Abstract
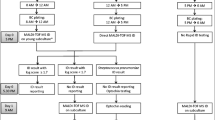
Matrix-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOF MS) considerably reduces timeframe required from initial blood culture positivity towards complete bacterial identification. However, rapid identification of polymicrobial blood cultures remains challenging. We evaluated the performances of the Bruker® MBT Sepsityper IVD module on MALDI-TOF MS for the direct identification of polymicrobial blood culture bottles. This module has the ability to give a strong indication that a sample contains a mixture of organisms and to identify two of them. Blood culture bottles considered as polymicrobial using routine subculture were collected and processed using the Sepsityper kit. MALDI-TOF MS identification was performed using the MBT Compass IVD software including the Sepsityper module. From 143 polymicrobial blood culture bottles tested, 34.3% (49/143) were completely identified by the module. Both microorganisms were more easily detected by the module in samples containing two pathogens than in samples containing two contaminants (36.8% vs 29.4%). Additionally, in more than half of the samples, the module detected 1 of the different microorganisms contained in the same vial. In these cases, with a pathogen and contaminant in the same sample, the module detected the pathogen in more than 80%. The Sepsityper module identified 14 microorganisms which were not recovered by conventional culture methods. The Bruker® MBT Sepsityper IVD module contributed to a valuable identification of polymicrobial blood cultures in more than a third of all cases. Conventional culture methods are still required to complete the results and to carry on susceptibility testing.



Similar content being viewed by others
References
Diekema DJ, Beekmann SE, Chapin KC, Morel KA, Munson E, Doern GV (2003) Epidemiology and outcome of nosocomial and community-onset bloodstream infection. J Clin Microbiol 41(8):3655–3660
Bearman GM, Wenzel RP (2005) Bacteremias: a leading cause of death. Arch Med Res 36(6):646–659. https://doi.org/10.1016/j.arcmed.2005.02.005
Goto M, Al-Hasan MN (2013) Overall burden of bloodstream infection and nosocomial bloodstream infection in North America and Europe. Clin Microbiol Infect 19(6):501–509. https://doi.org/10.1111/1469-0691.12195
Lenz R, Leal JR, Church DL, Gregson DB, Ross T, Laupland KB (2012) The distinct category of healthcare associated bloodstream infections. BMC Infect Dis 12:85. https://doi.org/10.1186/1471-2334-12-85
Luzzaro F, Ortisi G, Larosa M, Drago M, Brigante G, Gesu G (2011) Prevalence and epidemiology of microbial pathogens causing bloodstream infections: results of the OASIS multicenter study. Diagn Microbiol Infect Dis 69(4):363–369. https://doi.org/10.1016/j.diagmicrobio.2010.10.016
Royo-Cebrecos C, Gudiol C, Ardanuy C, Pomares H, Calvo M, Carratala J (2017) A fresh look at polymicrobial bloodstream infection in cancer patients. PLoS One 12(10):e0185768. https://doi.org/10.1371/journal.pone.0185768
Bouza E, Burillo A, Munoz P, Guinea J, Marin M, Rodriguez-Creixems M (2013) Mixed bloodstream infections involving bacteria and Candida spp. J Antimicrob Chemother 68(8):1881–1888. https://doi.org/10.1093/jac/dkt099
Lin JN, Lai CH, Chen YH, Chang LL, Lu PL, Tsai SS, Lin HL, Lin HH (2010) Characteristics and outcomes of polymicrobial bloodstream infections in the emergency department: a matched case-control study. Acad Emerg Med 17(10):1072–1079. https://doi.org/10.1111/j.1553-2712.2010.00871.x
Pammi M, Zhong D, Johnson Y, Revell P, Versalovic J (2014) Polymicrobial bloodstream infections in the neonatal intensive care unit are associated with increased mortality: a case-control study. BMC Infect Dis 14:390. https://doi.org/10.1186/1471-2334-14-390
Rolston KV, Bodey GP, Safdar A (2007) Polymicrobial infection in patients with cancer: an underappreciated and underreported entity. Clin Infect Dis 45(2):228–233. https://doi.org/10.1086/518873
Tsai MH, Chu SM, Hsu JF, Lien R, Huang HR, Chiang MC, Fu RH, Lee CW, Huang YC (2014) Polymicrobial bloodstream infection in neonates: microbiology, clinical characteristics, and risk factors. PLoS One 9(1):e83082. https://doi.org/10.1371/journal.pone.0083082
Kim SH, Yoon YK, Kim MJ, Sohn JW (2013) Risk factors for and clinical implications of mixed Candida/bacterial bloodstream infections. Clin Microbiol Infect 19(1):62–68. https://doi.org/10.1111/j.1469-0691.2012.03906.x
Lagnf AM, Zasowski EJ, Claeys KC, Casapao AM, Rybak MJ (2016) Comparison of clinical outcomes and risk factors in polymicrobial versus monomicrobial enterococcal bloodstream infections. Am J Infect Control 44(8):917–921. https://doi.org/10.1016/j.ajic.2016.02.017
Park SY, Park KH, Bang KM, Chong YP, Kim SH, Lee SO, Choi SH, Jeong JY, Woo JH, Kim YS (2012) Clinical significance and outcome of polymicrobial Staphylococcus aureus bacteremia. J Inf Secur 65(2):119–127. https://doi.org/10.1016/j.jinf.2012.02.015
Sutter D, Stagliano D, Braun L, Williams F, Arnold J, Ottolini M, Epstein J (2008) Polymicrobial bloodstream infection in pediatric patients: risk factors, microbiology, and antimicrobial management. Pediatr Infect Dis J 27(5):400–405. https://doi.org/10.1097/INF.0b013e31816591be
Dixon P, Davies P, Hollingworth W, Stoddart M, MacGowan A (2015) A systematic review of matrix-assisted laser desorption/ionisation time-of-flight mass spectrometry compared to routine microbiological methods for the time taken to identify microbial organisms from positive blood cultures. Eur J Clin Microbiol Infect Dis 34(5):863–876. https://doi.org/10.1007/s10096-015-2322-0
Idelevich EA, Schule I, Grunastel B, Wullenweber J, Peters G, Becker K (2014) Rapid identification of microorganisms from positive blood cultures by MALDI-TOF mass spectrometry subsequent to very short-term incubation on solid medium. Clin Microbiol Infect 20(10):1001–1006. https://doi.org/10.1111/1469-0691.12640
Jakovljev A, Bergh K (2015) Development of a rapid and simplified protocol for direct bacterial identification from positive blood cultures by using matrix assisted laser desorption ionization time-of- flight mass spectrometry. BMC Microbiol 15:258. https://doi.org/10.1186/s12866-015-0594-2
Kohlmann R, Hoffmann A, Geis G, Gatermann S (2015) MALDI-TOF mass spectrometry following short incubation on a solid medium is a valuable tool for rapid pathogen identification from positive blood cultures. Int J Med Microbiol 305(4–5):469–479. https://doi.org/10.1016/j.ijmm.2015.04.004
Morgenthaler NG, Kostrzewa M (2015) Rapid identification of pathogens in positive blood culture of patients with sepsis: review and meta-analysis of the performance of the sepsityper kit. Int J Microbiol 2015:827416. https://doi.org/10.1155/2015/827416
Verroken A, Defourny L, Lechgar L, Magnette A, Delmee M, Glupczynski Y (2015) Reducing time to identification of positive blood cultures with MALDI-TOF MS analysis after a 5-h subculture. Eur J Clin Microbiol Infect Dis 34(2):405–413. https://doi.org/10.1007/s10096-014-2242-4
Centers for Disease Control and Prevention. Atlanta. National Healthcare Safety Network CDC/NHSN bloodstream infection event (central line-associated infection and non-central line-associated bloodstream infection) (Update January 2016) http://www.cdc.gov/nhsn/PDFs/pscManual/4PSC_CLABScurrent.pdf
Kumar A, Ellis P, Arabi Y, Roberts D, Light B, Parrillo JE, Dodek P, Wood G, Kumar A, Simon D, Peters C, Ahsan M, Chateau D, Cooperative Antimicrobial Therapy of Septic Shock Database Research G (2009) Initiation of inappropriate antimicrobial therapy results in a fivefold reduction of survival in human septic shock. Chest 136(5):1237–1248. https://doi.org/10.1378/chest.09-0087
Pulimood S, Ganesan L, Alangaden G, Chandrasekar P (2002) Polymicrobial candidemia. Diagn Microbiol Infect Dis 44(4):353–357
Valles J, Rello J, Ochagavia A, Garnacho J, Alcala MA (2003) Community-acquired bloodstream infection in critically ill adult patients: impact of shock and inappropriate antibiotic therapy on survival. Chest 123(5):1615–1624
Beekmann SE, Diekema DJ, Chapin KC, Doern GV (2003) Effects of rapid detection of bloodstream infections on length of hospitalization and hospital charges. J Clin Microbiol 41(7):3119–3125
Norgaard M, Larsson H, Pedersen G, Schonheyder HC, Sorensen HT (2006) Haematological malignancies--a predictor of a poor outcome in patients with bacteraemia. J Inf Secur 53(3):190–198. https://doi.org/10.1016/j.jinf.2005.10.024
Sancho S, Artero A, Zaragoza R, Camarena JJ, Gonzalez R, Nogueira JM (2012) Impact of nosocomial polymicrobial bloodstream infections on the outcome in critically ill patients. Eur J Clin Microbiol Infect Dis 31(8):1791–1796. https://doi.org/10.1007/s10096-011-1503-8
Yamaga S, Shime N (2018) Association between appropriate empiric antimicrobial therapy and mortality from bloodstream infections in the intensive care unit. J Infect Chemother 24(4):267–271. https://doi.org/10.1016/j.jiac.2017.11.011
Kok J, Thomas LC, Olma T, Chen SC, Iredell JR (2011) Identification of bacteria in blood culture broths using matrix-assisted laser desorption-ionization Sepsityper and time of flight mass spectrometry. PLoS One 6(8):e23285. https://doi.org/10.1371/journal.pone.0023285
Hariu M, Watanabe Y, Oikawa N, Seki M (2017) Usefulness of matrix-assisted laser desorption ionization time-of-flight mass spectrometry to identify pathogens, including polymicrobial samples, directly from blood culture broths. Infect Drug Resist 10:115–120. https://doi.org/10.2147/IDR.S132931
La Scola B, Raoult D (2009) Direct identification of bacteria in positive blood culture bottles by matrix-assisted laser desorption ionisation time-of-flight mass spectrometry. PLoS One 4(11):e8041. https://doi.org/10.1371/journal.pone.0008041
Gajdacs M, Spengler G, Urban E (2017) Identification and antimicrobial susceptibility testing of anaerobic bacteria: Rubik’s cube of clinical microbiology? Antibiotics (Basel) 6(4). https://doi.org/10.3390/antibiotics6040025
Cateau E, Cognee AS, Tran TC, Vallade E, Garcia M, Belaz S, Kauffmann-Lacroix C, Rodier MH (2012) Impact of yeast-bacteria coinfection on the detection of Candida sp. in an automated blood culture system. Diagn Microbiol Infect Dis 72(4):328–331. https://doi.org/10.1016/j.diagmicrobio.2011.12.012
Hockey LJ, Fujita NK, Gibson TR, Rotrosen D, Montgomerie JZ, Edwards JE Jr (1982) Detection of fungemia obscured by concomitant bacteremia: in vitro and in vivo studies. J Clin Microbiol 16(6):1080–1085
Timbrook T, Boger MS, Steed LL, Hurst JM (2015) Unanticipated multiplex PCR-based identification of polymicrobial blood culture resulting in earlier isolation, determination of susceptibilities, and optimization of clinical care. J Clin Microbiol 53(7):2371–2373. https://doi.org/10.1128/JCM.00058-15
Altun O, Almuhayawi M, Ullberg M, Ozenci V (2013) Clinical evaluation of the FilmArray blood culture identification panel in identification of bacteria and yeasts from positive blood culture bottles. J Clin Microbiol 51(12):4130–4136. https://doi.org/10.1128/JCM.01835-13
Southern TR, VanSchooneveld TC, Bannister DL, Brown TL, Crismon AS, Buss SN, Iwen PC, Fey PD (2015) Implementation and performance of the BioFire FilmArray (R) Blood Culture Identification panel with antimicrobial treatment recommendations for bloodstream infections at a midwestern academic tertiary hospital. Diagn Microbiol Infect Dis 81(2):96–101. https://doi.org/10.1016/j.diagmicrobio.2014.11.004
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Testing was performed in accordance with the ethical standards of the Cliniques universitaires Saint-Luc, in accordance with the ethical standards of the national research committee, and in accordance with the 1964 Helsinki declaration and its later amendments.
Informed consent
Information from microbiological and clinical files was anonymously analyzed and did not require patient’s informed consent.
Rights and permissions
About this article
Cite this article
Scohy, A., Noël, A., Boeras, A. et al. Evaluation of the Bruker® MBT Sepsityper IVD module for the identification of polymicrobial blood cultures with MALDI-TOF MS. Eur J Clin Microbiol Infect Dis 37, 2145–2152 (2018). https://doi.org/10.1007/s10096-018-3351-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3351-2