Abstract
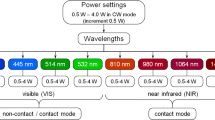
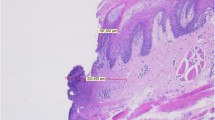
Using a 445-nm semiconductor laser for tissue incision, an effective cut is expected due to the special absorption properties of blue laser light in soft tissues. The aim of the present study was the histological evaluation of tissue samples after incision with a 445-nm diode laser. Forty soft tissue specimens were obtained from pork oral mucosa and mounted on a motorized linear translation stage. The handpiece of a high-frequency surgery device, a 970-nm semiconductor laser, and a 445-nm semiconductor laser were connected to the slide, allowing a constant linear movement (2 mm/s) and the same distance of the working tip to the soft tissue’s surface. Four incisions were made each: (I) 970-nm laser with conditioned fiber tip, contact mode at 3-W cw; (II–III): 445-nm laser with non-conditioned fiber tip, contact mode at 2-W cw, and non-contact mode (1 mm) at 2 W; and (IV): high-frequency surgery device with straight working tip, 90° angulation, contact mode at 50 W. Histological analysis was performed after H&E staining of the embedded specimens at 35-fold magnification. The comparison of the incision depths showed a significant difference depending on the laser wavelength and the selected laser parameters. The highest incision depth was achieved with the 445-nm laser contact mode (median depth 0.61 mm, min 0.26, max 1.17, interquartile range 0.58) (p < 0.05) with the lowest amount of soft tissue denaturation (p < 0.05). The lowest incision depth was measured for the high-frequency surgical device (median depth 0.36 mm, min 0.12, max 1.12, interquartile range 0.23) (p < 0.05). Using a 445-nm semiconductor laser, a higher cutting efficiency can be expected when compared with a 970-nm diode laser and high-frequency surgery. Even the 445-nm laser application in non-contact mode shows clinically acceptable incision depths without signs of extensive soft tissue denaturation.




Similar content being viewed by others
References
Hasar ZB, Ozmeric N, Ozdemir B, Gökmenoğlu C, Baris E, Altan G, Kahraman S (2016) Comparison of radiofrequency and electrocautery with conventional scalpel incisions. J Oral Maxillofac Surg 74:2136–2141
Romeo U, Libotte F, Palaia G, Del Vecchio A, Tenore G, Visca P, Nammour S, Polimeni A (2012) Histological in vitro evaluation of the effects of Er:YAG laser on oral soft tissues. Lasers Med Sci 27:749–753
Vescovi P, Corcione L, Meleti M, Merigo E, Fornaini C, Manfredi M, Bonanini M, Govoni P, Rocca JP, Nammour S (2010) Nd:YAG laser versus traditional scalpel. A preliminary histological analysis of specimens from the human oral mucosa. Lasers Med Sci 25:685–691
Niemz MH (1996) Laser-tissue interactions—fundamentals and applications, 3rd edn. Springer, Berlin
Pick RM, Colvard MD (1993) Current status of lasers in soft tissue dental surgery. J Periodontol 64:589–602
Amaral MB, de Ávila JM, Abreu MH, Mesquita RA (2015) Diode laser surgery versus scalpel surgery in the treatment of fibrous hyperplasia: a randomized clinical trial. Int J Oral Maxillofac Surg 44:1383–1389
Derikvand N, Chinipardaz Z, Ghasemi S, Chiniforush N (2016) The versatility of 980 nm diode laser in dentistry: a case series. J Lasers Med Sci 7:205–208
Romanos GE, Gutknecht N, Dieter S, Schwarz F, Crespi R, Sculean A (2009) Laser wavelengths and oral implantology. Lasers Med Sci 24:961–970
Braun A, Berthold M, Frankenberger R (2015) The 445-nm semiconductor laser in dentistry—introduction of a new wavelength. Quintessenz 66:205–211
Fornaini C, Rocca JP, Merigo E (2016) 450 nm diode laser: a new help in oral surgery. World J Clin Cases 4:253–257
Wilson SW (2014) Medical and aesthetic lasers: semiconductor diode laser advances enable medical applications. BioOptics World 7:21–25
Beard P (2011) Biomedical photoacoustic imaging. Interface Focus 1:602–631
Naqvi KR (2014) Screening hypochromism (sieve effect) in red blood cells a quantitative analysis. BiomedOpt Express 5:1290–1295
Reichelt J, Winter J, Meister J, Frentzen M, Kraus D (2017) A novel blue light laser system for surgical applications in dentistry: evaluation of specific laser-tissue interactions in monolayer cultures. Clin Oral Investig 21:985–994
Azevedo A-S, Monteiro L-S, Ferreira F, Delgado M-L, Garcês F, Carreira S, Martins M, Suarez-Quintanilla J (2016) In vitro histological evaluation of the surgical margins made by different laser wavelengths in tongue tissues. J Clin Exp Dent 8:e388–e396
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Lawrence Erlbaum Associates, Hillsdale, New Jersey
Fornaini C, Merigo E, Rocca JP, Lagori G, Raybaud H, Selleri S, Cucinotta A (2016) 450 nm blue laser and oral surgery: preliminary ex vivo study. J Contemp Dent Pract 17:795–800
Guney M, Tunc B, Gulsoy M (2014) Investigating the ablation efficiency of a 1940-nm thulium fibre laser for intraoral surgery. Int J Oral Maxillofac Surg 43:1015–1021
Fornaini C, Merigo E, Vescovi P, Bonanini M, Antonietti W, Leoci L, Lagori G, Meleti M (2015) Different laser wavelengths comparison in the second-stage implant surgery: an ex vivo study. Lasers Med Sci 30:1631–1639
Boonstra H, Oosterhuis JW, Oosterhuis AM, Fleuren GJ (1983) Cervical tissue shrinkage by formaldehyde fixation, paraffin wax embedding, section cutting and mounting. Virchows Arch A Pathol Anat Histopathol 402:195–201
Mistry RC, Qureshi SS, Kumaran C (2005) Post-resection mucosal margin shrinkage in oral cancer: quantification and significance. J Surg Oncol 91:131–133
Blasco-Morente G1, Garrido-Colmenero C, Pérez-López I, Carretero-García S, Martín-Castro A, Arias-Santiago S, Tercedor-Sánchez J (2015) Study of shrinkage of cutaneous surgical specimens. J Cutan Pathol 42:253–257
Tuncer I, Ozçakir-Tomruk C, Sencift K, Cöloğlu S (2010) Comparison of conventional surgery and CO2 laser on intraoral soft tissue pathologies and evaluation of the collateral thermal damage. Photomed Laser Surg 28:75–79
Angiero F, Parma L, Crippa R, Benedicenti S (2012) Diode laser (808 nm) applied to oral soft tissue lesions: a retrospective study to assess histopathological diagnosis and evaluate physical damage. Lasers Med Sci 27:383–388
Merigo E, Clini F, Fornaini C, Oppici A, Paties C, Zangrandi A, Fontana M, Rocca JP, Meleti M, Manfredi M, Cella L, Vescovi P (2013) Laser-assisted surgery with different wavelengths: a preliminary ex vivo study on thermal increase and histological evaluation. Lasers Med Sci 28:497–504
Acknowledgements
We acknowledge Dentsply Sirona for providing the semiconductor laser device and Robert Mandic and the staff of the Interdisciplinary Head & Neck Oncology Lab of the Departments of Otorhinolaryngology, Head & Neck Surgery, and Oral & Maxillofacial Surgery of the University of Marburg/University Hospital Giessen and Marburg (Campus Marburg) for preparing the histological samples.
Funding information
This study has been self-funded by the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Braun, A., Kettner, M., Berthold, M. et al. Efficiency of soft tissue incision with a novel 445-nm semiconductor laser. Lasers Med Sci 33, 27–33 (2018). https://doi.org/10.1007/s10103-017-2320-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-017-2320-9