Abstract
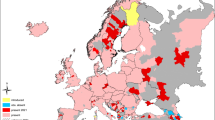
Leptospirosis is a zoonotic bacterial disease with a worldwide importance, mostly frequent in tropical and subtropical countries. In Côte d’Ivoire, little is known about leptospirosis and human data are sparse. This disease is usually misdiagnosed with other febrile illnesses, and determining high-risk areas could allow better management of this disease, leading to policies. This study aims to map leptospirosis exposure areas by determining geographic distribution of anti-Leptospira antibodies in humans in Côte d’Ivoire. A total of 384 serum samples were randomly selected in the national surveillance system for communicable diseases in 2014. All the 82 health districts were include in the study. Serums were screened by ELISA at Institut Pasteur de Côte d’Ivoire and confirmed by MAT in the National Reference Centre for leptospirosis in Institut Pasteur in Paris. In these samples, ELISA screened 90 specimens showing anti-Leptospira antibodies and 36 specimens were confirmed by MAT (9.4%). Observed cases were mostly located in health districts of the western and the southern parts of the country. People with anti-Leptospira antibodies had a mean age of 34.5 years old and a sex ratio of 2. This pattern corresponds to active low-income farmers working into agricultural fields. This study reveals circulation of leptospirosis in human population in Côte d’Ivoire. The disease seems to be more frequent in the western and the southern parts of the country. Active low-income farmers working into agricultural fields without personal protective gear could be one of the most at-risk populations.

Similar content being viewed by others
References
Haake DA, Levett PN (2015) Leptospirosis in humans. Curr Top Microbiol Immunol 387:65–97. https://doi.org/10.1007/978-3-662-45059-8_5
Hartskeerl RA, Collares-Pereira M, Ellis WA (2011) Emergence, control and re-emerging leptospirosis: dynamics of infection in the changing world. Clin Microbiol Infect 17:494–501. https://doi.org/10.1111/j.1469-0691.2011.03474.x
Costa F, Hagan JE, Calcagno J, Kane M, Torgerson P, Martinez-Silveira MS, Stein C, Abela-Ridder B, Ko AI (2015) Global morbidity and mortality of leptospirosis: a systematic review. PLoS Negl Trop Dis 9:e0003898. https://doi.org/10.1371/journal.pntd.0003898
De Vries SG, Visser BJ, Nagel IM, Goris MG, Hartskeerl RA, Grobusch MP (2014) Leptospirosis in sub-Saharan Africa: a systematic review. Int J Infect Dis 28:47–64
Allan KJ, Biggs HM, Halliday JEB, Kazwala RR, Maro VP, Cleaveland S, Crump JA (2015) Epidemiology of leptospirosis in Africa: a systematic review of a neglected zoonosis and a paradigm for ‘One Health’ in Africa. PLoS Negl Trop Dis 9:3899–3899
Roqueplo C, Marié JL, André-Fontaine G, Kodjo A, Davoust B (2015) Serological survey of canine leptospirosis in three countries of tropical Africa: Sudan, Gabon and Ivory Coast. Comp Immunol Microbiol Infect Dis 38:57–61. https://doi.org/10.1016/j.cimid.2014.10.006
Bourhy P, Vray M, Picardeau M (2013) Evaluation of an in-house ELISA using the intermediate species Leptospira fainei for diagnosis of leptospirosis. J Med Microbiol 62(Pt 6):822–827
R Core Team (2015) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL http://www.R-project.org
Pappas G, Papadimitriou P, Siozopoulou V, Christou L, Akritidis N (2008) The globalization of leptospirosis: worldwide incidence trends. Int J Infect Dis 12(4):351–357
Adler B, De La Pena MA (2010) Leptospira and leptospirosis. Vet Microbiol 140:287–296. https://doi.org/10.1016/j.vetmic.2009.03.012
Faine S, Adler B, Bolin C, Pérolat P (1999) Leptospira and leptospirosis. MediSci, Melbourne, 296 p
Levett PN (2001) Leptospirosis. Clin Microbiol Rev 14(2):296–326
Stamm LV, Charon NW (1988) Sensitivity of pathogenic and free-living Leptospira spp. to UV radiation and mitomycin C. Appl Environ Microbiol 54(3):728–733
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The national ethic and research committee of Côte d’Ivoire approved this study under the number 23/MSLS/CNER-dkn.
Informed consent
Not applicable.
Rights and permissions
About this article
Cite this article
Koffi, S.K., Meite, S., Ouattara, A. et al. Geographic distribution of anti-Leptospira antibodies in humans in Côte d’Ivoire, West Africa. Eur J Clin Microbiol Infect Dis 37, 2177–2180 (2018). https://doi.org/10.1007/s10096-018-3359-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3359-7