Abstract
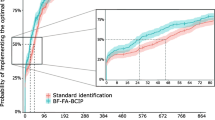
The objective of this study was to show the differences between paired blood cultures (PBC) versus single blood cultures (SBC) in the microbiologic yield, the sensitivity to detect pathogens and the time to positivity (TTP). We performed a retrospective study examining 112,570 blood culture samples over a 5-year period from July 2011 to May 2016 in the BacT/ALERT® 3D automated blood culture system (bioMérieux, Marcy l’Etoile, France). Bacteria and yeasts were identified using the VITEK® 2 Compact system (bioMérieux, Marcy l’Etoile, France). True-positives and contaminated bottles were defined and analysed separately. We analysed TTP and adherence to blood volume guidelines for a convenience sample of 510 and 999 sequential positive cultures, respectively. Out of 49,438 PBC samples, 5810 (11.7%) were positive. In 63,132 SBC samples, 4552 (7.2%) were positive (p < 0.0001). In PBC, 5371 (10.9%) were true-positives and 439 (0.9%) contaminants. In SBC, 4095 (6.5%) were true-positives and 457 (0.7%) contaminants. In the inpatient departments (IPD), the most common isolate was Escherichia coli (n = 1373), followed by Klebsiella pneumoniae (n = 1206), whereas in the outpatient departments (OPD), the most common isolates were Salmonella typhi (n = 612) and S. paratyphi A (n = 278). In the analysis of TTP, 98% grew within 72 h, 91% within 48 h and 89% within 36 h. In the blood volume analysis, 90% of the cultures had optimal blood volume. A significantly higher positivity rate was seen in PBC compared with SBC. Our study adds to the increasing evidence of improved microbial yield of clinically significant bacteria and fungi by performing PBC instead of SBC and adhering to blood volume collection guidelines.



Similar content being viewed by others
References
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb SA, Beale RJ, Vincent JL, Moreno R; Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup (2013) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 41:580–637
Khatib R, Saeed S, Sharma M, Riederer K, Fakih MG, Johnson LB (2006) Impact of initial antibiotic choice and delayed appropriate treatment on the outcome of Staphylococcus aureus bacteremia. Eur J Clin Microbial Infect Dis 25(3):181–185
Garey KW, Rege M, Pai MP, Mingo DE, Suda KJ, Turpin RS, Bearden DT (2006) Time to initiation of fluconazole therapy impacts mortality in patients with candidemia: a multi-institutional study. Clin Infect Dis 43(1):25–31
Clinical and Laboratory Standards Institute (CLSI) (2007) Principles and procedures for blood cultures; Approved guideline. CLSI document M47-A, volume 27 number 17
Mirrett S, Weinstein MP, Reimer LG, Wilson ML, Reller LB (2001) Relevance of the number of positive bottles in determining clinical significance of coagulase-negative staphylococci in blood cultures. J Clin Microbiol 39:3279–3281
Ntusi N, Aubin L, Oliver S, Whitelaw A, Mendelson M (2010) Guideline for the optimal use of blood cultures. S Afr Med J 100:839–843
Cockerill FR 3rd, Wilson JW, Vetter EA, Goodman KM, Torgerson CA, Harmsen WS, Schleck CD, Ilstrup DM, Washington JA 2nd, Wilson WR (2004) Optimal testing parameters for blood cultures. Clin Infect Dis 38:1724–1730
Lee A, Mirrett S, Reller LB, Weinstein MP (2007) Detection of bloodstream infections in adults: how many blood cultures are needed? J Clin Microbiol 45:3546–3548
Centers for Disease Control and Prevention (CDC) BSI event protocol, , January 2017. Available online at: https://www.cdc.gov/nhsn/pdfs/pscmanual/4psc_clabscurrent.pdf
Coburn B, Morris AM, Tomlinson G, Detsky AS (2012) Does this adult patient with suspected bacteremia require blood cultures? JAMA 308:502–511
Tarai B, Das P, Kumar D, Budhiraja S (2012) Comparative evaluation of paired blood culture (aerobic/aerobic) and single blood culture, along with clinical importance in catheter versus peripheral line at a tertiary care hospital. Indian J Med Microbiol 30:187–192
Oberoi JK, Wattal C, Goel N, Raveendran R, Datta S, Prasad K (2012) Non-albicans Candida species in blood stream infections in a tertiary care hospital at New Delhi, India. Indian J Med Res 136:997–1003
Rudramurthy SM, Chakrabarti A, Paul RA, Sood P, Kaur H, Capoor MR, Kindo AJ, Marak RSK, Arora A, Sardana R, Das S, Chhina D, Patel A, Xess I, Tarai B, Singh P, Ghosh A (2017) Candida auris candidaemia in Indian ICUs: analysis of risk factors. J Antimicrob Chemother 72:1794–1801
Suwantarat N, Carroll KC (2016) Epidemiology and molecular characterization of multidrug-resistant Gram-negative bacteria in Southeast Asia. Antimicrob Resist Infect Control 5:15
Mirrett S, Weinstein MP, Reimer LG, Wilson ML, Reller LB (1993) Interpretation of coagulase-negative staphylococci in blood cultures: does the number of positive bottles help? [Abstract C69.] In: Program and abstracts of the 93rd General Meeting of the American Society for Microbiology, Atlanta, Georgia, May 1993. American Society for Microbiology, Washington, DC, 458 pp
Peacock SJ, Bowler ICJW, Crook DWM (1995) Positive predictive value of blood cultures growing coagulase-negative staphylococci [letter]. Lancet 346:191–192
Bates DW, Goldman L, Lee TH (1991) Contaminant blood cultures and resource utilization: the true consequences of false-positive results. JAMA 265:365–369
Reimer LG, Wilson ML, Weinstein MP (1997) Update on detection of bacteremia and fungemia. Clin Microbiol Rev 10:444–465
Acknowledgements
The authors thankfully acknowledge the unrelenting efforts and technical expertise provided by Dr. Navjeet Singh, Head Medical Affairs, bioMérieux India. We also acknowledge Dr. Arunaloke Chakrabarti, HOD Microbiology, PGIMER Chandigarh and Dr. Shivaprakash M Rudramurthy for their support regarding further confirmation testing of samples.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest.
Ethical approval from institute
Approved.
Rights and permissions
About this article
Cite this article
Tarai, B., Jain, D., Das, P. et al. Paired blood cultures increase the sensitivity for detecting pathogens in both inpatients and outpatients. Eur J Clin Microbiol Infect Dis 37, 435–441 (2018). https://doi.org/10.1007/s10096-018-3188-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3188-8