Abstract
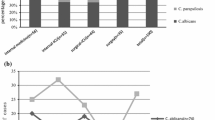
We aimed to detect possible changes in Candida species distribution over time and to know the antifungal susceptibility profile of isolates obtained from patients with bloodstream infection (BSI) due to this pathogen. Risk factors associated with 30-day mortality were also assessed. We conducted a retrospective cohort study of patients diagnosed with Candida BSI at a Japanese university hospital from 2013 to 2021. The change in the distribution pattern of the Candida spp. isolated was examined by considering three successive sub-periods of 3 years each. Risk factors for 30-day mortality were determined using Cox regression analysis. In the entire study period, Candida albicans was the most frequent species (46.7%), followed by Candida glabrata (21.5%) and Candida parapsilosis (18.7%). There was no change in Candida species distribution comparing the three sub-periods analyzed. All isolates were susceptible to micafungin, and most were susceptible to fluconazole, except for C. glabrata. No isolates were resistant to amphotericin B or voriconazole. The overall 30-day mortality was 40.2%. Univariate analysis revealed an association between 30-day mortality and central venous catheter (CVC) removal at any time, high Pitt bacteremia score (PBS), and high Charlson comorbidity index (CCI). Multivariate Cox analysis found that high PBS was the only independent predictor of 30-day mortality; subsequent multivariate Cox regression demonstrated that early CVC removal significantly reduced 30-day mortality. Candida species distribution and antifungal susceptibility profile in our hospital remained similar from 2013 to 2021. Early CVC removal may improve candidemia outcomes.


Similar content being viewed by others
Data availability
Our institution does not mandate archiving datasets generated during retrospective analyses, but they will be available on reasonable request.
References
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB (2004) Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis 39:309–317. https://doi.org/10.1086/421946
Hidron AI, Edwards JR, Patel J, Horan TC, Sievert DM, Pollock DA, Fridkin SK (2008) National Healthcare Safety Network Team; Participating National Healthcare Safety Network Facilities, NHSN annual update: antimicrobial-resistant pathogens associated with healthcare-associated infections: annual summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2006–2007. Infect Control Hosp Epidemiol 29:996–1011. https://doi.org/10.1086/591861
Puig-Asensio M, Padilla B, Garnacho-Montero J, Zaragoza O, Aguado JM, Zaragoza R, Montejo M, Muñoz P, Ruiz-Camps I, Cuenca-Estrella M, Almirante B (2014) CANDIPOP Project; GEIH-GEMICOMED (SEIMC); REIPI, Epidemiology and predictive factors for early and late mortality in Candida bloodstream infections: a population-based surveillance in Spain. Clin Microbiol Infect 20:O245-254. https://doi.org/10.1111/1469-0691.12380
Nagao M (2013) A multicentre analysis of epidemiology of the nosocomial bloodstream infections in Japanese university hospitals. Clin Microbiol Infect 19:852–858. https://doi.org/10.1111/1469-0691.12083
Magill SS, Edwards JR, Bamberg W, Beldavs ZG, Dumyati G, Kainer MA, Lynfield R, Maloney M, McAllister-Hollod L, Nadle J, Ray SM, Thompson DL, Wilson LE, Fridkin SK (2014) Emerging Infections Program Healthcare-Associated Infections and Antimicrobial Use Prevalence Survey Team, Multistate point-prevalence survey of health care-associated infections. N Engl J Med 370:1198–1208. https://doi.org/10.1056/NEJMoa1306801
Koehler P, Stecher M, Cornely OA, Koehler D, Vehreschild MJGT, Bohlius J, Wisplinghoff H, Vehreschild JJ (2019) Morbidity and mortality of candidaemia in Europe: an epidemiologic meta-analysis. Clin Microbiol Infect 25:1200–1212. https://doi.org/10.1016/j.cmi.2019.04.024
Pappas PG, Lionakis MS, Arendrup MC, Ostrosky-Zeichner L, Kullberg BJ (2018) Invasive candidiasis. Nat Rev Dis Primers 4:1–20. https://doi.org/10.1038/nrdp.2018.26
Talapko J, Juzbašić M, Matijević T, Pustijanac E, Bekić S, Kotris I, Škrlec I (2021) Candida albicans—the virulence factors and clinical manifestations of infection. J Fungi (Basel) 7:79. https://doi.org/10.3390/jof7020079
Kullberg BJ, Arendrup MC (2015) Invasive candidiasis. N Engl J Med 373:1445–1456. https://doi.org/10.1056/NEJMra1315399
Son HJ, Kim MJ, Lee S, Choi S, Jung KH, Jung J, Chong YP, Kim SH, Choi SH, Kim YS, Woo JH, Lee JY, Lee SO (2019) Risk factors and outcomes of patients with ocular involvement of candidemia. PLoS ONE 14:e0222356. https://doi.org/10.1371/journal.pone.0222356
Pfaller MA, Diekema DJ, Turnidge JD, Castanheira M, Jones RN (2019) Twenty years of the SENTRY antifungal surveillance program: results for Candida species from 1997–2016. Open Forum Infect Dis 15(Suppl 1):S79–S94. https://doi.org/10.1093/ofid/ofy358
Bassetti M, Righi E, Costa A, Fasce R, Molinari MP, Rosso R, Bobbio Pallavicini F, Viscoli C (2006) Epidemiological trends in nosocomial candidemia in intensive care. BMC Infect Dis 6:21. https://doi.org/10.1186/1471-2334-6-21
Richardson MD (2005) Changing patterns and trends in systemic fungal infections. J Antimicrob Chemother 56(Suppl 1):i5–i11. https://doi.org/10.1093/jac/dki218
Guinea J (2014) Global trends in the distribution of Candida species causing candidemia. Clin Microbiol Infect 20(Suppl 6):5–10. https://doi.org/10.1111/1469-0691.12539
Lai CC, Wang CY, Liu WL, Huang YT, Hsueh PR (2012) Time to positivity of blood cultures of different Candida species causing fungaemia. J Med Microbiol 61:701–704. https://doi.org/10.1099/jmm.0.038166-0
Clinical and Laboratory Standards Institute (2012) Reference method for broth dilution antifungal susceptibility testing of yeasts; fourth informational supplement. CLSI document M27-S4 (ISBN 1-56238-863-0 [Print]; ISBN 1-56238-864-9 [Electronic]). Wayne, PA, USA
European Committee on Antimicrobial Susceptibility Testing (2018) Antifungal agents. Breakpoint tables for interpretation of MICs, Version 9.0, valid from 2018–02–12. https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/AFST/Clinical_breakpoints/Antifungal_breakpoints_v_9.0_180212.pdf. Accessed 9 Mar 2022
Takakura S, Fujihara N, Saito T, Kudo T, Iinuma Y, Ichiyama S (2003) National surveillance of species distribution in blood isolates of Candida species in Japan and their susceptibility to six antifungal agents including voriconazole and micafungin. J Antimicrob Chemother 53:283–289. https://doi.org/10.1093/jac/dkh053
Kakeya H, Yamada K, Kaneko Y, Yanagihara K, Tateda K, Maesaki S, Takesue Y, Tomono K, Kadota JI, Kaku M, Miyazaki Y, Kamei K, Shibuya K, Niki Y, Yoshida M, Sei Y (2018) National trends in the distribution of Candida species causing candidemia in Japan from 2003 to 2014. Med Mycol J 59:E19–E22. https://doi.org/10.3314/mmj.17-00014
Boonsilp S, Homkaew A, Phumisantiphong U, Nutalai D, Wongsuk T (2021) Species distribution, antifungal susceptibility, and molecular epidemiology of Candida species causing candidemia in a tertiary care hospital in Bangkok. Thailand J Fungi (Basel) 19:577. https://doi.org/10.3390/jof7070577
Makimura K, Suzuki T, Tamura T, Ikedo M, Hanazawa R, Takahashi Y, Yamada Y, Uchida K, Yamaguchi H (2004) Comparative evaluation of standard dilution method and commercial kit for frozen plate antifungal susceptibility testing of yeasts using 200 clinical isolates. Microbiol Immunol 48:747–753
Makimura K, Oguri T, Mikami Y, Kume H, Hanazawa R, Abe M, Ikeda R, Shinoda T (2005) Multicenter evaluation of commercial frozen plates for microdilution broth antifungal susceptibility testing of yeasts and comparison of MIC limits recommended in NCCLS M27–A2. Microbiol Immunol 49:97–106
Xiao M, Chen SCA, Kong F, Xu XL, Yan L, Kong HS, Fan X, Hou X, Cheng JW, Zhou ML, Li Y, Yu SY, Huang JJ, Zhang G, Yang Y, Zhang JJ, Duan SM, Kang W, Wang H, Xu YC (2020) Distribution and antifungal susceptibility of Candida species causing candidemia in China: an update from the CHIF-NET study. J Infect Dis 16:S139–S147. https://doi.org/10.1093/infdis/jiz573
Lindberg E, Hammarström H, Ataollahy N, Kondori N (2019) Species distribution and antifungal drug susceptibilities of yeasts isolated from the blood samples of patients with candidemia. Sci Rep 7:3838. https://doi.org/10.1038/s41598-019-40280-8
Yang ZH, Song YG, Li RY (2021) A ten-year retrospective study of invasive candidiasis in a tertiary hospital in Beijing. Biomed Environ Sci 34:773–788. https://doi.org/10.3967/bes2021.107
Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner L, Reboli AC, Schuster MG, Vazquez JA, Walsh TJ, Zaoutis TE, Sobel JD (2015) Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis 62:e1-50. https://doi.org/10.1093/cid/civ933
Cornely OA, Bassetti M, Calandra T, Garbino J, Kullberg BJ, Lortholary O, Meersseman W, Akova M, Arendrup MC, Arikan-Akdagli S, Bille J, Castagnola E, Cuenca-Estrella M, Donnelly JP, Groll AH, Herbrecht R, Hope WW, Jensen HE, Lass-Flörl C, Petrikkos G, Richardson MD, Roilides E, Verweij PE, Viscoli C, Ullmann AJ (2012) ESCMID Fungal Infection Study Group, ESCMID* guideline for the diagnosis and management of Candida diseases 2012: non-neutropenic adult patients. Clin Microbiol Infect 18(Suppl 7):19–37. https://doi.org/10.1111/1469-0691.12039
Das I, Nightingale P, Patel M, Jumaa P (2011) Epidemiology, clinical characteristics, and outcome of candidemia: experience in a tertiary referral center in the UK. Int J Infect Dis 15(11):e759-763. https://doi.org/10.1016/j.ijid.2011.06.006
Nagao M, Saito T, Doi S, Hotta G, Yamamoto M, Matsumura Y, Matsushima A, Ito Y, Takakura S, Ichiyama S (2012) Clinical characteristics and risk factors of ocular candidiasis. Diagn Microbiol Infect Dis 73:149–152. https://doi.org/10.1016/j.diagmicrobio.2012.03.006
Ueda T, Takesue Y, Tokimatsu I, Miyazaki T, Nakada-Motokawa N, Nagao M, Nakajima K, Mikamo H, Yamagishi Y, Kasahara K, Yoshihara S, Ukimura A, Yoshida K, Yoshinaga N, Izumi M, Kakeya H, Yamada K, Kawamura H, Endou K, Yamanaka K, Yoshioka M, Amino K, Ikeuchi H, Uchino M, Miyazaki Y (2019) The incidence of endophthalmitis or macular involvement and the necessity of a routine ophthalmic examination in patients with candidemia. PLoS ONE 14:e0216956. https://doi.org/10.1371/journal.pone.0216956
Andes DR, Safdar N, Baddley JW, Playford G, Reboli AC, Rex JH, Sobel JD, Pappas PG, Kullberg BJ (2012) Mycoses Study Group, Impact of treatment strategy on outcomes in patients with candidemia and other forms of invasive candidiasis: a patient-level quantitative review of randomized trials. Clin Infect Dis 54:1110–1122. https://doi.org/10.1093/cid/cis021
Nucci M, Anaissie E, Betts RF, Dupont BF, Wu C, Buell DN, Kovanda L, Lortholary O (2010) Early removal of central venous catheter in patients with candidemia does not improve outcome: analysis of 842 patients from 2 randomized clinical trials. Clin Infect Dis 51:295–303. https://doi.org/10.1086/653935
Liu CY, Huang LJ, Wang WS, Chen TL, Yen CC, Yang MH, Hsiao LT, Liu CY, Chen PM, Chiou TJ (2009) Candidemia in cancer patients: impact of early removal of non-tunneled central venous catheters on outcome. J Infect 58:154–160. https://doi.org/10.1016/j.jinf.2008.12.008
Garnacho-Montero J, Díaz-Martín A, García-Cabrera E, Pérez R, de Pipaón M, Hernández-Caballero C, Lepe-Jiménez JA (2013) Impact on hospital mortality of catheter removal and adequate antifungal therapy in Candida spp. bloodstream infections. J Antimicrob Chemother 68:206–213. https://doi.org/10.1093/jac/dks347
Lee YM, Kim DY, Kim YJ, Park KH, Lee MS (2019) Clinical impacts of delayed central venous catheter removal according to the severity of comorbidities in patients with candidaemia. J Hosp Infect 103:420–427. https://doi.org/10.1016/j.jhin.2019.08.018
Nucci M, Rocha Braga P, Nouér SA, Anaissie E (2018) Time of catheter removal in candidemia and mortality. Braz J Infect Dis 22:455–461. https://doi.org/10.1016/j.bjid.2018.10.278
Kutlu M, Sayın-Kutlu S, Alp-Çavuş S, Öztürk ŞB, Taşbakan M, Özhak B, Kaya O, Kutsoylu OE, Şenol-Akar Ş, Turhan Ö, Mermut G, Ertuğrul B, Pullukcu H, Banu Çetin Ç, Avkan-Oğuz V, Yapar N, Yeşim-Metin D, Ergin Ç (2022) Mortality-associated factors of candidemia: a multi-center prospective cohort in Turkey. Eur J Clin Microbiol Infect Dis 41:597–607. https://doi.org/10.1007/s10096-021-04394-0
Janum S, Afshari A (2016) Central venous catheter (CVC) removal for patients of all ages with candidaemia. Cochrane Database Syst Rev 7:CD011195. https://doi.org/10.1002/14651858.CD011195.pub2
Clancy CJ, Nguyen MH (2013) Finding the “missing 50%” of invasive candidiasis: how nonculture diagnostics will improve understanding of disease spectrum and transform patient care. Clin Infect Dis 56:1284–1292. https://doi.org/10.1093/cid/cit006
Acknowledgements
Editorial support in the form of medical writing, assembling tables, and creating high-resolution images based on authors’ detailed directions, collating author comments, copyediting, fact checking, and referencing was provided by Editage, Cactus Communications.
Author information
Authors and Affiliations
Contributions
Conceptualization: Hitoshi Tsukamoto, Takashi Higashi, Takaaki Kodawara, Hiromichi Iwasaki, Nobuyuki Goto.
Data curation: Hitoshi Tsukamoto, Takashi Higashi.
Formal analysis: Hitoshi Tsukamoto, Takashi Higashi, Kyohei Watanabe, Nobuyuki Goto.
Investigation: Hitoshi Tsukamoto, Takashi Higashi, Takaaki Kodawara, Kyohei Watanabe, Yukio Hida.
Project administration: Hiromichi Iwasaki, Nobuyuki Goto.
Supervision: Hiromichi Iwasaki, Nobuyuki Goto.
Validation: Hitoshi Tsukamoto, Takashi Higashi, Takaaki Kodawara, Kyohei Watanabe, Yukio Hida.
Visualization: Hitoshi Tsukamoto.
Writing—original draft: Hitoshi Tsukamoto.
Writing—review and editing: Hitoshi Tsukamoto, Takashi Higashi, Takaaki Kodawara, Kyohei Watanabe, Yukio Hida, Hiromichi Iwasaki, and Nobuyuki Goto.
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the institutional review board of the Faculty of Medical Sciences, University of Fukui (approval number: 20120089). The study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. The requirement for informed consent was waived due to the retrospective nature of the study.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tsukamoto, H., Higashi, T., Kodawara, T. et al. A longitudinal study of Candida bloodstream infections in a Japanese university hospital: species distribution, drug susceptibility, clinical features, and mortality predictors. Eur J Clin Microbiol Infect Dis 41, 1315–1325 (2022). https://doi.org/10.1007/s10096-022-04499-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-022-04499-0