001 and algometry F (1.70) = 27.18, p < 0.001. GCPS revealed a significant difference between the groups during second (p = 0.04) and third evaluation (p = 0.04). The NRS and algometry presented a large effect size for the experimental groups. LLLT is an efficient method to reduce pain and enhance the GCP in postcesarean section. No significant clinical differences were found between the laser doses.




Similar content being viewed by others
References
Hopkins K (2000) Are Brazilian women really choosing to deliver by cesarean? Soc Sci Med 51:725–740
Dalmoro C, Rosa R, Bordin R (2018) Normal delivery and cesarean section: cost per brazilian regions, 2015. Rev. Assoc Med Bras 64:1045–1049. https://doi.org/10.1590/1806-9282.64.11.1045
Carvalho B, Cohen SE, Lipman SS, Fuller A, Mathusamy AD, Macario A (2005) Patient preferences for anesthesia outcomes associated with cesarean delivery. Anesth Analg 101:1182–1187. https://doi.org/10.1213/01.ane.0000167774.36833.99
Sutton CD, Carvalho B (2017) Optimal pain management after cesarean delivery. Anesthesiol Clin 35:107–124. https://doi.org/10.1016/j.anclin.2016.09.010
Callesen T, Bech K, Kehlet H (1999) Prospective study of chronic pain after groin hernia repair. Br J Surg 86:1528–1531. https://doi.org/10.1046/j.1365-2168.1999.01320.x
Karanikolas M, Aretha D, Tsolakis I et al (2011) Optimized perioperative analgesia reduces chronic phantom limb pain intensity, prevalence, and frequency. Anesthesiology 114:1144–1154. https://doi.org/10.1097/ALN.0b013e31820fc7d2
Lahtinen P, Kokki H, Hynynen M (2006) Pain after cardiac surgery: a prospective cohort study of 1-year incidence and intensity. Anesthesiology 105:794–800
Jin J, Peng L, Chen Q et al (2016) Prevalence and risk factors for chronic pain following cesarean section: a prospective study. BMC Anesthesiol 16:99. https://doi.org/10.1186/s12871-016-0270-6
Liu TT, Raju A, Boesel T, Cyna AM, Tan SG (2013) Chronic pain after caesarean delivery: an Australian cohort. Anaesth Intensive Care 41:496–500. https://doi.org/10.1177/0310057X1304100410
Wisner K, Stika C, Clark C (2014) Double Duty: Does Epidural Labor Analgesia Reduce Both Pain and Postpartum Depression? Anesth Analg 119:219–221. https://doi.org/10.1213/ANE.0000000000000322
Eshkevari L, Trout KK, Damore J (2013) Management of postpartum pain. J Midwifery Women’s Heal 58:622–631. https://doi.org/10.1111/jmwh.12129
Volmanen P, Valanne J, Alahuhta S (2004) Breast-feeding problems after epidural analgesia for labour : a retrospective cohort study of pain, obstetrical procedures and breast-feeding practices. Int J Obstet Anesth 13:25–29. https://doi.org/10.1016/S0959-289X(03)00104-3
Fahey JO (2017) Best practices in management of postpartum pain. J Perinat Neonatal Nurs 31:126–136. https://doi.org/10.1097/JPN.0000000000000241
Chou R, Gordon DB, de Leon-Casasola OA et al (2016) Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain 17:131–157. https://doi.org/10.1016/j.jpain.2015.12.008
Kayman-Kose S, Arioz DT, Toktas H et al (2014) Transcutaneous electrical nerve stimulation (TENS) for pain control after vaginal delivery and cesarean section. J Matern Fetal Neonatal Med 27:1572–1575. https://doi.org/10.3109/14767058.2013.870549
Alvarenga MB, de Oliveira SM, Francisco AA, da Silva FM, Sousa M, Nobre MR (2017) Effect of low-level laser therapy on pain and perineal healing after episiotomy : a triple-blind randomized controlled trial. Lasers Surg Med 49:181–188. https://doi.org/10.1002/lsm.22559
Mokmeli S, Khazemikho N, Niromanesh S, Vatankhah Z (2009) The application of low-level laser therapy after cesarean section does not compromise blood prolactin levels and lactation status. Photomed Laser Surg 27:509–512. https://doi.org/10.1089/pho.2008.2314
Clijsen R, Brunner A, Barbero M, Clarys P, Taeymans J (2017) Effects of low-level laser therapy on pain in patients with musculoskeletal disorders : a systematic review and meta-analysis. Eur J Phys Rehabil Med 53:603–610. https://doi.org/10.23736/S1973-9087.17.04432-X
Avci P, Gupta A, Sadasivam M et al (2013) Low-level laser (light) therapy (LLLT) in skin: stimulating, healing, restoring. Semin Cutan Med Surg 32:41–52
Hagiwara S, Iwasaka H, Hasegawa A, Noguchi T (2008) Pre-Irradiation of blood by gallium aluminum arsenide (830 nm) low-level laser enhances peripheral endogenous opioid analgesia in rats. Anesth Analg 107:1058–1063. https://doi.org/10.1213/ane.0b013e31817ee43e
Podogrodzki J, Lebiedowski M, Szalecki M, Kepa I, Syczewska M, Jozwiak S (2016) Impact of low level laser therapy on skin blood flow. Dev Period Med 20:40–46
Ferraresi C, de Sousa MV, Huang YY, Bagnato VS, Parizotto NA, Hamblin MR (2015) Time response of increases in ATP and muscle resistance to fatigue after low-level laser (light) therapy (LLLT) in mice. Lasers Med Sci 30:1259–1267. https://doi.org/10.1007/s10103-015-1723-8
Bjordal J, Lopes-Martins R, Iversen V (2006) A randomised, placebo controlled trial of low level laser therapy for activated Achilles tendinitis with microdialysis measurement of peritendinous prostaglandin E2 concentrations. Br J Sports Med 40:76–80. https://doi.org/10.1136/bjsm.2005.020842
Wang X, Tian F, Soni SS, Gonzalez-Lima F, Liu H (2016) Interplay between up-regulation of cytochrome-c-oxidase and hemoglobin oxygenation induced by near-infrared laser. Sci Rep 6:30540. https://doi.org/10.1038/srep30540
Kuffler DP (2016) Photobiomodulation in promoting wound healing: a review. Regen Med 11:107–122. https://doi.org/10.2217/rme.15.82
Liu H, Colavitti R, Rovira II, Finkel T (2005) Redox-dependent transcriptional regulation. Circ Res 97:967–974. https://doi.org/10.1161/01.RES.0000188210.72062.10
Peplow PV, Chung TY, Ryan B, Baxter GD (2011) Laser photobiomodulation of gene expression and release of growth factors and cytokines from cells in culture: a review of human and animal studies. Photomed Laser Surg 29:285–304. https://doi.org/10.1089/pho.2010.2846
Boutron I, Altman DG, Moher D et al (2017) CONSORT Statement for Randomized Trials of Nonpharmacologic Treatments: A 2017 Update and a CONSORT Extension for Nonpharmacologic Trial Abstracts. Ann Intern Med 167:40–47. https://doi.org/10.7326/M17-0046
Poursalehan S, Nesioonpour S, Akhondzadeh R, Mokmeli S (2018) The Effect of Low-Level Laser on Postoperative Pain After Elective Cesarean Section. Anesthesiol Pain Med 8:e84195. https://doi.org/10.5812/aapm.84195
Hawker GA, Mian S, Kendzerska T, French M (2011) Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res 63:240–252. https://doi.org/10.1002/acr.20543
Cheatham SW, Kolber MJ, Mokha GM, Hanney WJ (2018) Concurrent validation of a pressure pain threshold scale for individuals with myofascial pain syndrome and fibromyalgia. J Man Manip Ther 26:25–35. https://doi.org/10.1080/10669817.2017.1349592
Kamper SJ, Maher CG, Mackay G (2009) Global rating of change scales: a review of strengths and weaknesses and considerations for design. J Man Manip Ther 17:163–170. https://doi.org/10.1179/jmt.2009.17.3.163
Miot HA (2011) Sample size in clinical and experimental. J Vasc Bras 10:275–278. https://doi.org/10.1590/S1677-54492011000400001
Mussttaf RA, Jenkins DFL, Jha AN (2019) Assessing the impact of low level laser therapy (LLLT) on biological systems: a review. Int J Radiat Biol 95:120–143. https://doi.org/10.1080/09553002.2019.1524944
Nesioonpour S, Mokmeli S, Vojdani S et al (2014) The effect of low-level laser on postoperative pain after tibial fracture surgery: a double-blind controlled randomized clinical trial. Anesthesiol Pain Med 4:e84195. https://doi.org/10.5812/aapm.17350
Ren C, McGrath C, Jin L, Zhang C, Yang Y (2017) The effectiveness of low-level laser therapy as an adjunct to non-surgical periodontal treatment: a meta-analysis. J Periodontal Res 52:8–20. https://doi.org/10.1111/jre.12361
Santos de O J, Oliveira SM, Nobre MR, Aranha AC, Alvarenga MB (2012) A randomised clinical trial of the effect of low-level laser therapy for perineal pain and healing after episiotomy: a pilot study. Midwifery 28:e653–e659. https://doi.org/10.1016/j.midw.2011.07.009
Kymplová J, Navrátil L, Knízek J (2003) Contribution of phototherapy to the treatment of episiotomies. J Clin Laser Med Surg 21:35–39. https://doi.org/10.1089/10445470360516725
Wang X, Reddy DD, Nalawade SS, Pal S, Gonzalez-Lima F, Liu H (2018) Impact of heat on metabolic and hemodynamic changes in transcranial infrared laser stimulation measured by broadband near-infrared spectroscopy. Neurophotonics 5:011004. https://doi.org/10.1117/1.NPh.5.1.011004
Funding
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior–Brasil (CAPES)–Finance Code 001.
Author information
Authors and Affiliations
Contributions
AMPHA: conceptualization, planning, data collection, and writing of the manuscript. KRRS: data collection and planning. EMSF: writing of the manuscript, supporting data analysis, and proofreading. RP: conceptualization, planning, data analysis, and writing of the manuscript. MTABCM: conceptualization, planning, data analysis, and writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (include name of committee + reference number) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the local institutional ethics committee from Federal University of Rio Grande do Norte (number: 1.998.386). The study was registered in the REBEC platform (Identifier: RBR-6B8HCC).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Holanda Araujo, A.M.P., de Sena, K.R.R., da Silva Filho, E.M. et al. Low-level laser therapy improves pain in postcesarean section: a randomized clinical trial. Lasers Med Sci 35, 1095–1102 (2020). https://doi.org/10.1007/s10103-019-02893-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-019-02893-3