Abstract
The cephalosporin-β-lactamase-inhibitor-combinations, ceftolozane/tazobactam and ceftazidime/avibactam, have revolutionized treatment of carbapenem-resistant Pseudomonas aeruginosa (CR-PA). A contemporary assessment of their in vitro potency against a global CR-PA collection and an assessment of carbapenemase diversity are warranted. Isolates determined as CR-PA by the submitting site were collected from 2019–2021 (17 centers in 12 countries) during the ERACE-PA Global Surveillance Program. Broth microdilution MICs were assessed per CLSI standards for ceftolozane/tazobactam, ceftazidime/avibactam, ceftazidime, and cefepime. Phenotypic carbapenemase testing was conducted (modified carbapenem inactivation method (mCIM)). mCIM positive isolates underwent genotypic carbapenemase testing using the CarbaR, the CarbaR NxG, or whole genome sequencing. The MIC50/90 was reported as well as percent susceptible (CLSI and EUCAST interpretation). Of the 807 isolates, 265 (33%) tested carbapenemase-positive phenotypically. Of these, 228 (86%) were genotypically positive for a carbapenemase with the most common being VIM followed by GES. In the entire cohort of CR-PA, ceftolozane/tazobactam and ceftazidime/avibactam had MIC50/90 values of 2/ > 64 and 4/64 mg/L, respectively. Ceftazidime/avibactam was the most active agent with 72% susceptibility per CLSI compared with 63% for ceftolozane/tazobactam. For comparison, 46% of CR-PA were susceptible to ceftazidime and cefepime. Against carbapenemase-negative isolates, 88 and 91% of isolates were susceptible to ceftolozane/tazobactam and ceftazidime/avibactam, respectively. Ceftolozane/tazobactam and ceftazidime/avibactam remained highly active against carbapenem-resistant P. aeruginosa, particularly in the absence of carbapenemases. The contemporary ERACE-PA Global Program cohort with 33% carbapenemase positivity including diverse enzymology will be useful to assess therapeutic options in these clinically challenging organisms with limited therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multi-drug resistant Pseudomonas aeruginosa burdens clinicians across the globe due to the limited treatment options [1]. P. aeruginosa represents such a challenging pathogen due to the numerous mechanisms that drive antimicrobial resistance including drug efflux/porin loss, endogenous/exogenous β-lactamases, and target site mutations [2]. Although resistance mechanisms and epidemiology may differ based on geographic region, resistance to carbapenems is noted around the globe leaving clinicians agents that may be less effective and/or more toxic than β-lactams (i.e., polymyxins, aminoglycosides) [1]. Between 2014 and 2015, novel cephalosporin-β-lactamase-inhibitor combinations, ceftolozane/tazobactam and ceftazidime/avibactam, were introduced and revolutionized the treatment of carbapenem-resistant P. aeruginosa [3, 4].
Since introduction, both ceftolozane/tazobactam and ceftazidime/avibactam have shown potent activity against clinical P. aeruginosa isolates including carbapenem-resistant isolates [5]. The potent in vitro activity translated to improved patient outcomes compared to best available therapies by improving efficacy and safety [6,7,8]. However, now years into both agents representing important therapies for susceptible carbapenem-resistant P. aeruginosa where other β-lactams are ineffective, resistance has been described. Plasmid-mediated resistance due to carbapenemase production, including metallo-β-lactamases, has been a noted clinical challenge since introduction of both therapies due to β-lactam cross-resistance and global spread of such organisms increases concerns [9]. Similarly, mutations to chromosomally encoded P. aeruginosa derived cephalosporinases (PDCs) and transmissible extended-spectrum β-lactamases have been described also resulting in ceftolozane/tazobactam and ceftazidime/avibactam resistance [10, 11]. Indeed, a regional assessment from a global program of the in vitro activity of these agents 5 years later against the targeted pathogen of carbapenem-resistant P. aeruginosa will help clinicians assess the activity of these agents in their region.
Herein, we describe the establishment of the Enhancing Rational Antimicrobials against Carbapenem-resistant P. aeruginosa (ERACE-PA) Global Surveillance Program. This is a multi-center, multi-national surveillance program comprised of carbapenem-resistant P. aeruginosa submitted from around the globe. The program represents a contemporary assessment of the in vitro potency of ceftolozane/tazobactam and ceftazidime/avibactam 5 years into use. Additionally, the carbapenemase diversity of included isolates was assessed to categorize the cohort.
Methods
Bacterial isolates
Isolates were compiled as part of the ERACE-PA Global Surveillance Program. A total of 17 sites from 12 countries were included in the program. Global sites were located in Köln, Germany; Sao Paulo, Brazil; Istanbul, Turkey; Tel Aviv, Israel; Madrid, Spain; Jabriya, Kuwait; Cape Town, South Africa; Bogotá, Colombia; Athens, Greece; Jeddah, Saudi Arabia; Pisa, Italy; and Genoa, Italy. In the USA, centers from New York, NY; Miami, FL; St. Louis, MO; Seattle, WA; and Louisville, KY, submitted isolates. Isolates were sent to the central laboratory (Center for Anti-Infective Research and Development, Hartford, CT) for storage frozen at − 80 o C in skim milk until assessment.
Isolates could be included if they were non-duplicate isolates identified as P. aeruginosa by local standards of practice and determined to be carbapenem-resistant by the submitting site. Isolates were collected from 2019 to 2021. Isolates could be cultured from any anatomical site and there was no patient age limit for inclusion.
In vitro susceptibility testing
Isolates were transferred from frozen stock and then subsequently subcultured once more prior to all testing. Reference broth microdilution MICs were conducted at the central laboratory per CLSI standards to ceftolozane/tazobactam, ceftazidime/avibactam, ceftazidime, and cefepime [12, 13]. Routine quality control was conducted after tray preparation and during each MIC run using either ATCC P. aeruginosa ATCC 27853 or ATCC K. pneumoniae 700603. MICs were read after 16–20 h incubation and colony counts were conducted for each inoculum to confirm the target bacterial burden was transferred to the MIC trays by transferring one µL from a control well onto a trypticase soy agar with 5% sheep’s blood plate which was subsequently counted after overnight incubation.
Phenotypic carbapenemase screening
All isolates underwent phenotypic carbapenemase testing at the central laboratory using the modified carbapenem inactivation method (mCIM) per CLSI standards and interpreted by CLSI standards [12]. Routine quality control was conducted with each mCIM run with two negative controls (P. aeruginosa ATCC 27,853 and ATCC BAA K. pneumoniae 1706) and two positive controls (ATCC BAA K. pneumoniae 1705 (KPC-positive) and K. pneumoniae CDC #766 (NDM-positive).
Genotypic carbapenemase detection
Any isolates that tested mCIM positive were then assessed on the CarbaR assay (Cepheid, Sunnyvale, CA, USA) per the manufacturer’s package insert. Results were determined as positive for KPC, NDM, VIM, IMP, OXA-48-like, or negative for all targets.
All isolates that tested negative on the commercially available CarbaR were sent to Cepheid for assessment on the Research Use Only CarbaR NxG as previously described [14]. NxG testing assessed for the presence of more carbapenemase targets including GES, SPM, IMI, OXA-58, and IMP-subtypes.
Isolates negative for both assays underwent whole genome sequencing as previously described to evaluate for enzymatic resistance mechanisms outside of the CarbaR and CarbaR NxG spectrum [14].
Additional CarbaR NxG testing was conducted on ceftolozane/tazobactam-resistant isolates that tested mCIM negative to evaluate for GES-harboring isolates as this enzymology has previously been described as testing falsely negative [15, 16].
Clinical data
The present study was approved by the Hartford Hospital institutional review board and determined as exempted as all patient care was delivered per standards of care in the past, and thus, written informed consent was not obtained. De-identified clinical data of sex, age, hospital level of care at time of culture (intensive care unit (ICU), ward, or outpatient), and source of infection (respiratory, blood, urine, intra-abdominal, or other) were collected. Pediatric patients were defined as patients age < 18 years old.
Analysis
The categorical interpretation of the MIC for each agent was determined using CLSI and EUCAST interpretive criteria and described as percent susceptible, intermediate, and resistant (as applicable) in the entire cohort and subgroups [12, 17]. Demographic data was assessed using descriptive statistics including percentages for categorical data. For continuous data, the mean and standard deviation was reported.
Results
Demographics
A total of 807 isolates were collected. The mean age of patients was 56 (± 21) years-old and 62% of patients were male. A total of 46 isolates (7%) were obtained from patients less than 18 years old. The majority of patients were on inpatient wards (54%) at the time of culture, 37% were ICU patients. The respiratory tract represented the most common identified source (41%) followed by urine (20%) and blood (11%). Full demographic data are presented in Table 1.
Carbapenemase assessment
Phenotypic detection of a carbapenemase was noted for 265 of the 807 (33%) isolates. A total of 228 of the 265 (86%) phenotypically positive isolates had a carbapenemase gene detected by molecular testing (Table 2). Carbapenemase prevalence varied by region with the highest prevalence rates in Africa and Middle East with 68 and 46% of isolates from each region, respectively.
The most common carbapenemase genotypically identified was VIM (49%) followed by GES (21%). A total of 15 genotypically GES-categorized isolates tested mCIM-negative. The diversity of carbapenemase enzymology is presented in Table 2. Twelve isolates co-harbored two carbapenemase genes including nine harboring both metallo- and serine-carbapenemases.
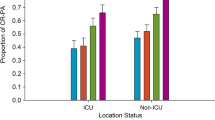
Ceftolozane/tazobactam and ceftazidime/avibactam in vitro activity
Against this global collection of carbapenem-resistant-P. aeruginosa, ceftolozane/tazobactam and ceftazidime/avibactam had MIC50/MIC90 values of 2/ > 64 mg/L and 4/64 mg/L, respectively. Ceftazidime/avibactam was the most active agent with 72% susceptibility per CLSI and EUCAST criteria followed by ceftolozane/tazobactam with 63% in all isolates. Both ceftazidime and cefepime remained susceptible against 46% of the carbapenem-resistant P. aeruginosa. Assessing isolates that tested phenotypically negative for carbapenemase production, more isolates tested susceptible to ceftolozane/tazobactam and ceftazidime/avibactam with 88 and 91% susceptibility, respectively. The phenotypic profiling of all isolates is presented in Fig. 1a, and the MIC distribution specific to phenotypically carbapenemase negative isolates is presented in Fig. 1b. Of note, a high proportion of serine-carbapenemase harboring isolates (KPC, n = 8; GES, n = 59) tested ceftazidime/avibactam susceptible with MIC50/MIC90 values of 4/8 and 2/8 mg/L, respectively. Table 3 displays the susceptibility testing results by each carbapenemase class.
a MIC distribution of tested agents in the entire cohort. Ceftolozane/tazobactam: MIC50/90 2/ > 64 mg/L, 63% susceptible; Ceftazidime/avibactam: MIC50/90 4/64 mg/L, 72% susceptible. Ceftazidime: MIC50/90 16/ > 64 mg/L, 46% susceptible; cefepime MIC50/90 16/ > 64, 46% susceptible. b. MIC distribution of tested agents in the phenotypically carbapenemase negative isolates. Ceftolozane/tazobactam: MIC50/90 1/8 mg/L, 88% susceptible; Ceftazidime/avibactam: MIC50/90 2/8 mg/L, 91% susceptible. Ceftazidime: MIC50/90 4/ > 64 mg/L, 65% susceptible; cefepime MIC50/90 8/64, 63% susceptible
The MIC results by region are presented in Table 4. Regional differences in susceptibility patterns were noted with ceftolozane/tazobactam susceptibility ranged from 32 to 85%. Similarly, ceftazidime/avibactam susceptibility ranged from 34 to 87%. For comparison, similar ranges were observed with ceftazidime and cefepime with susceptibility ranges of 22 to 56% and 14 to 60%, respectively.
Discussion
In a global collection of carbapenem-resistant P. aeruginosa, 33% of isolates tested phenotypically positive for carbapenemase production which varied based on region. Considering this high prevalence of carbapenemases, ceftolozane/tazobactam and ceftazidime/avibactam remained highly active against this collection of carbapenem-resistant P. aeruginosa five years into their use. Ceftazidime/avibactam remained highly active against the identified serine-carbapenemase producing isolates, further highlighting the importance of β-lactamase identification to guide therapy in the clinic.
Similar to previously assessed cohorts, VIM was the most commonly encountered carbapenemase in our study [18]. Notably detection of GES was the second most commonly identified in this cohort and is a growing clinical concern [19]. Detection of GES was most common in Europe; however GES harboring isolates were also identified in the Middle East and Africa. Although none of the US collected isolates in the present study tested positive for GES, recent reports have described their occurrence in the USA [20, 21]. These data call for introduction of commercially available assays that detect GES to better identify and subsequently help clinicians ascertain the most likely active antimicrobials against GES-harboring P. aeruginosa. IMP-harboring P. aeruginosa have been considered endemic to South East Asia [22]. The present study identified IMP harboring isolates from both the Middle East and South America further confirming global spread. A strength of the present study was the systematic approach where all isolates underwent phenotypic carbapenemase screening prior to genotypic assessment (CarbaR, CarbaR NxG, and WGS) considering that some carbapenemases may be outside the spectrum of current genotypic assays [14, 23]. Previous reports have shown that mCIM testing has excellent sensitivity (i.e., 98%) and would capture isolates outside of the scope of commercially available genotypic testing platforms (i.e., SPM and some IMP) [14, 15, 23]. However, false negatives are possible particularly among subtypes with poor hydrolytic activity (e.g., GES) [15, 23]. Additionally, with further implementation of carbapenemase-detection for carbapenem-resistant P. aeruginosa into clinical practice, periodic assessments on a local and global level should be conducted to detect shifts in carbapenemase prevalence and diversity to dictate local best practices for empiric therapy.
Previous data have supported the in vitro potency of ceftolozane/tazobactam and ceftazidime/avibactam against carbapenem-resistant P. aeruginosa. Indeed, susceptibility to both agents was highest in the USA consistent with a multicenter assessment that previously found 91 and 81% of isolate testing susceptible to each agent, respectively [5]. This high proportion of isolate testing susceptible to ceftolozane/tazobactam and ceftazidime/avibactam is likely secondary to the prominence of porin alterations and cephalosporinase over-production driving carbapenem-resistance. Considering the higher prevalence of carbapenemases globally, an assessment of meropenem-non-susceptible isolates from 2012 to 2014 found 72% susceptibility to ceftazidime/avibactam similar to the 72% susceptibility presented here [24]. Specific to an assessment of European and South American countries, ceftolozane/tazobactam remained active against 65% of carbapenem-non-susceptible P. aeruginosa in both regions compared with 65% and 66% of carbapenem-resistant isolates in the present study, respectively [25, 26]. The lowest ceftolozane/tazobactam and ceftazidime/avibactam susceptibility was observed in the Middle East/African sites. This is consistent with the high prevalence of metallo-β-lactamases observed in the present study and previous assessments from other countries in the region [27,28,29]. Assessments of novel agents or combinations with activity against both serine- and metallo-β-lactamase-producing P. aeruginosa are urgently needed in areas with such high prevalence of isolates harboring each or both enzyme classes.
Another underappreciated observation of the present study was that nearly 60% of carbapenem-resistant P. aeruginosa were isolated outside the ICU. While these findings are not ne [30], they have a tremendous impact on appropriate empiric therapy for the non-ICU patient population. These data further appeal for clinicians to consider early therapy that is active against carbapenem-resistant P. aeruginosa as part of empiric therapy guidelines outside of the intensive care units. The use of rapid molecular diagnostics will also help guide therapeutic decisions both within and outside the ICU.
The present study is not without limitations. Indeed, whole genome sequencing was not conducted for all carbapenemase positive isolates, so individual carbapenemase alleles were outside of the scope of the present study. However, we had a rigorous assessment for genotypic carbapenemases detection that included the commercially available CarbaR and the CarbaR NxG provides an expanding insight into the molecular detection of carbapenemases outside of only the “Big Five.” Additionally, this approach has translational benefit since healthcare providers in the clinical setting are increasingly making therapeutic decisions based on commercially available genotypic assays. Similarly, mutations in chromosomal resistance mechanisms have been described to dictate ceftolozane/tazobactam and ceftazidime/avibactam susceptibility[11] however based on the molecular methods used were not assessed here.
In conclusion, the findings of the present study re-affirm the potency of ceftolozane/tazobactam and ceftazidime/avibactam against a global collection of carbapenem-resistant P. aeruginosa 5 years into marketing. Clinicians should consider the local prevalence and diversity of carbapenemases among P. aeruginosa to guide antimicrobial therapy as their presence may dramatically change the ceftolozane/tazobactam and ceftazidime/avibactam susceptibility profile. Rapid carbapenemase-detection may help direct empiric therapy to ceftolozane/tazobactam, ceftazidime/avibactam, or alternative agents sooner in the clinical course prior to conventional susceptibility testing results. Additionally, the ERACE-PA Global Surveillance Program provides a contemporary collection of carbapenem-resistant P. aeruginosa to study therapeutic optimization for this challenging pathogen.
Data availability
Data are available through inquiry with the corresponding investigator.
Code availability
Not applicable.
References
Horcajada JP, Montero M, Oliver A, Sorlí L, Luque S, Gómez-Zorrilla S, Benito N, Grau S (2019) Epidemiology and Treatment of Multidrug-Resistant and Extensively Drug-Resistant Pseudomonas aeruginosa Infections. Clin Microbiol Rev 9(32):e00031-e119
Quale J, Bratu S, Gupta J, Landman D (2006) Interplay of efflux system, ampC, and oprD expression in carbapenem resistance of Pseudomonas aeruginosa clinical isolates. Antimicrob Agents Chemother 50:1633–1641
Zerbaxa® (2020) (ceftolozane/tazobactam) [Package Insert]. Merck Sharpe & Dohme Corp., Whitehouse Station. https://www.merck.com/product/usa/pi_circulars/z/zerbaxa/zerbaxa_pi.pdf
Avycaz® (2020) (ceftazidime/avibactam) [Package Insert]. Allergan USA, Inc., Madison. https://media.allergan.com/actavis/actavis/media/allergan-pdf-documents/product-prescribing/Avycaz_Final_PI_CBE-0_10_2019.pdf
Grupper M, Sutherland C, Nicolau DP (2017) Multicenter evaluation of ceftazidime-avibactam and ceftolozane-tazobactam inhibitory activity against meropenem-nonsusceptible pseudomonas aeruginosa from blood, respiratory tract, and wounds. Antimicrob Agents Chemother 61:e00875-e917
Pogue JM, Kaye KS, Veve MP, Patel TS, Gerlach AT, Davis SL, Puzniak LA, File TM, Olson S, Dhar S, Bonomo RA, Perez F (2020) Ceftolozane/tazobactam vs polymyxin or aminoglycoside-based regimens for the treatment of drug-resistant pseudomonas aeruginosa. Clin Infect Dis 71:304–310
Carmeli Y, Armstrong J, Laud PJ, Newell P, Stone G, Wardman A, Gasink LB (2016) Ceftazidime-avibactam or best available therapy in patients with ceftazidime-resistant Enterobacteriaceae and Pseudomonas aeruginosa complicated urinary tract infections or complicated intra-abdominal infections (REPRISE): a randomised, pathogen-directed, phase 3 study. Lancet Infect Dis 16:661–673
Vena A, Giacobbe DR, Castaldo N, Cattelan A, Mussini C, Luzzati R, Rosa FG, Del Puente F, Mastroianni CM, Cascio A, Carbonara S, Capone A, Boni S, Sepulcri C, Meschiari M, Raumer F, Oliva A, Corcione S, Bassetti M (2020) Clinical Experience with Ceftazidime-Avibactam for the Treatment of Infections due to Multidrug-Resistant Gram-Negative Bacteria Other than Carbapenem-Resistant Enterobacterales. Antibiotics (Basel) 9(9):71
van Duin D, Bonomo RA (2016) Ceftazidime/Avibactam and Ceftolozane/Tazobactam: Second-generation β-Lactam/β-Lactamase Inhibitor Combinations. Clin Infect Dis 63:234–241
Ortiz de la Rosa JM, Nordmann P, Poirel L (2019) ESBLs and resistance to ceftazidime/avibactam and ceftolozane/tazobactam combinations in Escherichia coli and Pseudomonas aeruginosa. J Antimicrob Chemother 74:1934–1939
Teo JQ, Lim JC, Tang CY, Lee SJ, Tan SH, Sim JH, Ong RT, Kwa AL (2021) Ceftolozane/Tazobactam Resistance and Mechanisms in Carbapenem-Nonsusceptible Pseudomonas aeruginosa. mSphere 6:e01026-20
CLSI (2021) Performance standards for antimicrobial susceptibility testing, 31st edn. CLSI Supplement M100. Clinical and Laboratory Standards Institute, Wayne
CLSI (2018) Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically, 11th edn. CLSI Supplement M7. Clinical and Laboratory Standards Institute, Wayne
Gill CM, Asempa TE, Tickler IA, Dela Cruz C, Tenover FC, Nicolau DP (2020) Evaluation of the Xpert Carba-R NxG Assay for Detection of Carbapenemase Genes in a Global Challenge Set of Pseudomonas aeruginosa Isolates. J Clin Microbiol 58:e01098-e1120
Gill CM, Lasko MJ, Asempa TE, Nicolau DP (2020) Evaluation of the EDTA-Modified Carbapenem Inactivation Method for Detecting Metallo-β-Lactamase-Producing Pseudomonas aeruginosa. J Clin Microbiol 58:e02015-e2019
Lisboa LF, Turnbull L, Boyd DA, Mulvey MR, Dingle TC (2017) Evaluation of a Modified Carbapenem Inactivation Method for Detection of Carbapenemases in Pseudomonas aeruginosa. J Clin Microbiol 56:e01234-e1317
The European Committee on Antimicrobial Susceptibility Testing (2021) Breakpoint tables for interpretation of MICs and zone diameters. Version 11.0. http://www.eucast.org
Kazmierczak KM, Rabine S, Hackel M, McLaughlin RE, Biedenbach DJ, Bouchillon SK, Sahm DF, Bradford PA (2015) Multiyear, Multinational Survey of the Incidence and Global Distribution of Metallo-β-Lactamase-Producing Enterobacteriaceae and Pseudomonas aeruginosa. Antimicrob Agents Chemother 60:1067–1078
Potron A, Poirel L, Nordmann P (2015) Emerging broad-spectrum resistance in Pseudomonas aeruginosa and Acinetobacter baumannii: Mechanisms and epidemiology. Int J Antimicrob Agents 45:568–585
Khan A, Tran TT, Rios R, Hanson B, Shropshire WC, Sun Z, Diaz L, Dinh AQ, Wanger A, Ostrosky-Zeichner L, Palzkill T, Arias CA, Miller WR (2019) Extensively Drug-Resistant Pseudomonas aeruginosa ST309 Harboring Tandem Guiana Extended Spectrum β-Lactamase Enzymes: A Newly Emerging Threat in the United States. Open Forum Infect Dis 6:ofz273
Gill CM, Asempa TE, Nicolau DP (2020) Development and Application of a Pragmatic Algorithm to Guide Definitive Carbapenemase Testing to Identify Carbapenemase-Producing Pseudomonas aeruginosa. Antibiotics (Basel) 9:738
Bush K, Bradford PA (2020) Epidemiology of β-Lactamase-Producing Pathogens. Clin Microbiol Rev 33:e00047-e119
Tamma PD, Simner PJ (2018) Phenotypic Detection of Carbapenemase-Producing Organisms from Clinical Isolates. J Clin Microbiol 56:e01140-e1218
Nichols WW, de Jonge BL, Kazmierczak KM, Karlowsky JA, Sahm DF (2016) In Vitro Susceptibility of Global Surveillance Isolates of Pseudomonas aeruginosa to Ceftazidime-Avibactam (INFORM 2012 to 2014). Antimicrob Agents Chemother 60:4743–4749
Pfaller MA, Bassetti M, Duncan LR, Castanheira M (2017) Ceftolozane/tazobactam activity against drug-resistant Enterobacteriaceae and Pseudomonas aeruginosa causing urinary tract and intraabdominal infections in Europe: report from an antimicrobial surveillance programme (2012–15). J Antimicrob Chemother 72:1386–1395
Pfaller MA, Shortridge D, Sader HS, Gales A, Castanheira M, Flamm RK (2017) Ceftolozane-tazobactam activity against drug-resistant Enterobacteriaceae and Pseudomonas aeruginosa causing healthcare-associated infections in Latin America: report from an antimicrobial surveillance program (2013–2015). Braz J Infect Dis 21:627–637
Sid Ahmed MA, Abdel Hadi H, Hassan AAI, Abu Jarir S, Al-Maslamani MA, Eltai NO, Dousa KM, Hujer AM, Sultan AA, Soderquist B, Bonomo RA, Ibrahim EB, Jass J, Omrani AS (2019) Evaluation of in vitro activity of ceftazidime/avibactam and ceftolozane/tazobactam against MDR Pseudomonas aeruginosa isolates from Qatar. J Antimicrob Chemother 74:3497–3504
Alatoom A, Elsayed H, Lawlor K, AbdelWareth L, El-Lababidi R, Cardona L, Mooty M, Bonilla MF, Nusair A, Mirza I (2017) Comparison of antimicrobial activity between ceftolozane-tazobactam and ceftazidime-avibactam against multidrug-resistant isolates of Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa. Int J Infect Dis 62:39–43
Zowawi HM, Balkhy HH, Walsh TR, Paterson DL (2013) β-Lactamase production in key gram-negative pathogen isolates from the Arabian Peninsula. Clin Microbiol Rev l 26:361–380
Eagye KJ, Banevicius MA, Nicolau DP (2012) Pseudomonas aeruginosa is not just in the intensive care unit any more: implications for empirical therapy. Crit Care Med 40:1329–1332
Acknowledgements
We would like to acknowledge all members of the ERACE-PA Global Study Group: Julia Wille, Thais Teles Freitas Rezende, Zuhal Cekin, Gulsah Malkocoglu, Desirèe Gijón, Layla Abdullah Tarakmeh , Chun Yat Chu, Christoffel Johannes Opperman, Hafsah Deepa Tootla, Clinton Moodley, Jennifer Coetzee, Sophia Vourli, George Dimopolus, Dalya M. Attallah, Giusy Tiseo, Alessandro Leonildi, Cesira Giordano, Simona Barnini, Francesco Menichetti, Vincenzo Di Pilato, Giulia Codda, Antonio Vena, Daniele Roberto Giacobbe, Lars Westblade, Armando Cardona, Lauren Curtis, Ferric Fang, and Gina Thomson.
We thank Isabella Tickler and Deborah Santini for their superior assistance in coordination and conduct of genotypic testing. We would like to thank the staff from the Center for Anti-Infective Research and Development for their assistance in the conduct of this study.
Funding
The GeneXpert System and CarbaR Cartridges were supplied by Cepheid Sunnyvale, CA. CarbaR NxG testing and whole genome sequencing was conducted by Cepheid Sunnyvale, CA. All other resources necessary to conduct the study were internally funded by the Center for Anti-Infective Research and Development.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Hartford Hospital’s IRB as not conducting human subject research.
Conflict of interest
A.B. is a speaker bureau member of Merck, Pfizer, and has received research support from FIND. H.S. has received grants or research support from the German Research Foundation (DFG) and the German Centre for Infection Research (DZIF). H.S. is a consultant or speaker bureau member for Basilea, Entasis, Eumedica, Gilead, MSD, and Shionogi. D.P.N. is a consultant, speaker bureau member or has received research support from Abbvie, Cepheid, Merck, Paratek, Pfizer, Wockhardt, Shionogi, and Tetraphase. All other authors non to declare.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gill, C.M., Aktaþ, E., Alfouzan, W. et al. The ERACE-PA Global Surveillance Program: Ceftolozane/tazobactam and Ceftazidime/avibactam in vitro Activity against a Global Collection of Carbapenem-resistant Pseudomonas aeruginosa. Eur J Clin Microbiol Infect Dis 40, 2533–2541 (2021). https://doi.org/10.1007/s10096-021-04308-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-021-04308-0