Abstract
Background
We assessed the clinical effectiveness of cefiderocol (CFDC) in comparison with colistin (COL) for the treatment of carbapenem-resistant Acinetobacter baumannii (CRAB) bloodstream infections (BSI).
Materials/methods
Retrospective cohort study including adults with CRAB-BSI. Outcomes were mortality, clinical cure and adverse events during therapy. The average treatment effect of CFDC compared to COL was weighted with the inverse-probability treatment weight (IPTW).
Results
Overall, 104 patients were included (50 CFDC, 54 COL), median age 66.5 years, median Charlson Comorbidity Index 5, septic shock in 33.6% of patients. Primary BSI accounted for 43.3% of cases, followed by ventilator-associated pneumonia (VAP) (26%), catheter-related BSI (20.2%) and hospital-acquired pneumonia (HAP) (9.6%). Although not significantly, mortality at all time points was lower for CFDC than COL, while clinical cure was higher in CFDC than COL (66% vs. 44.4%, p = 0.027). Adverse events were more frequent in COL than CFDC-group (38.8% vs. 10%, p < 0.0001), primarily attributed to acute kidney injury (AKI) in the COL group. Patients with bacteremic HAP/VAP treated with CFDC had a significant lower 30-d mortality and higher clinical cure than COL (p = 0.008 and p = 0.0008, respectively). Increment of CCI (p = 0.005), ICU (p = 0.025), SARS-CoV2 (p = 0.006) and ECMO (p < 0.0001) were independently associated with 30-d mortality, while receiving CFDC was not associated with survival.
Conclusions
CFDC could represent an effective and safe treatment option for CRAB BSI, especially in patients with bacteremic HAP/VAP and frail patients where the risk of acute renal failure during therapy should be avoided.
Key summary points
Increasing real-life data support the clinical effectiveness and safety of cefiderocol (CFDC) for carbapenem resistant Acinetobacter baumannii (CRAB) infections.
We investigated CFDC in comparison with colistin (COL) for the treatment of CRAB bloodstream infections (BSI).
Clinical cure was higher in CFDC than COL group.
Patients with hospital acquired/ventilator-associated pneumonia treated with CFDC had a statistically significant lower 30-d mortality and higher clinical cure than those treated with COL.
Adverse events were more frequent in COL than in CFDC-group.
CFDC could be an effective and safe treatment option for CRAB BSI, especially in patients with HAP/VAP and frail patients where the risk of acute renal failure during therapy should be avoided.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antibiotic resistance is a major global health concern impacting both medical costs and mortality rates [1]. In particular, resistance to carbapenems in Acinetobacter baumannii exceeds 70% in Southern and Eastern European regions, including Italy [2,3,4].
Carbapenem-resistant A. baumannii (CRAB) poses a significant threat, particularly in Intensive Care Unit (ICU) settings [5]. Mortality rates are high, ranging from 50 to 70%, especially in cases of septic shock and ventilator-associated pneumonia (VAP) [4].
While colistin is considered a mainstay in CRAB treatment, mostly in combination with other antibiotics [6], its use is limited by poor lung penetration [7] and risk of nephrotoxicity [7,8,9,10]. Furthermore, many strains of CRAB have recently developed resistance against colistin and other polymyxins [4, 11].
In this context, cefiderocol (CFDC), a new siderophore cephalosporin approved by the Food and Drug Administration for the treatment of serious infections caused by carbapenem-resistant Gram-negative bacteria (CR-GNB) [12], might offer a compatible alternative in the treatment of CRAB infections.
While the phase 3 trial CREDIBLE-CR revealed that, within the subset of CRAB infections, patients treated with CFDC experienced higher mortality rates compared to those receiving the best available therapy [13], subsequent real-life studies have shown promising outcomes regarding improved clinical efficacy and safety with CFDC, particularly in the context of bloodstream infections (BSI) and ventilator-associated pneumonia (VAP) [14,15,16,17,18,19,20,21,22]. Consequently, the debate concerning the role of CFDC in treating CRAB infections remains ongoing and necessitates additional evidence from real-world settings.
The aim of the study was to evaluate the clinical effectiveness and safety of CFDC in comparison with colistin (COL) for the treatment of CRAB BSI during the COVID-19 era.
Materials and methods
Study design
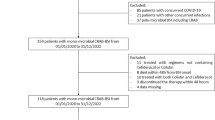
This is an observational, retrospective, single-centre study including adult patients diagnosed with CRAB BSI and hospitalized at a large Academic Hospital between June 2021 and April 2023.
Patients were categorized into those treated with CFDC- or COL-based regimens.
Inclusion criteria were (i) age > 18 years, (ii) hospitalization for at least 48 h and (iii) receipt of CFDC or COL as the definite treatment for CRAB BSI. Patients aged < 18 years, those receiving agents other than CFDC or COL or those deceased before the blood culture (BC) results had been available were excluded.
Variables
Collected data included age, gender, ward of index BC (Intensive Care Unit, ICU, or non-ICU), date of admission, previous antibiotic therapy, previous CRAB colonization, days of hospitalisation prior to infection, presence of indwelling central venous catheters, comorbidities such diabetes mellitus, cardiovascular, renal failure or haemodialysis, solid and haematological malignancies, cirrhosis, hepatopathy, obesity (defined as BMI≥30), immunosuppression, chronic obstructive pulmonary disease (COPD), HIV infection. Concomitant SARS-CoV2 infection was also recorded. Burden of comorbidities was assessed by means of Charlson Comorbidity Index (CCI) [23] while for severity at ICU admission we calculated the Simplified Acute Physiology Score (SAPS). Variables related to the infection included source of BSI, presence of septic shock at infection onset, mechanical ventilation and/or need of continuous renal replacement therapies (CRRT), extra-corporeal membrane oxygenation (ECMO), laboratory parameters such as C-reactive protein (CRP) and procalcitonin (PCT). Empiric and definitive antibiotic regimens, as well as their use in monotherapy or in combination, were also collected.
Antimicrobial treatment decision and appropriateness of therapy
The choice of antibiotic therapy was at discretion of the treating Infectious Diseases consultants. Intravenous antibiotics were administered as follows: CFDC 2 gr loading dose followed by a 3 h infusion of 2 g every 8 h; COL 9 MUI loading dose followed by 4.5 MUI every 12 h; ampicillin/sulbactam (A/S) with a total daily dose of 24–27 g (4 g/2 g every 6 h or 6 g/3 g every 8 h); fosfomycin (FOF) with a total daily dose of 16–18 g, divided every 6–8 h; tigecycline, first dose of 100–200 mg, followed by 50–100 mg every 12 h; meropenem 2 g loading dose followed by 2 g every 8 h. Dose adjustments for all antibiotics were made based on renal function, following the manufacturer’s recommendations.
Early (< 24 h) appropriate antibiotic therapy was reached when at least one drug started within 24 h from the collection of index BC was subsequently found to be active in vitro.
Definitive appropriate therapy was defined if the isolated CRAB was found to be susceptible at least to one antibiotic of the final treatment and if it was started within 48 h from BSI onset.
Study outcomes
Primary outcomes were all-cause mortality at 7, 14 and 30-d following BSI onset, while secondary outcomes were clinical and microbiological cure, occurrence of adverse events during treatment, CRAB infection recurrence and 30-d superinfections.
Definitions
Immunosuppression was defined as use of prednisolone (or equivalent) > 0.5 mg/kg/day for > 1 month, chemotherapy or immunotherapy in the last 3 months.
Infections were defined according to the CDC/NHSN criteria [24]. Hospital acquired/ventilator-associated pneumonia (HAP/VAP) were defined in accordance with CDC/NHSN surveillance definition of healthcare-associated infection for pneumonia with specific criteria [25]. VAP was defined as pneumonia in patients who had a device to assist or control respiration continuously through a tracheostomy or by endotracheal intubation within the 48 h period before the onset of infection. Primary BSI was defined as BSI occurring in patients without a recognized source of infection. Catheter-related BSI (CR-BSI) was defined if the semiquantitative culture of the catheter tip was positive for the same CRAB isolated from the blood [26]. The likely or ascertained source of BSI was indicated by the attending physician or by the Infectious Disease consultants (AO, GC) in the medical record according to guidelines [27]. In case of doubt, a panel discussion was performed.
The indicative parameters of early (48–72 h) clinical improvement were at least one of the following: discontinuation of treatment with inotropic drugs if the patient was previously in septic shock, disappearance of fever for at least 48 consecutive hours after the start of treatment, reduction of serum procalcitonin values by at least 80% compared to the initial value or achievement of a serum PCT value < 0. 5 ng/mL, a reduction of at least 75% of the maximum achieved value of c-reactive protein (PCR) [28].
Clinical cure was defined as the resolution of symptoms after the end of antibiotic treatment. Microbiological cure was defined as negative follow-up BCs with eradication of CRAB from the start of definitive therapy. CRAB infection recurrence was defined as a new isolation of the same CRAB from BC or other sites within 30 days after the clinical recovery. Superinfections were recorded at 30 days following the start of definitive treatment. Acute kidney injury (AKI) was defined as an increase in serum creatinine by ≥ 0.3 mg/dl (≥ 26.5 µmol/l) within 48 h or an increase in serum creatinine to ≥ 1.5 times baseline from the start of antibiotic therapy [29, 30].
Microbiology
According to the hospital microbiology laboratory routines, bacterial pellet obtained from positive BCs was used for bacterial identification by the Matrix-Assisted Laser Desorption Ionization–Time Of Flight Mass Spectrometry (MALDI-TOF MS) system (Bruker Daltonik GmbH, Bremen, Germany). Isolated colonies from other biological samples (sputum or lower respiratory samples in cases of HAP/VAP as source of BSI, catheter’s tip in case of CR-BSI or wound/abscesses in cases of skin and soft tissue as source of BSI) were also identified by MALDI-TOF MS system.
Antimicrobial susceptibility testing was performed with the Vitek 2 automated system (bioMérieux, Marcy l’Etoile, France) and Microscan Walkaway (Beckman and Coulter, Brea, California, USA) system. For CFDC susceptibility, the disk diffusion method was used, and the diameter of inhibition was calculated and interpreted in accordance with guidelines [31]. In instances where we provided the precise value of CFDC Minimum Inhibitory Concentration (MIC), the ComASP® Cefiderocol (Liofilchem, Roseto degli Abruzzi, Italy) was utilized, following the manufacturer’s instructions.
Statistical analyses
Categorical variables were described through absolute frequencies and percentages; quantitative variables were reported through median with interquartile range or mean and SD, depending on the normal or non-normal distribution of the data. Differences between qualitative variables were analysed by means of Chi-square or Fischer tests, while differences between quantitative variables were assessed by means of t-Student or Mann-Whitney tests, as appropriate. Multivariate Cox regression model was performed to sort out the independent predictors of mortality within 30 days from BSI onset, accounting for covariables.
The average treatment effect of CFDC compared to COL was weighted using the inverse-probability treatment weight (IPTW) accounting for variables potentially influencing the treatment (SARS-CoV2 infection, CKD, tumor, septic shock) and the outcome, such as ICU, SARS-CoV2, septic shock, CRRT, ECMO, source of infection (VAP vs. other), diabetes mellitus, age and burden of comorbidities.
To assess the balance among the variables, we calculated the standardized mean difference before and after the IPTW procedure for each variable that could potentially influence the treatment.
P-value analyses were two-sided and a p-value of less than 0.05 was considered statistically significant. All statistical analyses were performed using STATA™ software, v. 17 (StataCorp) and Graphpad Prism™, charts using Microsoft Office™ and Graphpad Prism™.
The study was conducted in accordance with the principles of the Declaration of Helsinki. The protocol was approved by the local Ethics Committee. The clinical and diagnostic management of the patients was already carried out according to normal clinical practice. Informed consent was waived due to the retrospective nature of the research.
Results
Study population
During the study period, 104 patients satisfied our inclusion criteria. Among them, 50 (48.1%) patients were treated with CFDC and 54 (51.9%) with COL. The median age was 66.5 (IQR 58–78) years, 71 (68.3%) patients were male and the median CCI was 5 (IQR 2–7), with a slightly higher CCI in CFDC than COL. At the time of infection onset, 44 (42.3%) patients had a SARS-CoV2 infection, more commonly observed in the COL group (53.7% vs. 30%, p = 0.015) and 66 (63.6%) were hospitalized in the ICU (64.8% vs. 62% in the CFDC and COL group respectively, p = 0.766). Mechanical ventilation was present in 51 (49.5%) patients and 5 (4.8%) patients needed ECMO at the time of infection. Septic shock was present in 33.6% of subjects, higher in the COL group (42.6% vs. 24%). The most frequent source of BSI was primary BSI (45, 43.3%), followed by VAP (27, 26%), CR-BSI (21, 20.2%) and HAP (10, 9.6%), with no significant differences observed between the groups.
Overall, polymicrobial BSIs were identified in 23 out of 104 patients (22.1%), distributed as follows: 6 cases of CRAB/E. faecalis, 5 cases of CRAB/KPC-producing K. pneumoniae, 5 cases of CRAB/vancomycin-resistant E. faecium (VRE), 2 cases of CRAB/S. aureus, 2 cases of CRAB/Candida spp, 2 cases of CRAB/E. cloacae, 1 case of CRAB/KPC-producing K. pneumoniae/Candida spp.
Specifically, among the patients with lung infections, 7 cases exhibited polymicrobial BSI, distributed as follows: 2 cases of CRAB/E. faecalis, 2 cases of CRAB/VRE, 1 case of CRAB/Candida spp, 1 case of CRAB/KPC, 1 case of CRAB/E. cloacae. Notably, in only the latter two cases, KPC and E. cloacae were also detected in bronchoalveolar lavage (BAL) samples, suggesting a genuine polymicrobial lung infection.
The full baseline demographic and clinical features of study population are shown in Table 1.
Combination therapy was administrated in the majority of patients (78, 75%), of which 36 (72%) treated with CFDC regimens and 42 (77.7%) with COL regimens. The most common associated antibiotic was A/S [median dosage 24 gr/die (range 6–27)], used overall in 42 (40.4%) patients [24 (48%) vs. 18 (33.3%) in CFDC and COL groups, respectively], followed by FOF in 32 (30.8%) patients [median dosage 16 gr/die (range 6–18)] [12 (24%) vs. 20 (37%) in CFDC group and COL group, respectively]. Meropenem was mainly combined with COL than CFDC (12.9% vs. 2%, p = 0.036). All the regimens are described in Supplementary Fig. 1.
Outcomes
While the 7-day, 14-day, and 30-day mortality rates did not show significant differences between the two groups, they were lower for the CFDC group compared to the COL group (16% vs. 20.4%, 22% vs. 31.5% and 36% vs. 42.6% for CFDC and COL, respectively). Notably, clinical cure was significantly higher in CFDC than in COL group (66% vs. 44.4%, p = 0.027) (Fig. 1). Details of the comparison between patients with and without clinical cure are shown in Supplementary Table 1.
After stratification according to the source of infection, we found that patients with HAP/VAP treated with CFDC had a statistically significant lower 30-d mortality and higher clinical cure than those treated with COL (22.2% vs. 68.4%, p = 0.008, and 72.2% vs. 15.8%, p = 0.0008, respectively), especially in patients with bacteremic VAP (28.6% vs. 76.9%, p = 0.02 and 71.4% vs. 7.7% p = 0.001, respectively) (Fig. 2, panel A-B).
Patients treated with COL exhibited a higher incidence of adverse events compared to those treated with CFDC regimens (38.8% vs. 10%, p < 0.0001), primarily attributed to acute kidney injury (AKI) in the COL group (Fig. 1). In detail, patients receiving CFDC experienced mild gastrointestinal toxicity (n = 4) and increase in sodium values (n = 1), the latter probably due to concomitant A/S administration, while AKI was observed in all the patients treated with COL.
No differences between the two groups were observed as for microbiological cure and rates of infection recurrence or secondary infections (Table 1).
Predictors of 30-d mortality
Comparison between 30-d survivors and non-survivors is shown in Table 2. A significative higher mortality was found in older patients (p = 0.040), those with SARS-CoV2 infection (p = 0.002), higher CCI (p = 0.0019), septic shock (p < 0.001), CRRT (p = 0.017) and ECMO (p = 0.004), while source control (when indicated) was protective (p = 0.028), as well as early clinical improvement and clinical cure (p < 0.0001 each).
At multivariable Cox regression analysis, ICU stay (HR 2.74, 95% CI 1.13–6.65, p = 0.025), SARS-CoV2 infection (HR 2.61, 95% CI 1.31–5.19, p = 0.006), ECMO (HR 8.63, 95% CI 2.68–27.77, p < 0.0001) and CCI (each point increment, HR 1.17, 95% CI 1.05–1.32, p = 0.005) were independently associated with 30-d mortality.
Receiving CFDC was not associated with the primary outcome (HR 0.91, 95% CI 0.45–1.82, p = 0.798), and this finding was further supported by the IPTW analysis (HR 0.74, CI 0.35–1.55, p = 0.431) (Table 3). The standardized mean differences before and after the IPTW procedure for each variable potentially influencing the treatment are shown in Supplementary Table 1.
Microbiology analyses
CFDC susceptibility was available in 59 patients (56.3%), equally distributed between the groups (26/50, 52% and 33/54, 61.1% in CFDC and COL, respectively). CFDC was in-vitro susceptible in all but one subjects, with MIC values ranging from 0.094 to 1.5 µg/mL. The patient with CFDC resistance even before CFDC therapy had MIC 4 µg/mL, exhibited also COL resistance and was eventually treated with COL, MEM and A/S.
Emergence of CFDC in vivo resistance was observed in one patient (MIC 4 µg/mL). Unfortunately, we could not estimate the actual MIC before CFDC treatment since only disk diffusion was available.
COL resistance was observed in 13/104 patients (12.5%). All the strains were resistant to A/S, with MIC > 16/8 µg/mL.
Use of CFDC
CFDC was mostly used in combination (36/50, 72%), particularly with A/S (48%) and FOF (24%). CFDC adjustment for renal function was noted in 12 patients, with a slightly higher 30-day mortality observed in those receiving CFDC adjusted for renal function (7/18, 38.8% vs. 5/32, 15.6%, p = 0.08), although the difference did not reach statistical significance. In particular, the patient who experienced in vivo resistance to CFDC was obese and on hemodialysis while treated.
Discussion
In this study, we demonstrated that, although the overall mortality was only slightly lower in the CFDC-treated patients, the clinical cure rate was significantly higher in the CFDC group compared to the COL group. More importantly, within the subgroup of patients with HAP/VAP, the administration of CFDC was associated with a statistically significant decrease in 30-day mortality and an increase in clinical cure compared to COL. Furthermore, CFDC was associated with a statistically significant lower rate of adverse events than COL, particularly in terms of renal failure.
The role of CFDC as a potential first therapeutic option in CRAB infections is still under debate. Although the CREDIBLE-CR study indicated higher mortality rates in the subgroup of CRAB-infected patients treated with CFDC [13], leading to current guidelines not endorsing its use [32,33,34], real-life experiences have been accumulating evidence supporting the potential benefit of CFDC over COL-based regimens, particularly in the context of BSI and lung infections [17, 19,20,21,22, 35].
Only one retrospective observational study including severe CRAB infections, of which 47.7% were bacteremic, reported a lower 30-d mortality in those treated with COL compared to CFDC-containing regimens [18].
Consistent with these findings, a recent systematic review demonstrated that, compared to alternative therapies (mostly colistin-based), patients treated with CFDC-based regimens had a lower risk of mortality when the analysis was focused on observational studies with adjustments for confounding factors [36].
In our study, we demonstrated that patients with HAP/VAP treated with CFDC had a statistically significant advantage in terms of mortality and clinical cure than those receiving COL, and this finding was even more evident in the setting of VAP. ELF penetration of antibiotics in critically ill patients with VAP remains still a concern. As a matter of fact, COL penetration in the ELF is poor [7], while, at standard dosing, CFDC exposure in the ELF is similar to that of other cephalosporins and has been demonstrated to achieve ELF concentrations sufficient for treating Gram-negative bacteria with a MIC of 4 mg/L [37]. Nevertheless, suboptimal PK/PD CFDC targets could occur, leading to microbiological failure [38].
We confirmed the role of SARS-CoV2 infection and ECMO as independent predictors of unfavorable outcome [19, 39,40,41,42], the latter probably due to a significantly reduced serum concentrations of specific antibiotics [43]. Furthermore, we found that the burden of comorbidities was independently associated with mortality. Indeed, our study population was extremely complex and frail, with a median CCI of 5 [44, 45], which was higher than that reported in many studies in the literature [19, 20] and may potentially explain the lack of statistically significant differences observed between the two groups.
These findings underscore that the presence of multiple comorbidities may have a crucial role in worsening treatment outcomes, even if antimicrobial agents have been appropriately and timely prescribed. In this context, CFDC undoubtedly exhibited a safer profile than COL, particularly concerning renal function, suggesting a net advantage in favor of CFDC for frail patients, where the risk of acute renal failure during therapy should be avoided.
Our results may also be influenced by the fact that in only 52% of patients receiving CFDC, drug susceptibility has been available. While all but one of the tested strains were susceptible to CFDC, we could not exclude that some other CRAB isolates may have been less susceptible, or even resistant, to CFDC. Indeed, resistance to CFDC in MDR Gram-negatives has emerged even before its widespread use in clinical practice [46,47,48]. In addition, development of resistance during treatment has also been observed, suggesting the need to test all isolates before and during CFDC administration [19]. Interestingly, heteroresistance is highly prevalent in CRAB, but its clinical impact is still unclear [49].
In line with the current literature [19, 20], we showed that CFDC was predominantly employed in combination, with A/S and FOF being the most frequently administered partner drugs. Despite the in vitro resistance of all our strains to A/S, the decision to still use this drug was based on the fact that, when given in high doses, such as ours, sulbactam has the capability to saturate PBP-1 and PBP-3 and may therefore overcome the increasing rates of sulbactam resistance [5]. Unfortunately, due to the low number of patients, we were not able to state whether a specific combination was associated with a better outcome, even though recent studies suggest a possible benefit for the combination CFDC plus FOF [17, 20].
Although CRAB infections are considered peculiar of the ICU, we showed that approximately one third of patients with CRAB BSI acquired the infection outside the critical care setting. This finding has important clinical implications and should raise the awareness that also patients not in the ICU may be at risk of CRAB infections, influencing not only the appropriateness of early therapy, which is a well-known predictor of survival, but also the infection control policies within the hospital [45].
Our study undoubtedly presents several limitations. First, it is a retrospective single center study, thus not leading to a generalization of the results, and the selection of antimicrobial therapies was based on the clinical judgement of physicians. Secondly, we could not obtain CFDC susceptibility in all the patients receiving the drug, and therefore we could not exclude with certainty that some patients may have had a CRAB infection sustained by a less susceptible strain, possibly influencing our results. Thirdly, we acknowledge that the two study populations exhibited distinct features that could have possibly influenced the choice of treatment and the outcome. However, we conducted the IPTW analysis to balance the covariates and to reduce potential bias related to the heterogenicity of population and the retrospective nature of the study.
Additionally, not all the infections were monomicrobial. Nevertheless, among HAP/VAP, only two were truly polymicrobial. Hence, we believe that the better outcome observed in HAP/VAP for CFDC than COL was not influenced by the presence of pathogens other than CRAB. Lastly, but not less important, we could not assess the serum CFDC concentrations in our study cohort, which may have given possible insights on the observed worse outcome in some conditions.
Conclusion
In conclusion, our data suggest that CFDC could be an effective and safe treatment option for CRAB BSI, especially in patients with HAP/VAP as well as frail patients where the risk of acute renal failure during therapy should be avoided. In our real-life experience, CFDC was mostly used in combination therapy, either with A/S or FOF. Further investigations are needed to assess the exact role of CFDC for the treatment of CRAB infections.
Data availability
All data relevant to the study are included in the article and are available from the corresponding author upon request.
Code availability
All statistical analyses were performed using STATA™ software, v. 17 (StataCorp) and Graphpad Prism™, charts using Microsoft Office™ and Graphpad Prism™.
References
Newsroom Antibiotic resistance. World Health Organization [cited 2023 July 23]. https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance
Tacconelli E, Carrara E, Savoldi A et al (2018) Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis 18(3):318–327. https://doi.org/10.1016/S1473-3099(17)30753-3Epub 2017 Dec 21. PMID: 29276051
Ayobami O, Willrich N, Suwono B, Eckmanns T, Markwart R (2020) The epidemiology of carbapenem-non-susceptible Acinetobacter species in Europe. Antimicrob Resist Infect Control 9(1):89. https://doi.org/10.1186/s13756-020-00750-5PMID: 32560670; PMCID: PMC7304165 : analysis of EARS-Net data from 2013 to 2017
Iovleva A, Mustapha MM, Griffith MP et al (2022) Carbapenem-Resistant Acinetobacter baumannii in U.S. hospitals: diversification of circulating lineages and Antimicrobial Resistance. mBio 13(2):e0275921. https://doi.org/10.1128/mbio.02759-21Epub 2022 Mar 21. PMID: 35311529; PMCID: PMC9040734
Cavallo I, Oliva A, Pages R et al (2023) Acinetobacter baumannii in the critically ill: complex infections get complicated. Front Microbiol 14:1196774. https://doi.org/10.3389/fmicb.2023.1196774PMID: 37425994; PMCID: PMC10325864
Giacobbe DR, Saffioti C, Losito AR et al (2020) Use of colistin in adult patients: a cross-sectional study. J Glob Antimicrob Resist 20:43–49. https://doi.org/10.1016/j.jgar.2019.06.009Epub 2019 Jun 15. PMID: 31207379
Imberti R, Cusato M, Villani P et al (2010) Steady-state pharmacokinetics and BAL concentration of colistin in critically ill patients after IV colistin methanesulfonate administration. Chest 138(6):1333–1339. https://doi.org/10.1378/chest.10-0463Epub 2010 Jun 17. PMID: 20558557
Ordooei Javan A, Shokouhi S, Sahraei Z (2015) A review on colistin nephrotoxicity. Eur J Clin Pharmacol 71(7):801–810. https://doi.org/10.1007/s00228-015-1865-4Epub 2015 May 27. PMID: 26008213
Chen Z, Chen Y, Fang Y et al (2015) Meta-analysis of colistin for the treatment of Acinetobacter baumannii infection. Sci Rep 5:17091. https://doi.org/10.1038/srep17091PMID: 26597507; PMCID: PMC4657015
Kengkla K, Kongpakwattana K, Saokaew S, Apisarnthanarak A, Chaiyakunapruk N (2018) Comparative efficacy and safety of treatment options for MDR and XDR Acinetobacter baumannii infections: a systematic review and network meta-analysis. J Antimicrob Chemother. ;73(1):22–32. https://doi.org/10.1093/jac/dkx368. PMID: 29069421
Cai Y, Chai D, Wang R, Liang B, Bai N (2012) Colistin resistance of Acinetobacter baumannii: clinical reports, mechanisms and antimicrobial strategies. J Antimicrob Chemother 67(7):1607–1615. https://doi.org/10.1093/jac/dks084Epub 2012 Mar 22. PMID: 22441575
US Food and Drug Administration (2019) Highlights of prescribing information: Fetroja (Cefiderocol). [cited 2023 July 23]. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/209445s000lbl.pdf
Bassetti M, Echols R, Matsunaga Y et al (2021) Efficacy and safety of cefiderocol or best available therapy for the treatment of serious infections caused by carbapenem-resistant Gram-negative bacteria (CREDIBLE-CR): a randomised, open-label, multicentre, pathogen-focused, descriptive, phase 3 trial. Lancet Infect Dis 21(2):226–240. https://doi.org/10.1016/S1473-3099(20)30796-9Epub 2020 Oct 12. PMID: 33058795
Oliva A, Ceccarelli G, De Angelis M et al (2020) Cefiderocol for compassionate use in the treatment of complicated infections caused by extensively and pan-resistant Acinetobacter baumannii. J Glob Antimicrob Resist 23:292–296 Epub 2020 Oct 13. PMID: 33065329
Rando E, Segala FV, Vargas J et al (2021) Cefiderocol for severe carbapenem-resistant A. Baumannii Pneumonia: towards the comprehension of its place in Therapy. Antibiot (Basel) 11(1):3. https://doi.org/10.3390/antibiotics11010003PMID: 35052880; PMCID: PMC8773286
Bavaro DF, Belati A, Diella L et al (2021) Cefiderocol-based combination therapy for difficult-to-treat Gram-negative severe infections: real-life Case Series and Future perspectives. Antibiot (Basel) 10(6):652. https://doi.org/10.3390/antibiotics10060652PMID: 34072342; PMCID: PMC8227820
Dalfino L, Stufano M, Bavaro DF et al (2023) Effectiveness of First-Line therapy with Old and Novel antibiotics in Ventilator-Associated Pneumonia caused by Carbapenem-Resistant Acinetobacter baumannii: a real life, prospective, observational, single-center study. Antibiot (Basel) 12(6):1048. https://doi.org/10.3390/antibiotics12061048PMID: 37370367; PMCID: PMC10295543
Mazzitelli M, Gregori D, Sasset L et al (2023) Cefiderocol-based versus colistin-based regimens for severe carbapenem-resistant Acinetobacter baumannii infections: a propensity Score-Weighted, Retrospective Cohort Study during the first two years of the COVID-19 pandemic. Microorganisms 11(4):984. https://doi.org/10.3390/microorganisms11040984PMID: 37110408; PMCID: PMC10146662
Falcone M, Tiseo G, Nicastro M et al (2021) Cefiderocol as Rescue Therapy for Acinetobacter baumannii and Other Carbapenem-resistant Gram-negative Infections in Intensive Care Unit Patients. Clin Infect Dis. ;72(11):2021–2024. https://doi.org/10.1093/cid/ciaa1410. PMID: 32941593
Russo A, Bruni A, Gullì S et al (2023) Efficacy of cefiderocol- vs colistin-containing regimen for treatment of bacteraemic ventilator-associated pneumonia caused by carbapenem-resistant Acinetobacter baumannii in patients with COVID-19. Int J Antimicrob Agents 62(1):106825. https://doi.org/10.1016/j.ijantimicag.2023.106825Epub 2023 Apr 21. PMID: 37088438; PMCID: PMC10121149
Bavaro DF, Papagni R, Belati A, Diella L, De Luca A, Brindicci G, De Gennaro N, Di Gennaro F, Romanelli F, Stolfa S, Ronga L, Mosca A, Pomarico F, Dell’Aera M, Stufano M, Dalfino L, Grasso S, Saracino A (2023) Cefiderocol Versus Colistin for the treatment of Carbapenem-Resistant Acinetobacter baumannii Complex Bloodstream infections: a retrospective, propensity-score adjusted, Monocentric Cohort Study. Infect Dis Ther 12(8):2147–2163. https://doi.org/10.1007/s40121-023-00854-6Epub 2023 Sep 1. PMID: 37653122; PMCID: PMC10505116
Rando E, Cutuli SL, Sangiorgi F, Tanzarella ES, Giovannenze F, De Angelis G, Murri R, Antonelli M, Fantoni M, De Pascale G (2023) Cefiderocol-containing regimens for the treatment of carbapenem-resistant A. Baumannii ventilator-associated pneumonia: a propensity-weighted cohort study. JAC Antimicrob Resist 5(4):dlad085. https://doi.org/10.1093/jacamr/dlad085PMID: 37484029; PMCID: PMC10359102
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383. https://doi.org/10.1016/0021-9681(87)90171-8
CDC/NHSN Surveillance Definitions for Specific Types of Infections [retrieved October 2022]. https://www.cdc.gov/nhsn/pdfs/pscmanual/17pscnosinfdef_current.pdf
Centers for Disease Control and Prevention website. National Healthcare safety Network (NHSN) Pneumonia (Ventilator-associated [VAP] and non-ventilator-associated Pneumonia [PNEU]) Event. [retrieved January 2023]. https://www.cdc.gov/nhsn/pdfs/pscmanual/6pscvapcurrent.pdf
Cleri DJ, Corrado ML, Seligman SJ (1980) Quantitative culture of intravenous catheters and other intravascular inserts. J Infect Dis 141(6):781–786. https://doi.org/10.1093/infdis/141.6.781
Centers for Disease Control and Prevention website. National Healthcare safety Network (NHSN) Bloodstream Infection (BSI) Events. [cited 2022 January 25]. https://www.cdc.gov/nhsn/psc/bsi/index.html
Oliva A, Campogiani L, Savelloni G et al (2023) Clinical characteristics and outcome of Ceftazidime/Avibactam-Resistant Klebsiella pneumoniae carbapenemase-producing Klebsiella pneumoniae infections: a retrospective, observational, 2-Center Clinical Study. Open Forum Infect Dis 10(7):ofad327. https://doi.org/10.1093/ofid/ofad327PMID: 37476077; PMCID: PMC10354859
Mehta RL, Kellum JA, Shah SV et al (2007) Acute kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 11(2):R31. https://doi.org/10.1186/cc5713PMID: 17331245; PMCID: PMC2206446
Kellum JA, Lameire N, KDIGO AKI Guideline Work Group (2013) Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (part 1). Crit Care 17(1):204. https://doi.org/10.1186/cc11454PMID: 23394211; PMCID: PMC4057151
EUCAST European Committe on antimicrobial susceptibility testing Website. Clinical breakpoints - breakpoints and guidance January 2 (2023) Clinical breakpoints (v 13.1) - new file for printing (29 June, 2023) to make new breakpoints for anaerobic bacteria available. [cited 2023 July 21]. https://www.eucast.org/clinical_breakpoints
Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ Infectious Diseases Society of America Antimicrobial-Resistant Treatment Guidance: Gram-Negative Bacterial Infections. Infectious Diseases Society of America 2023; Version 3.0. [cited 2023 June 18]. https://www.idsociety.org/practice-guideline/amr-guidance/
Tiseo G, Brigante G, Giacobbe DR et al (2022) Diagnosis and management of infections caused by multidrug-resistant bacteria: guideline endorsed by the Italian Society of Infection and Tropical Diseases (SIMIT), the Italian Society of Anti-Infective Therapy (SITA), the Italian Group for Antimicrobial Stewardship (GISA), the Italian Association of Clinical Microbiologists (AMCLI) and the Italian Society of Microbiology (SIM). Int J Antimicrob Agents. ;60(2):106611. https://doi.org/10.1016/j.ijantimicag.2022.106611. Epub 2022 Jun 11. PMID: 35697179
Paul M, Carrara E, Retamar P et al (2022) European Society of Clinical Microbiology and Infectious diseases (ESCMID) guidelines for the treatment of infections caused by multidrug-resistant Gram-negative bacilli (endorsed by European society of intensive care medicine). Clin Microbiol Infect 28(4):521–547 Epub 2021 Dec 16. PMID: 34923128
Pascale R, Pasquini Z, Bartoletti M et al (2021) Cefiderocol treatment for carbapenem-resistant Acinetobacter baumannii infection in the ICU during the COVID-19 pandemic: a multicentre cohort study. JAC Antimicrob Resist 3(4):dlab174. https://doi.org/10.1093/jacamr/dlab174PMID: 34806011; PMCID: PMC8599913
Gatti M, Cosentino F, Giannella M, Viale P, Pea F (2023) Clinical efficacy of cefiderocol-based regimens in patients with carbapenem-resistant Acinetobacter baumannii infections: A systematic review with meta-analysis. Int J Antimicrob Agents. ;63(2):107047. doi: 10.1016/j.ijantimicag.2023.107047. Epub ahead of print. PMID: 38061418
Katsube T, Nicolau DP, Rodvold KA et al (2021) Intrapulmonary pharmacokinetic profile of cefiderocol in mechanically ventilated patients with pneumonia. J Antimicrob Chemother 76:2902–2905
Gatti M, Bartoletti M, Cojutti PG et al (2021) A descriptive case series of pharmacokinetic/pharmacodynamic target attainment and microbiological outcome in critically ill patients with documented severe extensively drug-resistant Acinetobacter baumannii bloodstream infection and/or ventilator-associated pneumonia treated with cefiderocol. J Glob Antimicrob Resist 27:294–298 Epub 2021 Oct 26. PMID: 34710630
Russo A, Gavaruzzi F, Ceccarelli G et al (2022) Multidrug-resistant Acinetobacter baumannii infections in COVID-19 patients hospitalized in intensive care unit. Infection 50:83–92
Cogliati Dezza F, Arcari G, Alessi F et al (2022) Clinical impact of COVID-19 on Multi-drug-resistant Gram-negative Bacilli Bloodstream infections in an intensive care unit setting: two pandemics compared. Antibiot (Basel) 11(7):926. https://doi.org/10.3390/antibiotics11070926PMID: 35884179; PMCID: PMC9312122
Oliva A, Volpicelli L, Di Bari S et al (2022) Effect of ceftazidime/avibactam plus fosfomycin combination on 30 day mortality in patients with bloodstream infections caused by KPC-producing Klebsiella pneumoniae: results from a multicentre retrospective study. JAC Antimicrob Resist 4(6):dlac121. https://doi.org/10.1093/jacamr/dlac121PMID: 36506890; PMCID: PMC9728520
Dhamija A, Thibault D, Fugett J et al (2022) Incremental effect of complications on mortality and hospital costs in adult ECMO patients. Perfusion. ;37(5):461–469. https://doi.org/10.1177/02676591211005697. Epub 2021 Mar 26. PMID: 33765884
Kühn D, Metz C, Seiler F et al (2020) Antibiotic therapeutic drug monitoring in intensive care patients treated with different modalities of extracorporeal membrane oxygenation (ECMO) and renal replacement therapy: a prospective, observational single-center study. Crit Care 24(1):664. https://doi.org/10.1186/s13054-020-03397-1PMID: 33239110; PMCID: PMC7689974
Jouffroy R, Parfait PA, Gilbert B et al (2022) Relationship between prehospital modified Charlson Comorbidity Index and septic shock 30-day mortality. Am J Emerg Med 60:128–133 Epub 2022 Aug 6. PMID: 35961123
Cogliati Dezza F, Covino S, Petrucci F et al (2023) Risk factors for carbapenem-resistant Acinetobacter baumannii (CRAB) bloodstream infections and related mortality in critically ill patients with CRAB colonization. JAC Antimicrob Resist 5(4):dlad096. https://doi.org/10.1093/jacamr/dlad096
Longshaw SIDERO, Manissero C, Tsuji D, Echols M, Yamano R (2020) In vitro activity of the siderophore cephalosporin, cefiderocol, against molecularly characterized, carbapenem-non-susceptible gram-negative bacteria from Europe. JAC Antimicrob Resist 2(3):dlaa060. https://doi.org/10.1093/jacamr/dlaa060PMID: 34223017; PMCID: PMC8210120
Mushtaq S, Sadouki Z, Vickers A, Livermore DM, Woodford N (2020) Vitro Activity of Cefiderocol, a Siderophore Cephalosporin, against Multidrug-Resistant Gram-negative Bacteria. Antimicrob Agents Chemother 64(12):e01582–e01520. https://doi.org/10.1128/AAC.01582-20PMID: 32958717; PMCID: PMC767404
Wang Y, Li Y, Zhao J, Guan J, Ni W, Gao Z (2022) Susceptibility of cefiderocol and other antibiotics against carbapenem-resistant, Gram-negative bacteria. Ann Transl Med 10(5):261. https://doi.org/10.21037/atm-22-889PMID: 35402576; PMCID: PMC8987888
Karakonstantis S, Rousaki M, Kritsotakis EI, Cefiderocol (2022) Systematic review of mechanisms of Resistance, Heteroresistance and in vivo emergence of resistance. Antibiot (Basel) 11(6):723. https://doi.org/10.3390/antibiotics11060723PMID: 35740130; PMCID: PMC9220290
Acknowledgements
Authors acknowledge all the nursing staff for their assistance to patients.
Part of this work has been accepted as poster presentation at the 33rd European Congress of Clinical Microbiology & Infectious Diseases (Copenaghen, 13–16 April 2023).
Funding
No fundings have been received.
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
Conceptualization: OA; Methodology: OA; Data collection: LL, CS, PF, CDF, CM, SF, CG, VA, RG, AF, PF; Formal analysis and investigation: OA, SG; Writing - original draft preparation: CA, OA; Writing - review and editing: VM, OA; Supervision: VM, MCM.
Corresponding author
Ethics declarations
Conflict of interest
OA participated to advisory boards or speaker’s bureau for MSD, Zambon and Angelini. VM participated to advisory boards or speaker’s bureau for Gilead, MSD and Mundipharma. MCM participated to advisory boards or speaker’s bureau for Gilead, ASTRA-Zeneca, GSK, and Angelini. Other authors declare no conflict of interest.
Ethics approval
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the local Institutional Review Board.
Consent to participate
Specific informed consent was waived due to the retrospective nature of the research. Patients (or their representatives) provided consent for use of data for research purposes.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.

Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oliva, A., Liguori, L., Covino, S. et al. Clinical effectiveness of cefiderocol for the treatment of bloodstream infections due to carbapenem-resistant Acinetobacter baumannii during the COVID-19 era: a single center, observational study. Eur J Clin Microbiol Infect Dis 43, 1149–1160 (2024). https://doi.org/10.1007/s10096-024-04833-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-024-04833-8