Abstract
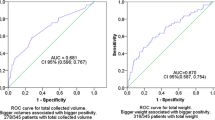
The introduction of dedicated phlebotomy teams certified for blood collection has been reported to be highly cost-effective by reducing contamination rates. However, data on their effects on blood volume and true positive rate are limited. Therefore, we investigated the effect of replacing interns with a phlebotomy team on blood culture results. We performed a 24-month retrospective, quasi-experimental study before and after the introduction of a phlebotomy team dedicated to collecting blood cultures in a 2700-bed tertiary-care hospital. The microbiology laboratory database was used to identify adult patients with positive blood culture results. During the study period, there were no changes in blood collection method, blood culture tubes, and the application of antiseptic measures. Blood volume was measured by the BACTEC™ FX system based on red blood cell metabolism. A total of 162,207 blood cultures from 23,563 patients were analyzed, comprising 78,673 blood cultures during the intern period and 83,534 during the phlebotomy team period. Blood volume increased from a mean of 2.1 ml in the intern period to a mean of 5.6 ml in the phlebotomy team period (p < 0.001). Introduction of the phlebotomy team also reduced contamination rate (0.27% vs. 0.45%, p < 0.001) and led to a higher true positive rate (5.87% vs. 5.01%, p < 0.05). The increased true positive rate associated with the phlebotomy team involved both gram-positive and gram-negative bacteria. The introduction of a dedicated phlebotomy team can increase blood volumes, reduce blood culture contamination rate, and increase true positive rate.
Similar content being viewed by others
References
Goto M, Al-Hasan MN (2013) Overall burden of bloodstream infection and nosocomial bloodstream infection in North America and Europe. Clin Microbiol Infect 19(6):501–509
Souvenir D, Anderson DE Jr, Palpant S, Mroch H, Askin S, Anderson J, Claridge J, Eiland J, Malone C, Garrison MW, Watson P, Campbell DM (1998) Blood cultures positive for coagulase-negative staphylococci: antisepsis, pseudobacteremia, and therapy of patients. J Clin Microbiol 36(7):1923–1926
Tepus D, Fleming E, Cox S, Hazelett S, Kropp D (2008) Effectiveness of Chloraprep in reduction of blood culture contamination rates in emergency department. J Nurs Care Qual 23(3):272–276
Gander RM, Byrd L, DeCrescenzo M, Hirany S, Bowen M, Baughman J (2009) Impact of blood cultures drawn by phlebotomy on contamination rates and health care costs in a hospital emergency department. J Clin Microbiol 47(4):1021–1024
Weightman NC, Kerr KG (2012) Blood culture contamination: having your cake and eating it. J Hosp Infect 80(1):101–102
Weinbaum FI, Lavie S, Danek M, Sixsmith D, Heinrich GF, Mills SS (1997) Doing it right the first time: quality improvement and the contaminant blood culture. J Clin Microbiol 35(3):563–565
Sheppard C, Franks N, Nolte F, Fantz C (2008) Improving quality of patient care in an emergency department: a laboratory perspective. Am J Clin Pathol 130(4):573–577
Leibovici L, Shraga I, Drucker M, Konigsberger H, Samra Z, Pitlik SD (1998) The benefit of appropriate empirical antibiotic treatment in patients with bloodstream infection. J Intern Med 244(5):379–386
Tenney JH, Reller LB, Mirrett S, Wang WL, Weinstein MP (1982) Controlled evaluation of the volume of blood cultured in detection of bacteremia and fungemia. J Clin Microbiol 15(4):558–561
Mermel LA, Maki DG (1993) Detection of bacteremia in adults: consequences of culturing an inadequate volume of blood. Ann Intern Med 119(4):270–272
Li J, Plorde JJ, Carlson LG (1994) Effects of volume and periodicity on blood cultures. J Clin Microbiol 32(11):2829–2831
Willems E, Smismans A, Cartuyvels R, Coppens G, Van Vaerenbergh K, Van den Abeele AM, Frans J, Bilulu Study G (2012) The preanalytical optimization of blood cultures: a review and the clinical importance of benchmarking in 5 Belgian hospitals. Diagn Microbiol Infect Dis 73(1):1–8
Coorevits L, Van den Abeele AM (2015) Evaluation of the BD BACTEC FX blood volume monitoring system as a continuous quality improvement measure. Eur J Clin Microbiol Infect Dis 34(7):1459–1466
Clinical and Laboratory Standards Institue (2007) Principles and procedures for blood cultures; approved guideline. CLSI document M47-A. Clinical and Laboratory Standards Institute, Wayne
Garcia RA, Spitzer ED, Beaudry J, Beck C, Diblasi R, Gilleeny-Blabac M, Haugaard C, Heuschneider S, Kranz BP, McLean K, Morales KL, Owens S, Paciella ME, Torregrosa E (2015) Multidisciplinary team review of best practices for collection and handling of blood cultures to determine effective interventions for increasing the yield of true-positive bacteremias, reducing contamination, and eliminating false-positive central line-associated bloodstream infections. Am J Infect Control 43(11):1222–1237
So M-K, Chung H-S, Kim C-J, Choi HJ, Lee M (2016) Effects of blood volume monitoring on the rate of positive blood cultures from the emergency room. Ann Clin Microbiol 19(3):70–75
Donnino MW, Goyal N, Terlecki TM, Donnino KF, Miller JB, Otero RM, Howell MD (2007) Inadequate blood volume collected for culture: a survey of health care professionals. Mayo Clin Proc 82(9):1069–1072
Vitrat-Hincky V, Francois P, Labarere J, Recule C, Stahl JP, Pavese P (2011) Appropriateness of blood culture testing parameters in routine practice. Results from a cross-sectional study. Eur J Clin Microbiol Infect Dis 30(4):533–539
van Ingen J, Hilt N, Bosboom R (2013) Education of phlebotomy teams improves blood volume in blood culture bottles. J Clin Microbiol 51(3):1020–1021
Chang J, Park JS, Park S, Choi B, Yoon NS, Sung H, Kim MN (2015) Impact of monitoring blood volume in the BD BACTEC FX blood culture system: virtual volume versus actual volume. Diagn Microbiol Infect Dis 81(2):89–93
Shin JH, Song SA, Kim MN, Lee NY, Kim EC, Kim S, Koo SH, Ryoo NH, Kim JS, Cho JH (2011) Comprehensive analysis of blood culture performed at nine university hospitals in Korea. Korean J Lab Med 31(2):101–106
Bekeris LG, Tworek JA, Walsh MK, Valenstein PN (2005) Trends in blood culture contamination: a College of American Pathologists Q-Tracks study of 356 institutions. Arch Pathol Lab Med 129(10):1222–1225
Self WH, Talbot TR, Paul BR, Collins SP, Ward MJ (2014) Cost analysis of strategies to reduce blood culture contamination in the emergency department: sterile collection kits and phlebotomy teams. Infect Control Hosp Epidemiol 35(8):1021–1028
Gilligan PH, York MK (2016) General detection and interpretation. In: Leber AL (ed) Clinical microbiology procedures handbook, 4th edn. American Society of Microbiology, Washington, DC, pp 121–151
Acknowledgements
This work was supported by a grant from the Korea Healthcare Technology R&D Project, Ministry for Health and Welfare, Republic of Korea (grant number HI12C0756). The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Table S1
(PDF 98 kb)
Rights and permissions
About this article
Cite this article
Bae, M., In Kim, H., Park, J.H. et al. Improvement of blood culture contamination rate, blood volume, and true positive rate after introducing a dedicated phlebotomy team. Eur J Clin Microbiol Infect Dis 38, 325–330 (2019). https://doi.org/10.1007/s10096-018-3430-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3430-4