Abstract
Purpose
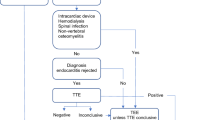
Distinguishing between complicated and uncomplicated Staphylococcus aureus bacteraemia (SAB) is therapeutically essential. However, this distinction has limitations in reflecting the heterogeneity of SAB and encouraging targeted diagnostics. Recently, a new risk stratification system for SAB metastatic infection, involving stepwise approaches to diagnosis and treatment, has been suggested. We assessed its applicability in methicillin-resistant SAB (MRSAB) patients.
Methods
We retrospectively analysed data of a 3-year multicentre, prospective cohort of hospitalised patients with MRSAB. We classified the patients into three risk groups: low, indeterminate, and high, based on the new system and compared between-group management and outcomes.
Results
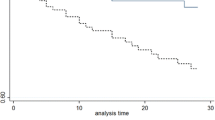
Of 380 patients with MRSAB, 6.3% were classified as low-, 7.6% as indeterminate-, and 86.1% as high-risk for metastatic infection. No metastatic infection occurred in the low-, 6.9% in the indeterminate-, and 19.6% in the high-risk groups (P < 0.001). After an in-depth diagnostic work-up, patients were finally diagnosed as ‘without metastatic infection (6.3%)’, ‘with metastatic infection (17.4%)’, and ‘uncertain for metastatic infection (76.3%)’. 30-day mortality increased as the severity of diagnosis shifted from ‘without metastatic infection’ to ‘uncertain for metastatic infection’ and ‘with metastatic infection’ (P = 0.09). In multivariable analysis, independent factors associated with metastatic complications were suspicion of endocarditis in transthoracic echocardiography, clinical signs of metastatic infection, Pitt bacteraemia score ≥ 4, and persistent bacteraemia.
Conclusions
The new risk stratification system shows promise in predicting metastatic complications and guiding work-up and management of MRSAB. However, reducing the number of cases labelled as ‘high-risk’ and ‘uncertain for metastatic infection’ remains an area for improvement.


Similar content being viewed by others
References
van Hal SJ, Jensen SO, Vaska VL, Espedido BA, Paterson DL, Gosbell IB (2012) Predictors of mortality in Staphylococcus aureus Bacteremia. Clin Microbiol Rev 25:362–386
Lam JC, Gregson DB, Robinson S, Somayaji R, Conly JM, Parkins MD (2019) Epidemiology and outcome determinants of Staphylococcus aureus bacteremia revisited: a population-based study. Infection 47:961–971
Holland TL, Arnold C, Fowler VG Jr (2014) Clinical management of Staphylococcus aureus bacteremia: a review. JAMA 312:1330–1341
Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ et al (2011) Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis 52:e18-55
Fowler VG Jr, Olsen MK, Corey GR, Woods CW, Cabell CH, Reller LB et al (2003) Clinical identifiers of complicated Staphylococcus aureus bacteremia. Arch Intern Med 163:2066–2072
Chong YP, Park SJ, Kim HS, Kim ES, Kim MN, Park KH et al (2013) Persistent Staphylococcus aureus bacteremia: a prospective analysis of risk factors, outcomes, and microbiologic and genotypic characteristics of isolates. Medicine (Baltimore) 92:98–108
Kouijzer IJE, Fowler VG Jr, Ten Oever J (2023) Redefining Staphylococcus aureus bacteremia: a structured approach guiding diagnostic and therapeutic management. J Infect 86:9–13
Chow JW, Fine MJ, Shlaes DM, Quinn JP, Hooper DC, Johnson MP et al (1991) Enterobacter bacteremia: clinical features and emergence of antibiotic resistance during therapy. Ann Intern Med 115:585–590
Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP et al (2002) Health care–associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med 137:791–797
Nambiar K, Seifert H, Rieg S, Kern WV, Scarborough M, Gordon NC et al (2018) Survival following Staphylococcus aureus bloodstream infection: a prospective multinational cohort study assessing the impact of place of care. J Infect 77:516–525
Kuehl R, Morata L, Boeing C, Subirana I, Seifert H, Rieg S et al (2020) Defining persistent Staphylococcus aureus bacteraemia: secondary analysis of a prospective cohort study. Lancet Infect Dis 20:1409–1417
Khatib R, Johnson LB, Sharma M, Fakih MG, Ganga R et al (2009) Persistence in Staphylococcus aureus bacteremia: incidence, characteristics of patients and outcome. Scand J Infect Dis 41:4–9
Lodise TP, McKinnon PS, Swiderski L, Rybak MJ (2003) Outcomes analysis of delayed antibiotic treatment for hospital-acquired Staphylococcus aureus bacteremia. Clin Infect Dis 36:1418–1423
Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T et al (2000) Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 30:633–638
Fowler VG Jr, Nelson CL, McIntyre LM, Kreiswirth BN, Monk A, Archer GL et al (2007) Potential associations between hematogenous complications and bacterial genotype in Staphylococcus aureus infection. J Infect Dis 196:738–747
Fowler VG Jr, Sanders LL, Sexton DJ, Kong L, Marr KA, Gopal AK et al (1998) Outcome of Staphylococcus aureus bacteremia according to compliance with recommendations of infectious diseases specialists: experience with 244 patients. Clin Infect Dis 27:478–486
Hagel S, Bahrs C, Schumann R, Pletz M, Weis S (2022) Complicated and uncomplicated S. aureus bacteraemia: an international Delphi survey among infectious diseases experts on definitions and treatment. Clin Microbiol Infect 28:1026.e7-.e11
Kaasch AJ, Fowler VG Jr, Rieg S, Peyerl-Hoffmann G, Birkholz H, Hellmich M et al (2011) Use of a simple criteria set for guiding echocardiography in nosocomial Staphylococcus aureus bacteremia. Clin Infect Dis 53:1–9
Buis DTP, Sieswerda E, Kouijzer IJE, Huynh WY, Burchell GL, Berrevoets MAH et al (2022) [18F]FDG-PET/CT in Staphylococcus aureus bacteremia: a systematic review. BMC Infect Dis 22:282
van Leerdam EJ, Gompelman M, Tuinte RAM, Aarntzen E, Berrevoets MAH, Maat I et al (2022) Individualizing the use of [(18)F]FDG-PET/CT in patients with complicated Staphylococcus aureus bacteremia: experiences from a tertiary care center. Infection 50:491–498
Kim T, Kim ES, Park SY, Sung H, Kim MN, Kim SH et al (2017) Phenotypic changes of methicillin-resistant Staphylococcus aureus during vancomycin therapy for persistent bacteraemia and related clinical outcome. Eur J Clin Microbiol Infect Dis 36:1473–1481
Funding
This study was supported by the Korean Society of Internal Medicine (Grant 2020–179), by a National Research Foundation of Korea (NRF) grant funded by the Korean Government (MSIT) (Grant Number: NRF-2022R1F1A1074848), and by EMBRI Grants 2022-EMBRISN0002 from the Eulji University.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, T., Lee, SR., Park, S.Y. et al. Validation of a new risk stratification system-based management for methicillin-resistant Staphylococcus aureus bacteraemia: analysis of a multicentre prospective study. Eur J Clin Microbiol Infect Dis (2024). https://doi.org/10.1007/s10096-024-04790-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10096-024-04790-2