Abstract
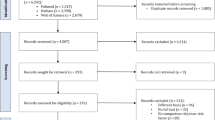
Previous studies have shown increased risk of herpes zoster (HZ) infection in patients with inflammatory bowel disease (IBD). The aim of this study is to better characterize this possible association by conducting a meta-analysis. A comprehensive search of relevant literature until April 30, 2019, was performed. Data on HZ infection and medications in patients with IBD and controls were extracted. The relative risk (RR) and 95% confidence interval (CI) were calculated. Subgroup analyses were performed to assess the source of heterogeneity. Seven cohort studies were included that involved more than 1,000,000 participants. The RR of HZ infection in patients with Crohn’s disease (CD) compared with non-CD patients was 1.74 (95% CI 1.57–1.92, p < 0.001). The pooled RR of HZ infection in patients with ulcerative colitis (UC) compared with non-UC was 1.40 (95% CI 1.31–1.50, p < 0.001). Subgroup analyses revealed that age, race, and publication year contribute to heterogeneity. We also found that steroid users were at increased risk of HZ in CD (OR = 1.78, 95% CI 1.10–2.88). Steroid users and anti-TNFα users were at increased risk of HZ in UC, with RRs of 1.99 (95% CI 1.64–2.42) and 2.29 (95% CI 1.52–3.45), respectively. Begg’s test and Egger’s test suggested no publication bias. There was a 74% increased risk of HZ infection in patients with CD and 40% increased risk of HZ infection in patients with UC compared with that in non-IBD. IBD patients with high risk of HZ infection may benefit from an HZ vaccine.




Similar content being viewed by others
References
Park JH, Peyrin-Biroulet L, Eisenhut M, Shin JI (2017) IBD immunopathogenesis: a comprehensive review of inflammatory molecules. Autoimmun Rev 16(4):416–426. https://doi.org/10.1016/j.autrev.2017.02.013
Bernstein CN, Fried M, Krabshuis JH, Cohen H, Eliakim R, Fedail S, Gearry R, Goh KL, Hamid S, Khan AG, LeMair AW, Malfertheiner OQ, Rey JF, Sood A, Steinwurz F, Thomsen OO, Thomson A, Watermeyer G (2010) World Gastroenterology Organization practice guidelines for the diagnosis and management of IBD in 2010. Inflamm Bowel Dis 16(1):112–124. https://doi.org/10.1002/ibd.21048
Khan N, Patel D, Trivedi C, Shah Y, Lichtenstein G, Lewis J, Yang YX (2018) Overall and comparative risk of herpes zoster with pharmacotherapy for inflammatory bowel diseases: a nationwide cohort study. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association 16(12):1919–1927.e1913. https://doi.org/10.1016/j.cgh.2017.12.052
Kirchgesner J, Lemaitre M, Carrat F, Zureik M, Carbonnel F, Dray-Spira R (2018) Risk of serious and opportunistic infections associated with treatment of inflammatory bowel diseases. Gastroenterology 155(2):337–346.e310. https://doi.org/10.1053/j.gastro.2018.04.012
Bonovas S, Fiorino G, Allocca M, Lytras T, Nikolopoulos GK, Peyrin-Biroulet L, Danese S (2016) Biologic therapies and risk of infection and malignancy in patients with inflammatory bowel disease: a systematic review and network meta-analysis. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association 14(10):1385–1397.e1310. https://doi.org/10.1016/j.cgh.2016.04.039
Yawn BP, Saddier P, Wollan PC, St Sauver JL, Kurland MJ, Sy LS (2007) A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc 82(11):1341–1349
Lin YH, Huang LM, Chang IS, Tsai FY, Lu CY, Shao PL, Chang LY (2010) Disease burden and epidemiology of herpes zoster in pre-vaccine Taiwan. Vaccine 28(5):1217–1220. https://doi.org/10.1016/j.vaccine.2009.11.029
Harpaz R, Ortega-Sanchez IR, Seward JF (2008) Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR recommendations and reports : morbidity and mortality weekly report recommendations and reports 57(Rr-5):1–30 quiz CE32-34
Forbes HJ, Bhaskaran K, Thomas SL, Smeeth L, Clayton T, Langan SM (2014) Quantification of risk factors for herpes zoster: population based case-control study. BMJ (Clinical research ed) 348:g2911. https://doi.org/10.1136/bmj.g2911
Smitten AL, Choi HK, Hochberg MC, Suissa S, Simon TA, Testa MA, Chan KA (2007) The risk of herpes zoster in patients with rheumatoid arthritis in the United States and the United Kingdom. Arthritis Rheum 57(8):1431–1438. https://doi.org/10.1002/art.23112
Cote-Daigneault J, Bessissow T, Nicolae MV, Nie R, Bitton A, Lakatos PL, Brassard P (2018) Herpes zoster incidence in inflammatory bowel disease patients: a population-based study. Inflamm Bowel Dis. https://doi.org/10.1093/ibd/izy311
Gupta G, Lautenbach E, Lewis JD (2006) Incidence and risk factors for herpes zoster among patients with inflammatory bowel disease. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association 4(12):1483–1490. https://doi.org/10.1016/j.cgh.2006.09.019
Long MD, Martin C, Sandler RS, Kappelman MD (2013) Increased risk of herpes zoster among 108 604 patients with inflammatory bowel disease. Aliment Pharmacol Ther 37(4):420–429. https://doi.org/10.1111/apt.12182
Soh H, Chun J, Han K, Park S, Choi G, Kim JH, Lee J, Im JP, Kim JS (2018) Increased risk of herpes zoster in young and metabolically healthy patients with inflammatory bowel disease: a nationwide population-based study. Gut and liver. https://doi.org/10.5009/gnl18304
Tsai SY, Yang TY, Lin CL, Tsai YH, Kuo CF, Kao CH (2015) Increased risk of varicella zoster virus infection in inflammatory bowel disease in an Asian population: a nationwide population-based cohort study. Int J Clin Pract 69(2):228–234. https://doi.org/10.1111/ijcp.12508
Chang K, Lee HS, Kim YJ, Kim SO, Kim SH, Lee SH, Song EM, Hwang SW, Park SH, Yang DH, Ye BD, Byeon JS, Myung SJ, Yang SK (2018) Increased risk of herpes zoster infection in patients with inflammatory bowel diseases in Korea. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association 16(12):1928–1936.e1922. https://doi.org/10.1016/j.cgh.2018.05.024
Marehbian J, Arrighi HM, Hass S, Tian H, Sandborn WJ (2009) Adverse events associated with common therapy regimens for moderate-to-severe Crohn’s disease. Am J Gastroenterol 104(10):2524–2533. https://doi.org/10.1038/ajg.2009.322
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605. https://doi.org/10.1007/s10654-010-9491-z
Siristatidis C, Sergentanis TN, Kanavidis P, Trivella M, Sotiraki M, Mavromatis I, Psaltopoulou T, Skalkidou A, Petridou ET (2013) Controlled ovarian hyperstimulation for IVF: impact on ovarian, endometrial and cervical cancer--a systematic review and meta-analysis. Hum Reprod Update 19(2):105–123. https://doi.org/10.1093/humupd/dms051
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ (Clinical research ed) 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Khan N, Trivedi C, Kavani H, Medvedeva E, Lewis J, Yang YX (2018) Efficacy of live attenuated herpes zoster vaccine in patients with inflammatory bowel diseases. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. https://doi.org/10.1016/j.cgh.2018.10.016
Che H, Lukas C, Morel J, Combe B (2014) Risk of herpes/herpes zoster during anti-tumor necrosis factor therapy in patients with rheumatoid arthritis. Systematic review and meta-analysis. Joint, bone, spine : revue du rhumatisme 81(3):215–221. https://doi.org/10.1016/j.jbspin.2013.07.009
Marra F, Lo E, Kalashnikov V, Richardson K (2016) Risk of herpes zoster in individuals on biologics, disease-modifying antirheumatic drugs, and/or corticosteroids for autoimmune diseases: a systematic review and meta-analysis. Open forum infectious diseases 3(4):ofw205. https://doi.org/10.1093/ofid/ofw205
Winthrop KL, Baddley JW, Chen L, Liu L, Grijalva CG, Delzell E, Beukelman T, Patkar NM, Xie F, Saag KG, Herrinton LJ, Solomon DH, Lewis JD, Curtis JR (2013) Association between the initiation of anti-tumor necrosis factor therapy and the risk of herpes zoster. Jama 309(9):887–895. https://doi.org/10.1001/jama.2013.1099
Sandborn WJ, Ghosh S, Panes J, Vranic I, Su C, Rousell S, Niezychowski W (2012) Tofacitinib, an oral Janus kinase inhibitor, in active ulcerative colitis. N Engl J Med 367(7):616–624. https://doi.org/10.1056/NEJMoa1112168
Winthrop KL, Melmed GY, Vermeire S, Long MD, Chan G, Pedersen RD, Lawendy N, Thorpe AJ, Nduaka CI, Su C (2018) Herpes zoster infection in patients with ulcerative colitis receiving tofacitinib. Inflamm Bowel Dis 24(10):2258–2265. https://doi.org/10.1093/ibd/izy131
Farraye FA, Melmed GY, Lichtenstein GR, Kane SV (2017) ACG clinical guideline: preventive care in inflammatory bowel disease. Am J Gastroenterol 112(2):241–258. https://doi.org/10.1038/ajg.2016.537
Rahier JF, Magro F, Abreu C, Armuzzi A, Ben-Horin S, Chowers Y, Cottone M, de Ridder L, Doherty G, Ehehalt R, Esteve M, Katsanos K, Lees CW, Macmahon E, Moreels T, Reinisch W, Tilg H, Tremblay L, Veereman-Wauters G, Viget N, Yazdanpanah Y, Eliakim R, Colombel JF (2014) Second European evidence-based consensus on the prevention, diagnosis and management of opportunistic infections in inflammatory bowel disease. J Crohns Colitis 8(6):443–468. https://doi.org/10.1016/j.crohns.2013.12.013
Zhang J, Xie F, Delzell E, Chen L, Winthrop KL, Lewis JD, Saag KG, Baddley JW, Curtis JR (2012) Association between vaccination for herpes zoster and risk of herpes zoster infection among older patients with selected immune-mediated diseases. Jama 308(1):43–49. https://doi.org/10.1001/jama.2012.7304
Khan N, Shah Y, Trivedi C, Lewis JD (2017) Safety of herpes zoster vaccination among inflammatory bowel disease patients being treated with anti-TNF medications. Aliment Pharmacol Ther 46(7):668–672. https://doi.org/10.1111/apt.14257
Khan N, Trivedi C, Shah Y, Patel D, Lewis J, Yang YX (2018) The severity of herpes zoster in inflammatory bowel disease patients treated with anti-TNF agents. Inflamm Bowel Dis 24(6):1274–1279. https://doi.org/10.1093/ibd/izx115
Wasan SK, Zullow S, Berg A, Cheifetz AS, Ganley-Leal L, Farraye FA (2016) Herpes zoster vaccine response in inflammatory bowel disease patients on low-dose immunosuppression. Inflamm Bowel Dis 22(6):1391–1396. https://doi.org/10.1097/mib.0000000000000743
Thomas SL, Hall AJ (2004) What does epidemiology tell us about risk factors for herpes zoster? Lancet Infect Dis 4(1):26–33
Tseng HF, Smith N, Harpaz R, Bialek SR, Sy LS, Jacobsen SJ (2011) Herpes zoster vaccine in older adults and the risk of subsequent herpes zoster disease. Jama 305(2):160–166. https://doi.org/10.1001/jama.2010.1983
Funding
This work was supported by the grants from Medical Science Research Foundation of Health Bureau of Zhejiang Province (WKJ-ZJ-1516).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Irrelevant due to study design.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ning, L., Liu, R., Li, S. et al. Increased risk of herpes zoster infection in patients with inflammatory bowel disease: a meta-analysis of cohort studies. Eur J Clin Microbiol Infect Dis 39, 219–227 (2020). https://doi.org/10.1007/s10096-019-03706-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-019-03706-9