Abstract
The performance and acceptability of first-void urine as specimen for the detection of HPV DNA in a Belgian referral population was evaluated using an optimized sample collection and processing protocol. One hundred ten first-void urine and cervical samples were collected from 25- to 64-year-old women who were referred for colposcopy (January–November 2016). Paired samples were analyzed by the Riatol qPCR HPV genotyping assay. Acceptability data were gathered through questionnaires (NCT02714127). A higher high-risk HPV DNA prevalence was observed in first-void urine (n = 76/110) compared to cervical samples (n = 73/110), with HPV31 and HPV16/31 being most prevalent correspondingly. For both any and high-risk HPV DNA, good agreement was observed between paired samples (Cohen’s Kappa of 0.660 (95% CI: 0.486–0.833) and 0.688 (95% CI: 0.542–0.835), respectively). In addition, significant positive correlations in HPV copies (per microliter of DNA extract) between paired samples were observed for HPV16 (rs = 0.670; FDR (false discovery rate)-adjusted p = 0.006), HPV18 (rs = 0.893; FDR-adjusted p = 0.031), HPV31 (rs = 0.527; FDR-adjusted p = 0.031), HPV53 (rs = 0.691; FDR-adjusted p = 0.017), and HPV68 (rs = 0.569; FDR-adjusted p = 0.031). First-void urine sampling using a first-void urine collection device was preferred over a clinician-collected cervical sample. And mostly, first-void urine sampling at home was favored over collection at the clinic or the general practitioner’s office. First-void urine sampling is a highly preferred, non-invasive method that ensures good agreement in HPV DNA (copies) with reference cervical samples. It is particularly interesting as a screening technique to reach non-participants, and its clinical performance should be further evaluated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
To date, cervical cancer (CxCa) remains a significant problem worldwide, representing the fourth most common cancer in women [1]. The identification of human papillomavirus (HPV) as the principal cause of CxCa and the ongoing improvement of diagnostic tools leading to high-throughput screening have changed the paradigm of CxCa prevention. Prophylactic HPV vaccines have been introduced that protect millions of women against HPV16/18, and recently, HPV16/18/31/33/45/52/58 associated CxCa and genital warts (HPV6/11) [2, 3]. HPV-based screening is currently of high interest, providing 60–70% greater protection against invasive CxCa compared to cytology-based screening [4, 5]. Nevertheless, challenges remain to attaining better uptake in screening programmes, as well as more accurate detection of HPV and triage markers in self-collected specimens [6]. These challenges can be diverse, and include practical, emotional, and cognitive barriers [7, 8]. HPV DNA testing on a self-sample has been proposed as an additional strategy to reach non-attendees [9, 10]. The impact of offering vaginal/cervical- [11,12,13] and urine-based [14] self-sampling to increase participation and screening coverage has become quite apparent. Non-invasive urine sampling has been recognized as the preferred choice for self-sampling compared to the currently available methods that involve the collection of vaginal/cervical material [15,16,17].
The use of first-void urine (FVU) as a liquid biopsy for HPV DNA testing is promising. High correlations have been established between urinary HPV DNA and cervical infections [18,19,20,21,22,23,24,25,26,27,28]. The theory put forward for identifying HPV DNA in the urine of women with vaginal or cervical HPV infections is based on the fact that during urination, the first part of the urine void (defined as first-void urine) captures mucus and debris from exfoliated cells from the female genital organs, including the cervix. This explains why the first collected part of a urine void contains significantly more HPV DNA than the subsequent part [25, 29]. There is also some remaining confusion regarding the definition of FVU, as it is often mistaken for the first urine of the day [29]. Adding a nucleic acid preservative to urine samples has proven effective to prevent nucleases from degrading cell-associated and cell-free DNA during transport, storage, and pre-analytical processing steps [30, 31]. In the last decade, the use of HPV type-specific copy number measurement in cervical samples (CS) for clinical management of HPV infections has been reported. However, the clinical utility of this method to differentiate between cervical precancerous grades remains challenging [32,33,34,35,36,37]. This raises the question (i) as to whether testing of (first-void) urine lacks the sensitivity and the ability to correlate between HPV copy number and a cervical precancerous state [38, 39], or (ii) whether a high concordance in HPV copy number exists between paired urine and CS [24], and (iii) if a correlation exists between HPV copy number and cervical precancerous state [23].
This study was designed as a pilot to investigate the presence of biomarkers in FVU for CxCa screening and triage of HPV-infected women, including HPV copy number as a candidate biomarker of interest. Therefore, HPV genotype agreement observed between paired FVU and CS was assessed using an optimized protocol for FVU collection, storage, and pre-analytical processing, in combination with a qPCR-based assay. In the present study, the HPV prevalence and (genotype) concordance between paired FVU and CS in a Belgian colposcopy cohort was investigated. Furthermore, we assessed the HPV copy number agreement between paired samples. Finally, we report on the acceptability of FVU sampling using a FVU collection device.
Materials and methods
Study participants
Women (aged 25–64) who were referred to the colposcopy clinic at the Antwerp University Hospital (UZA, Belgium) were screened for eligibility during January and November 2016 (NCT02714127). The criteria included referral due to abnormal cytology or infection with one or multiple HPV genotypes. Patients who underwent cervical conisation in the previous year were excluded. Women who fit the criteria were informed about the study and received an information brochure beforehand. Paired FVU and cervical HPV DNA genotyping results were available for 110 out of 127 eligible patients (Fig. 1). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (UZA/University of Antwerp, Belgium (B300201525585)) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. To ensure patient confidentiality, each study participant received a personal identifier number to which all data were linked.
Flow diagram for the inclusion of study participants, samples, and medical records. All 127 eligible patients received a questionnaire containing, next to personal, inquiries about the acceptability of first-void urine (FVU) collection. Surveys from 124 out of 127 women who provided a Colli-Pee® (Novosanis, Belgium) collected FVU sample were included to investigate acceptability. aWhen unavailable at D0 (day of study visit/FVU collection), the colposcopy, LBC (liquid based cytology), and histology results from D0 ± 3 months were included for data analysis instead. Thus, two additional colposcopy results were included, as well as one LBC and six histology results. No results were included from D0 ± 3 months if the woman underwent surgical treatment for high-grade cervical abnormalities in this period
Sample collection, processing, and storage
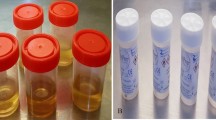
Upon arriving at the clinic, informed consent was obtained, and it was explained to women how to collect the FVU sample. Standard, illustrated instructions provided by the device company were also available. Women were asked to collect a FVU sample with the Colli-Pee® device (Novosanis, Belgium) prior to their visit with the gynecologist for a CS and colposcopy. Women were requested beforehand to not extensively wash their genitals before the visit at the clinic and to not urinate at least 1 h prior to this visit. Upon collection, FVU samples were immediately placed on ice and transported to the UZA laboratory, where they were aliquoted and preserved on dry ice before storage at −80 °C. For HPV DNA genotyping, one volume of urine conservation medium (UCM) [31] was added to two volumes of FVU before storage at −80 °C.
Data from CS (HPV DNA genotyping, liquid based cytology (LBC)) and colposcopy (with an optional biopsy) from D0 (day of the study visit) ± 3 months were retrieved from the medical records of each study participant. CS were collected with a Cervex-Brush® (Rovers Medical Devices, The Netherlands), which were transferred in 20 ml PreservCyt® collection medium (Hologic Europe, Belgium) and analyzed with the ThinPrep® Pap Test (Hologic Europe). During colposcopy, the cervix was visually inspected for abnormalities and graded as normal, low-, or high-grade cervical abnormality. When indicated, a biopsy for histological confirmation was taken. Women scheduled for an ambulant conisation were also included, as were their histology results from the conus. Both LBC and histology were performed at the UZA pathology laboratory and were graded according to the Bethesda and Cervical Intraepithelial Neoplasia (CIN) classifications, respectively. Women graded with different colposcopic and histological outcomes were classified according to the most severe stage. CS were taken, and colposcopies were performed by two colposcopists.
DNA extraction of first-void urine samples
UCM-buffered FVU aliquots were thawed (after storage for 2–12 months) and DNA extraction was performed with an in-house protocol [31]. Briefly, 4 ml of the aliquot was centrifuged at 3820 g for 20 min at 20 °C in an Amicon Ultra-4 50 K filter device (Merck Millipore, Belgium). Following filtration, 2 ml of NucliSENS® Lysis Buffer (BioMérieux, Benelux) was added to the concentrate retained on the filter and incubated for 10 min at ambient temperature. The solution retained on the filter was subsequently transferred to the NucliSENS Lysis Buffer vial before DNA extraction using NucliSENS® easyMAG® (BioMérieux, Benelux). DNA was eluted in 55 μl, after which 35 μl was transferred to a second vial with elution buffer (BioMérieux, Benelux) to reach a total volume of 75 μl of DNA extract used for HPV DNA genotyping.
HPV DNA genotyping
Cervical samples
HPV DNA genotyping of CS was performed with the Riatol qPCR HPV genotyping assay (Riatol assay), quantifying 12 high-risk (HR) (HPV16/18/31/33/35/39/45/51/52/56/58/59), one probable HR (HPV68), three possible HR (HPV53/66/67), and two low-risk (LR) (HPV6/11) HPV genotypes [40] and β-globin as described elsewhere [41, 42]. Briefly, 400–800 μl of the remaining LBC specimens were subjected to automatic nucleic acid preparation. Following extraction, HPV and β-globin were quantified using highly sensitive multiplex qPCR (LightCycler® 480, Roche, Switzerland), with 1–100 HPV copies detected per reaction (copies/μl). β-globin was amplified to assess the DNA quality and to determine the number of cells present in the sample. HPV DNA positivity was reported in HPV copies per cell by dividing the HPV copies per microliter (µl) DNA extract by the number of cells per µl. The positivity threshold was set at 0.0001 HPV copies per cell [42, 43]. HPV copies per cell, hereafter referred to as the human DNA (hDNA) equivalent, was calculated back to HPV copies per µl of DNA extract to enable comparison with FVU HPV DNA results.
First-void urine
HPV DNA genotyping using FVU DNA extracts was performed with the Riatol assay [41, 42] according to an optimized protocol for FVU [44]. The difference between the protocol used for CS and FVU was that, for the latter, DNA extracts were directly pipetted into the 96-well plate, followed by qPCR, bypassing the sample preparation and DNA extraction steps. FVU samples were subjected to batches in random order for DNA extraction and HPV DNA genotyping. The HPV DNA results were reported in copies per hDNA equivalent and per microliter of DNA extract for each genotype separately. The concentration of human and HPV DNA in nanogram (ng) and copies per µl of DNA extract was 44.08 times lower than in 1 ml of the original urine fraction. Thus, HPV DNA copies per µl of DNA extract should be multiplied by this factor or 1.64 logarithm-to-base 10 should be added to the log10 copies to determine human and HPV DNA copies per milliliter of FVU.
Statistical analysis
The percent correct and Cohen’s Kappa (κ) were calculated to assess the HPV genotype agreement between paired samples. In addition, the McNemar’s odds ratio (OR) and test were computed to compare the association between FVU or CS for a given HPV genotype. In case a zero cell count occurred, a constant of 1 was added to each cell in the table [45]. The Wilcoxon matched pairs signed rank test was used to test for differences in dependent continuous measures and for differences within levels of categorical measures. hDNA and HPV copy number correlations were calculated using Pearson and Spearman rank correlations, respectively. All p-values were corrected for multiple testing using the false discovery rate (FDR) method [46]. Statistical analyses were performed at a significance level of 5% using the statistical software R version 3.3.3 [47] and IBM SPSS Statistics Version 24. Additional graphs were generated using Excel Microsoft Office Professional Plus 2016 and JMP Pro 13.
Results
Study population
The median participant age in our study population was 36 (interquartile range (IQR): 29–44 years old), with a gradual decrease in the number of participants per increasing age group. LBC and HR-HPV results are detailed in Table 1 according to age group. Colposcopy results were available from 107 out of 110 women, with 29.91% classified as normal (n = 32/107), 52.34% with low-grade (n = 56/107), and 17.76% with high-grade cervical abnormality (n = 19/107). Histology results were available from 33 women and revealed that 33.33% of women had cervical intraepithelial neoplasia grade 1 (CIN1) (n = 11/33), 18.18% with CIN2 (n = 6/33), 27.27% with CIN3 (n = 9/33), and 21.21% with no proven CIN (n = 7/33).
HPV genotype prevalence and concordance
The use of a FVU collection device (Colli-Pee®) resulted in a median collection volume of 19 ml FVU (IQR: 18–19 ml), collected within a median time span of 1 h and 56 min (IQR: 1:23–2:50) after the previous urination. Samples were frozen in aliquots after the addition of a DNA preservative (UCM) within a median time span of 12 min (IQR: 0:11–0:16) after urination. No invalid hDNA test results (β-globin negative) were reported in the 110 included CS, nor in FVU after in-house ultrafiltration and DNA extraction.
The results of the Riatol assay in paired FVU and CS demonstrated an HPV prevalence of 80.00 (n = 88/110) and 75.45% (n = 83/110) in FVU and CS, respectively, with a good κ-agreement of 0.660 (95% CI: 0.486–0.833). The same pattern was observed for HPV16/18 and HR-HPV DNA, with a prevalence of 25.45 and 69.09% in FVU, and 23.64 and 66.36% in CS, respectively. A very good and good agreement for HPV16 and/or 18 (κ: 0.902; 95% CI: 0.807–0.996) and HR-HPV DNA (κ: 0.688; 95% CI: 0.542–0.835) between paired samples was observed, with a McNemar OR of 3.000 (95% CI: 0.241–157.492; FDR-adjusted p = 0.822) (ntotal = 110; n = 25 FVU+/CS+, n = 3 FVU+/CS-, n = 1 FVU-/CS+, n = 81 FVU-/CS-) and 1.500 (95% CI: 0.477–5.121; FDR-adjusted p = 0.822) (ntotal = 110; n = 67 FVU+/CS+, n = 9 FVU+/CS-, n = 6 FVU-/CS+, n = 28 FVU-/CS-), respectively (Online Resource 1). HPV31 (FVU) and HPV16 and 31 (CS) were observed to be most prevalent in our referral population, followed by HPV16 and 68 for FVU, and HPV51 and 52 for CS (Fig. 2).
Prevalence of HPV genotypes according to sample type. The sum of cervical (CS; blue bars) and first-void urine samples (FVU; green bars) observed as positive for HPV are separately displayed on the y-axis for each genotype (x-axis). Ranking of HPV genotypes was performed according to the combined number of CS and FVU samples that tested positive
Overall, a (very) good agreement was observed at the genotype level, except for HPV33/39/67 and 6, where moderate and fair κ-agreements were observed, respectively (Fig. 3). The observed odds of having a positive result for a single infection for FVU versus CS was 0.263 (95% CI: 0.077–0.729, FDR-adjusted p = 0.041) (CS: n = 45/92; FVU: n = 31/92). In contrast, the observed odds of having a positive result for FVU versus CS was 7-fold higher in the case of multiple infections (McNemar OR: 7.333, 95% CI: 2.203–38.269, FDR-adjusted p = 0.004) (CS: n = 38/92; FVU: n = 57/92) (Online Resource 1), with a maximum of five types simultaneously detected in CS as opposed to eight in FVU.
HPV genotype distribution and agreement of paired cervical (CS) and first-void urine samples (FVU). The number of samples that tested positive in both FVU and CS are indicated by turquoise bars. Discordant samples for each genotype are separately indicated by blue (CS only) and green (FVU only) bars. aThe Cohen’s Kappa (κ) was judged as follows: κ ≤ 0.20, poor; 0.21 ≤ κ ≤ 0.40, fair; 0.41 ≤ κ ≤ 0.60, moderate; 0.61 ≤ κ ≤ 0.80, good; and κ ≥ 0.81, very good agreement [48]. 95% CI 95% confidence interval, NV Due to the zero cell count in the discordant pairs for HPV11, κ was not calculated
HPV copy number agreement
For all 110 paired samples, β-globin was amplified to determine the amount of hDNA per µl of DNA extract. The median hDNA concentration in FVU and CS was 14.68 (IQR: 6.57–31.08) and 67.79 (IQR: 32.53–117.63) ng per µl of DNA extract, respectively. On the log scale, we detected 0.67 log more of hDNA in CS (1.83 ± 0.04 SE (standard error)) compared to FVU (1.16 ± 0.05 SE) on average. No linear correlation (Pearson) was observed between log hDNA and age for CS (0.043, FDR-adjusted p = 0.654) nor FVU (−0.126, FDR-adjusted p = 0.382).
Significant positive Spearman rank correlations (rs) in HPV copies per µl of DNA extract between paired samples were observed for HPV16 (rs = 0.670; FDR-adjusted p = 0.006), HPV18 (rs = 0.893; FDR-adjusted p = 0.031), HPV31 (rs = 0.527; FDR-adjusted p = 0.031), HPV53 (rs = 0.691; FDR-adjusted p = 0.017), and HPV68 (rs = 0.569; FDR-adjusted p = 0.031) (Online Resource 2). Correlations for the two most carcinogenic HPV types (HPV16 and 18) are illustrated in Online Resource 3.
No significant Spearman’s rank correlations were observed between HPV copies per µl of DNA extract (for each individual genotype), and the number of cells present in either CS or FVU. For comparison, the log transformed HPV copies per µl of DNA extract and per hDNA equivalent for each individual genotype are represented in Fig. 4 (absolute numbers and statistics are detailed in Online Resource 3). A higher median log HPV copy number was observed in 12 out of 13 and 11 out of 13 (probable) HR-HPV genotypes in CS versus FVU samples reported in HPV copies per µl of DNA extract and per hDNA equivalent, respectively. These differences were only significant for HPV16 and 68, for which a 1.134 (FDR-adjusted p = 0.040) and 1.017 log (FDR-adjusted p = 0.040) increase in the median copy number per µl of DNA extract was observed in CS versus FVU, respectively.
Distribution of log transformed HPV copies in paired cervical (CS) and first-void urine samples (FVU). The log transformed HPV copies per (A) microliter of DNA extract and (B) per hDNA equivalent in CS (blue bars) and FVU (green bars) are displayed on the y-axis for each genotype (x-axis). Significantly different median log HPV copies between paired samples are indicated by an asterisk (Wilcoxon matched pairs signed rank test), when p-values adjusted for multiple testing using the false discovery rate (FDR) were smaller than 0.05
Acceptability of first-void urine sampling
Acceptability data were gathered through questionnaires completed by 124 eligible women after providing a Colli-Pee®-collected FVU sample. The majority of the participants favored FVU sampling (n = 83/113; 73.45%) over a clinician-collected sample (n = 24/113; 21.24%). Five out of 83 women preferred the Colli-Pee® method if it were as reliable as a smear collected by a doctor/gynecologist. One woman only preferred this method if it could be performed at home. Another woman brought up the issue that no questions could be asked to the doctor/gynecologist. Although ‘no preference’ was not an option in the questionnaire, five out of 113 women (4.42%) wrote down that they did not have a preference between the two methods or checked both boxes. One woman (n = 1/113; 0.88%) preferred yearly FVU collection with the Colli-Pee® and bi-yearly smear collection by the doctor/gynecologist. In addition, from the data that was collected, FVU collection at home was preferred over collection at the clinic or the general practitioner’s office. This was demonstrated by 115 out of 122 (94.26%) and 81 out of 120 (67.50%) of women agreeing that FVU sampling was a good method to perform at home versus at the clinic or the general practitioner’s office, respectively (Online Resource 5).
Discussion
Several studies have explored the use of urine sampling as a useful and non-invasive alternative for HPV detection for screening purposes [18,19,20,21,22,23,24,25,26,27,28, 49,50,51,52], and to reach screening non-attendees via home-based self-sampling [14]. However, these results are not conclusive due to a number of variables that could negatively affect HPV detection in urine. In this study, we investigated the usefulness of FVU as a specimen for the detection of HPV DNA among women referred for colposcopy using an optimized sample collection and processing protocol and the results obtained from CS as references.
Key notes for improved human and HPV DNA detection in urine have been studied [16, 17, 21, 25, 26, 30, 31] and were recently summarized [6]. Briefly, optimized urinary HPV DNA detection should include: (i) use of FVU; (ii) prevention of human/HPV DNA degradation during extraction and storage by adding a preservative; (iii) processing of a sufficient volume of whole urine; and the (iv) use of an analytically sensitive HPV test. In this study, FVU samples were collected prior to the clinical exam using a FVU collection device to ensure the collection of a standardized FVU volume (19 ml; IQR: 18–19 ml). In addition, women were asked to not extensively wash their genitals and to not urinate at least 1 h prior to sample collection. The suitability of the optimized techniques used, namely, ultrafiltration and automated extraction of DNA from preserved, unfractionated FVU samples [21, 31], was confirmed by the presence of hDNA in all FVU samples. This was in contrast to other studies in which invalid test results were reported [14, 24, 38]. The validity of hDNA as indicator for proper sample storage, processing, and detection of HPV DNA has been questioned [31] and was discussed in a previous study [22]. Still, samples testing negative for hDNA might point towards suboptimal collection, storage, and (pre-)analytical processing protocols. In addition, the HPV test used is a highly sensitive qPCR-based assay employed by the Belgian HPV reference laboratory.
This study provided evidence of a good HR-HPV agreement between paired FVU and CS (κ = 0.688; 95% CI: 0.542–0.835). Furthermore, very good agreement was observed for HPV16, 18, and 31, with no significant difference in the observed odds of FVU and CS positive for the abovementioned genotypes, nor for HR-HPV. Where others reported a lower HR-HPV prevalence in urine samples compared to cervical specimens [38], we observed an HR-HPV prevalence of 69 (n = 76/110) and 66% (n = 73/110) in FVU and CS, respectively. These results are in line with studies where optimized collection and pre-analytical processing protocols were applied [19, 20, 22, 31, 50]. Previous observations made in a similar study performed by Bissett and colleagues (2011) [38], who collected 253 paired urine and CS from women referred to colposcopy, reported an HR-HPV prevalence of 70 and 81%, respectively. The somewhat lower HR-HPV prevalence observed in our study could be because our study population consisted of a greater number of women diagnosed with normal cytological findings. In a screening setting, a lower median age of the women could result in a higher HR-HPV prevalence [14, 23]. However, no decreasing trend of HR-HPV prevalence with increasing age was observed in our referral population. Consistent with Belgian data, in which HPV16 and 31 are ranked as two out of three most prevalent genotypes in women with normal, low- and high-grade abnormal cytology [53] and invasive CxCa [54, 55], both HPV16 and 31 (CS) and HPV31 (FVU) were the most prevalent genotypes observed in our study population. These results are in agreement with previous observations made in a referral population [38]. Furthermore, we observed that in samples positive for any HPV genotype in at least one of the paired samples, more single-type infections were observed in CS, whereas multiple-type infections were more frequent in FVU. In the CapU study, a large proportion of multiple urinary infections (44.80%) was observed as well [14]. The discrepancy in the HPV results in our cohort was primarily evident in HPV genotypes classified as probable and possible high-risk. These results may suggest that FVU might sample next to cervical, also more infections originating from the vagina and vulva.
The HPV viral load in CS is typically defined as the number of HPV copies per cell, herein referred to as the hDNA equivalent. As similarly reported by Payan and colleagues [24], no significant correlation was observed in our study between HPV copies per µl of DNA extract and the number of cells per sample. Additionally, no difference can be made between HPV-infected and non-infected cells. Because we were interested in detecting the total amount of HPV DNA (cell-free and -associated) in FVU per sample volume, and since HPV DNA in urine originates from mucus and debris from exfoliated cervical cells, unlike clinician-collected samples, where cervical cells are scraped off the cervix, we did not normalize HPV copy number according to sample cellularity. This enabled comparison of the FVU and cervical HPV DNA results. However, this calculation does not take stratification according to sample cellularity during DNA extraction into account [22], which is performed on CS prior to the Riatol assay [42]. Thus, HPV copies are reported per µl of DNA extract, and not per volume of initial sample collected. Furthermore, no significant difference in the median HPV copy number (per µl of DNA extract) was observed between paired samples, except for HPV16 and 68. The trend towards good agreement between FVU and CS for HPV DNA (per µl of DNA extract) was also observed by the significantly positive correlations observed between paired samples for HPV16, 18, 31, 53, and 68.
Lastly, the results obtained from the questionnaires confirmed data from previous studies [15, 16] reporting that (first-void) urine collection is the most preferred sampling method for CxCa screening by women with respect to vaginal/cervical self-sampling and clinician collected samples. We observed that FVU collection using a FVU collection device (Colli-Pee®) was preferred over a clinician-collected CS (n = 83/113 (73%) favored FVU sampling). The acceptability of FVU sampling was also described by Leeman and colleagues, comparing the preference of a clinician-collected CS, vaginal self-sample (Evalyn brush™, Rovers Medical Devices, the Netherlands), and FVU sample (Colli-Pee®) in 91 women providing all three samples, with an overall rating of 7.6, 8.1, and 8.6 out of 10, respectively [17]. Notably, FVU collection at home was preferred over collection at the clinic or the general practitioner’s office. This is in agreement with 87% of women (referral population) who reported being comfortable receiving a urine collection package at home in a study by Senkomago and colleagues (2016) [16]. Together with results from the CapU study, in which home-based urine sampling increased the participation rate by 11–16% in screening non-responders (40–65 years) after receiving two reminders [14], these data indicate that FVU sampling shows potential as liquid biopsy source to reach (non-attending) women for home-based CxCa screening. Nevertheless, it remains to be investigated how home-based FVU sampling can be ideally implemented in practice, since in contrast to the positive outcomes obtained in the studies mentioned above, a lack of privacy at home, education, place of residence (urban versus rural), and women’s concerns about collecting the self-sample properly themselves could influence the acceptability of self-sampling [56]. The use of urine sampling to monitor the impact of HPV-vaccination has also been reported, focusing on urine as a sample to assess viral endpoints [20, 57, 58]. The World Health Organization and International Agency for Research on Cancer have already reported on a vaccine-impact study using viral endpoints in FVU in approximately 2,000 young women [20], demonstrating that FVU is a well-accepted liquid biopsy source that can be easily and non-invasively collected in large-scale studies.
Limitations of our study need to be acknowledged, most notably the relatively small sample size. As our study was not designed to investigate HPV copy number trend and lesion severity, or to compare the association of FVU and CS for individual HPV-genotypes, one should be cautious with interpreting the results. The acceptability results should be interpreted with caution, as several women wrote down that they had no preference between the two methods, while the option ‘no preference’ was not given in the questionnaire. As this could bias our results, we choose to descriptively report the acceptability data obtained in this study. In addition, despite the heterogeneous character of our study population (including women redirected to colposcopy for the first time, or women who had been followed-up for a long time, whether after treatment or not), participating women were well-characterized. The absence of a home-based setting, which is the purpose of using this liquid biopsy method [6], will be assessed in an adjoining study. As this was a pilot study to investigate the presence of biomarkers in FVU, including HPV DNA (copy number) and to develop analytical protocols, no preservation buffer was prefilled in the collector vials to avoid incompatibilities with other assays under research. Still, samples were immediately placed on ice after collection and stored with preservation buffer within a median time span of 12 min (IQR: 0:11–0:16) to reduce the loss of human and HPV DNA to a minimum. At last, a higher disease prevalence in referral populations might benefit from an accurate measure of sensitivity at the cost of less reliable specificity measures.
In conclusion, in this study, we observed that, when appropriately sampled, stored, and processed, testing FVU for (HR-) HPV DNA ensured a good agreement with CS in a Belgian referral population. At the genotype level, significant positive correlations were observed between paired samples for the three most carcinogenic HPV types in our country, HPV16, 18, and 31, as well as for HPV53 and 68. The median copy number observed in paired samples did not differ except for HPV16 and 68. Furthermore, FVU sampling is highly preferred, non-invasive, and can be performed at home. This method is particularly interesting as a screening tool to overcome the hurdle of screening among non-responders. However, further research is imperative to standardize the procedures involved in HPV DNA detection in FVU and to evaluate its clinical performance in large population-based studies.
References
GLOBOCAN (2012) Cervical cancer: estimated incidence, mortality and prevalence worldwide in 2012. http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx. Accessed 1 Sept 2017
Van Damme P, Bonanni P, Bosch FX, Joura E, Kjaer SK, Meijer CJ, Petry KU, Soubeyrand B, Verstraeten T, Stanley M (2016) Use of the nonavalent HPV vaccine in individuals previously fully or partially vaccinated with bivalent or quadrivalent HPV vaccines. Vaccine 34(6):757–761. https://doi.org/10.1016/j.vaccine.2015.12.063
Kreimer AR, Struyf F, Del Rosario-Raymundo MR, Hildesheim A, Skinner SR, Wacholder S, Garland SM, Herrero R, David MP, Wheeler CM, Costa Rica Vaccine Trial Study Group A, Gonzalez P, Jimenez S, Lowy DR, Pinto LA, Porras C, Rodriguez AC, Safaeian M, Schiffman M, Schiller JT, Schussler J, Sherman ME, Authors PSG, Bosch FX, Castellsague X, Chatterjee A, Chow SN, Descamps D, Diaz-Mitoma F, Dubin G, Germar MJ, Harper DM, Lewis DJ, Limson G, Naud P, Peters K, Poppe WA, Ramjattan B, Romanowski B, Salmeron J, Schwarz TF, Teixeira JC, Tjalma WA, Collaborators HPPIC-PI, Group GSKVCSS (2015) Efficacy of fewer than three doses of an HPV-16/18 AS04-adjuvanted vaccine: combined analysis of data from the Costa Rica vaccine and PATRICIA trials. Lancet Oncol 16(7):775–786. https://doi.org/10.1016/S1470-2045(15)00047-9
Arbyn M, Ronco G, Anttila A, Meijer CJLM, Poljak M, Ogilvie G, Koliopoulos G, Naucler P, Sankaranarayanan R, Peto J (2012) Evidence regarding human papillomavirus testing in secondary prevention of cervical cancer. Vaccine 30:F88–F99. https://doi.org/10.1016/j.vaccine.2012.06.095
Ronco G, Dillner J, Elfstrom KM, Tunesi S, Snijders PJ, Arbyn M, Kitchener H, Segnan N, Gilham C, Giorgi-Rossi P, Berkhof J, Peto J, Meijer CJ, International HPVswg (2014) Efficacy of HPV-based screening for prevention of invasive cervical cancer: follow-up of four European randomised controlled trials. Lancet 383(9916):524–532. https://doi.org/10.1016/S0140-6736(13)62218-7
Van Keer S, Pattyn J, Tjalma WAA, Van Ostade X, Ieven M, Van Damme P, Vorsters A (2017) First-void urine: a potential biomarker source for triage of high-risk human papillomavirus infected women. Eur J Obstet Gynecol Reprod Biol 216:1–11. https://doi.org/10.1016/j.ejogrb.2017.06.036
Waller J, Bartoszek M, Marlow L, Wardle J (2009) Barriers to cervical cancer screening attendance in England: a population-based survey. J Med Screen 16(4):199–204. https://doi.org/10.1258/jms.2009.009073
Arrossi S, Ramos S, Straw C, Thouyaret L, Orellana L (2016) HPV testing: a mixed-method approach to understand why women prefer self-collection in a middle-income country. BMC Public Health 16:832. https://doi.org/10.1186/s12889-016-3474-2
Arbyn M, Verdoodt F, Snijders PJ, Verhoef VM, Suonio E, Dillner L, Minozzi S, Bellisario C, Banzi R, Zhao FH, Hillemanns P, Anttila A (2014) Accuracy of human papillomavirus testing on self-collected versus clinician-collected samples: a meta-analysis. Lancet Oncol 15(2):172–183. https://doi.org/10.1016/S1470-2045(13)70570-9
von Karsa L, Arbyn M, De Vuyst H, Dillner J, Dillner L, Franceschi S, Patnick J, Ronco G, Segnan N, Suonio E, Törnberg S, Anttila A (2015) European guidelines for quality assurance in cervical cancer screening. Summary of the supplements on HPV screening and vaccination. Papillomavirus Res 1:22–31. https://doi.org/10.1016/j.pvr.2015.06.006
Tamalet C, Le Retraite L, Leandri FX, Heid P, Sancho Garnier H, Piana L (2013) Vaginal self-sampling is an adequate means of screening HR-HPV types in women not participating in regular cervical cancer screening. Clin Microbiol Infect: Off Publ Eur Soc Clin Microbiol Infect Dis 19(1):E44–E50. https://doi.org/10.1111/1469-0691.12063
Racey CS, Withrow DR, Gesink D (2013) Self-collected HPV testing improves participation in cervical cancer screening: a systematic review and meta-analysis. Can J Publ Health Rev Can Sante Publique 104(2):e159–e166
Verdoodt F, Jentschke M, Hillemanns P, Racey CS, Snijders PJ, Arbyn M (2015) Reaching women who do not participate in the regular cervical cancer screening programme by offering self-sampling kits: a systematic review and meta-analysis of randomised trials. Eur J Cancer 51(16):2375–2385. https://doi.org/10.1016/j.ejca.2015.07.006
Ducancelle A, Reiser J, Pivert A, Le Guillou-Guillemette H, Le Duc-Banaszuk AS, Lunel-Fabiani F (2015) Home-based urinary HPV DNA testing in women who do not attend cervical cancer screening clinics. J Infect 71(3):377–384. https://doi.org/10.1016/j.jinf.2015.05.001
Sellors JW, Lorincz AT, Mahony JB, Mielzynska I, Lytwyn A, Roth P, Howard M, Chong S, Daya D, Chapman W, Chernesky M (2000) Comparison of self-collected vaginal, vulvar and urine samples with physician-collected cervical samples for human papillomavirus testing to detect high-grade squamous intraepithelial lesions. CMAJ 163(5):513–518
Senkomago V, Des Marais AC, Rahangdale L, Vibat CR, Erlander MG, Smith JS (2016) Comparison of urine specimen collection times and testing fractions for the detection of high-risk human papillomavirus and high-grade cervical precancer. J Clin Virol 74:26–31. https://doi.org/10.1016/j.jcv.2015.11.005
Leeman A, Del Pino M, Molijn A, Rodriguez A, Torne A, de Koning M, Ordi J, van Kemenade F, Jenkins D, Quint W (2017) HPV testing in first-void urine provides sensitivity for CIN2+ detection comparable to a physician-taken smear or brush-based self-sample: cross-sectional data from a triage population. BJOG: Int J Obstet Gynaecol 124(9):1356–1363. https://doi.org/10.1111/1471-0528.14682
Burroni E, Bonanni P, Sani C, Lastrucci V, Carozzi F, Hpv ScreeVacc Working G, Iossa A, Andersson KL, Brandigi L, Di Pierro C, Confortini M, Levi M, Boccalini S, Indiani L, Sala A, Tanini T, Bechini A, Azzari C (2015) Human papillomavirus prevalence in paired urine and cervical samples in women invited for cervical cancer screening. J Med Virol 87(3):508–515. https://doi.org/10.1002/jmv.24085
Combita AL, Gheit T, Gonzalez P, Puerto D, Murillo RH, Montoya L, Vorsters A, Van Keer S, Van Damme P, Tommasino M, Hernandez-Suarez G, Sanchez L, Herrero R, Wiesner C (2016) Comparison between urine and cervical samples for HPV DNA detection and typing in young women in Colombia. Cancer Prev Res (Phila) 9(9):766–771. https://doi.org/10.1158/1940-6207.CAPR-16-0038
Franceschi S, Chantal Umulisa M, Tshomo U, Gheit T, Baussano I, Tenet V, Tshokey T, Gatera M, Ngabo F, Van Damme P, Snijders PJ, Tommasino M, Vorsters A, Clifford GM (2016) Urine testing to monitor the impact of HPV vaccination in Bhutan and Rwanda. Int J Cancer 139(3):518–526. https://doi.org/10.1002/ijc.30092
Vorsters A, Micalessi I, Bilcke J, Ieven M, Bogers J, Van Damme P (2012) Detection of human papillomavirus DNA in urine. A review of the literature. Eur J Clin Microbiol Infect Dis 31(5):627–640. https://doi.org/10.1007/s10096-011-1358-z
Vorsters A, Van Keer S, Biesmans S, Hens A, De Coster I, Goossens H, Ieven M, Van Damme P (2016) Long-term follow-up of HPV infection using urine and cervical quantitative HPV DNA testing. Int J Mol Sci 17(5). https://doi.org/10.3390/ijms17050750
Ducancelle A, Legrand MC, Pivert A, Veillon P, Le Guillou-Guillemette H, De Brux MA, Beby-Defaux A, Agius G, Hantz S, Alain S, Catala L, Descamps P, Postec E, Caly H, Charles-Petillon F, Labrousse F, Lunel F, Payan C (2014) Interest of human papillomavirus DNA quantification and genotyping in paired cervical and urine samples to detect cervical lesions. Arch Gynecol Obstet 290(2):299–308. https://doi.org/10.1007/s00404-014-3191-y
Payan C, Ducancelle A, Aboubaker MH, Caer J, Tapia M, Chauvin A, Peyronnet D, Le Hen E, Arab Z, Legrand MC, Tran A, Postec E, Tourmen F, Avenel M, Malbois C, De Brux MA, Descamps P, Lunel F (2007) Human papillomavirus quantification in urine and cervical samples by using the Mx4000 and LightCycler general real-time PCR systems. J Clin Microbiol 45(3):897–901. https://doi.org/10.1128/JCM.02022-06
Pathak N, Dodds J, Zamora J, Khan K (2014) Accuracy of urinary human papillomavirus testing for presence of cervical HPV: systematic review and meta-analysis. BMJ 349:g5264. https://doi.org/10.1136/bmj.g5264
Enerly E, Olofsson C, Nygard M (2013) Monitoring human papillomavirus prevalence in urine samples: a review. Clin Epidemiol 5:67–79. https://doi.org/10.2147/CLEP.S39799
Hagihara M, Yamagishi Y, Izumi K, Miyazaki N, Suzuki T, Kato H, Nishiyama N, Koizumi Y, Suematsu H, Mikamo H (2016) Comparison of initial stream urine samples and cervical samples for detection of human papillomavirus. J Infect Chemother: Off J Jpn Soc Chemother 22(8):559–562. https://doi.org/10.1016/j.jiac.2016.05.009
Sahasrabuddhe VV, Gravitt PE, Dunn ST, Brown D, Allen RA, Eby YJ, Smith K, Zuna RE, Zhang RR, Gold MA, Schiffman M, Walker JL, Castle PE, Wentzensen N (2014) Comparison of human papillomavirus detections in urine, vulvar, and cervical samples from women attending a colposcopy clinic. J Clin Microbiol 52(1):187–192. https://doi.org/10.1128/jcm.01623-13
Vorsters A, Van Damme P, Clifford G (2014) Urine testing for HPV: rationale for using first void. BMJ 349:g6252. https://doi.org/10.1136/bmj.g6252
Smith JS, Smith JB, Faherty BR, Isaacson SC, Des Marais AC, Fakner A, Rahangdale L, Vaughan LM (2017) Effect of urine preservative on HPV testing results among urine samples. In: HPV2017, Cape Town, South Africa
Vorsters A, Van den Bergh J, Micalessi I, Biesmans S, Bogers J, Hens A, De Coster I, Ieven M, Van Damme P (2014) Optimization of HPV DNA detection in urine by improving collection, storage, and extraction. Eur J Clin Microbiol Infect Dis 33(11):2005–2014. https://doi.org/10.1007/s10096-014-2147-2
Schmitt M, Depuydt C, Benoy I, Bogers J, Antoine J, Arbyn M, Pawlita M, Group VS (2013) Multiple human papillomavirus infections with high viral loads are associated with cervical lesions but do not differentiate grades of cervical abnormalities. J Clin Microbiol 51(5):1458–1464. https://doi.org/10.1128/JCM.00087-13
Wu Z, Qin Y, Yu L, Lin C, Wang H, Cui J, Liu B, Liao Y, Warren D, Zhang X, Chen W (2017) Association between human papillomavirus (HPV) 16, HPV18, and other HR-HPV viral load and the histological classification of cervical lesions: results from a large-scale cross-sectional study. J Med Virol 89(3):535–541. https://doi.org/10.1002/jmv.24645
Carcopino X, Henry M, Mancini J, Giusiano S, Boubli L, Olive D, Tamalet C (2012) Significance of HPV 16 and 18 viral load quantitation in women referred for colposcopy. J Med Virol 84(2):306–313. https://doi.org/10.1002/jmv.23190
Marongiu L, Godi A, Parry JV, Beddows S (2014) Human papillomavirus 16, 18, 31 and 45 viral load, integration and methylation status stratified by cervical disease stage. BMC Cancer 14:384. https://doi.org/10.1186/1471-2407-14-384
Depuydt CE, Jonckheere J, Berth M, Salembier GM, Vereecken AJ, Bogers JJ (2015) Serial type-specific human papillomavirus (HPV) load measurement allows differentiation between regressing cervical lesions and serial virion productive transient infections. Cancer Med 4(8):1294–1302. https://doi.org/10.1002/cam4.473
Depuydt CE, Criel AM, Benoy IH, Arbyn M, Vereecken AJ, Bogers JJ (2012) Changes in type-specific human papillomavirus load predict progression to cervical cancer. J Cell Mol Med 16(12):3096–3104. https://doi.org/10.1111/j.1582-4934.2012.01631.x
Bissett SL, Howell-Jones R, Swift C, De Silva N, Biscornet L, Parry JV, Saunders NA, Nathan M, Soldan K, Szarewski A, Cuzick J, Beddows S (2011) Human papillomavirus genotype detection and viral load in paired genital and urine samples from both females and males. J Med Virol 83(10):1744–1751. https://doi.org/10.1002/jmv.22167
Sehgal A, Gupta S, Parashari A, Sodhani P, Singh V (2009) Urine HPV-DNA detection for cervical cancer screening: prospects and prejudices. J Inst Obstet Gynaecol 29(7):583–589. https://doi.org/10.1080/01443610903061736
IARC (2016) Agents classified by the IARC Monographs. vol 1–120. http://monographs.iarc.fr/ENG/Classification/latest_classif.php. Accessed 27 Oct. 2017
Depuydt CE, Thys S, Beert J, Jonckheere J, Salembier G, Bogers JJ (2016) Linear viral load increase of a single HPV-type in women with multiple HPV infections predicts progression to cervical cancer. Int J Cancer 139(9):2021–2032. https://doi.org/10.1002/ijc.30238
Micalessi IM, Boulet GAV, Bogers JJ, Benoy IH, Depuydt CE (2012) High-throughput detection, genotyping and quantification of the human papillomavirus using real-time PCR. Clin Chem Lab Med 50(4):655–661. https://doi.org/10.1515/Cclm.2011.835
Depuydt CE, Benoy IH, Beert JF, Criel AM, Bogers JJ, Arbyn M (2012) Clinical validation of a type-specific real-time quantitative human papillomavirus PCR against the performance of hybrid capture 2 for the purpose of cervical cancer screening. J Clin Microbiol 50(12):4073–4077. https://doi.org/10.1128/JCM.01231-12
Pattyn J, Dekoeijer, Van Keer S, Biesmans S, Ieven M, Beyers K, Vankerckhoven V, Van Damme P, Vorsters A (2017) HPV DNA detection in urine: effect of a first-void urine collection device and timing of collection. In: HPV2017, Cape Town, South Africa
Greenland S (2000) Small-sample bias and corrections for conditional maximum-likelihood odds-ratio estimators. Biostatistics 1(1):113–122. https://doi.org/10.1093/biostatistics/1.1.113
Klaus B, Strimmer K (2015) fdrtool: estimation of (local) false discovery rates and higher criticism. R package version 1.2.15. http://CRAN.R-project.org/package=fdrtool
Team RC (2017) R: A Language and Environment for Statistical Computing. https://www.r-project.org/
Altman DG (1991) Practical statistics for medical research. Chapman and Hall/CRC
Stanczuk G, Baxter G, Currie H, Lawrence J, Cuschieri K, Wilson A, Arbyn M (2016) Clinical validation of hrHPV testing on vaginal and urine self-samples in primary cervical screening (cross-sectional results from the papillomavirus Dumfries and Galloway-PaVDaG study). BMJ Open 6(4):e010660. https://doi.org/10.1136/bmjopen-2015-010660
Tshomo U, Franceschi S, Tshokey T, Tobgay T, Baussano I, Tenet V, Snijders PJ, Gheit T, Tommasino M, Vorsters A, Clifford GM (2017) Evaluation of the performance of human papillomavirus testing in paired urine and clinician-collected cervical samples among women aged over 30 years in Bhutan. Virol J 14(1):74. https://doi.org/10.1186/s12985-017-0744-2
Cuzick J, Cadman L, Ahmad AS, Ho L, Terry G, Kleeman M, Lyons D, Austin J, Stoler MH, Vibat CRT, Dockter J, Robbins D, Billings PR, Erlander MG (2017) Performance and diagnostic accuracy of a urine-based human papillomavirus assay in a referral population. Cancer Epidemiol Biomark Prev: Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol 26(7):1053–1059. https://doi.org/10.1158/1055-9965.EPI-16-0960
D’Hauwers KW, Tjalma WA (2009) Screening for human papillomavirus: is urine useful? Indian J Cancer 46(3):190–193. https://doi.org/10.4103/0019-509x.52952
ICO (2017) Human papillomavirus and related disease report. http://www.hpvcentre.net/statistics/reports/XWX.pdf. Accessed 1 Sept 2017
Tjalma WA, Trinh XB, Rosenlund M, Makar AP, Kridelka F, Rosillon D, Van Dam PA, Collas De Souza S, Holl K, Simon P, Jenkins D (2015) A cross-sectional, multicentre, epidemiological study on human papillomavirus (HPV) type distribution in adult women diagnosed with invasive cervical cancer in Belgium. Facts Views Vis Obgyn 7(2):101–108
Tjalma WA, Fiander A, Reich O, Powell N, Nowakowski AM, Kirschner B, Koiss R, O’Leary J, Joura EA, Rosenlund M, Colau B, Schledermann D, Kukk K, Damaskou V, Repanti M, Vladareanu R, Kolomiets L, Savicheva A, Shipitsyna E, Ordi J, Molijn A, Quint W, Raillard A, Rosillon D, De Souza SC, Jenkins D, Holl K (2013) Differences in human papillomavirus type distribution in high-grade cervical intraepithelial neoplasia and invasive cervical cancer in Europe. Int J Cancer 132(4):854–867. https://doi.org/10.1002/ijc.27713
Chamot E, Mulambia C, Kapambwe S, Shrestha S, Parham GP, Macwan’gi M, Mwanahamuntu MH (2015) Preference for human papillomavirus-based cervical cancer screening: results of a choice-based conjoint study in Zambia. J Low Genit Tract Dis 19(2):119–123. https://doi.org/10.1097/LGT.0000000000000081
Vorsters A, Van Keer S, Van Damme P (2015) The use of urine in the follow-up of HPV vaccine trials. Hum Vacc Immunother 11(2):350–352. https://doi.org/10.4161/21645515.2014.995058
Cuschieri K, Nandwani R, McGough P, Cook F, Hogg L, Robertson C, Cubie H (2011) Urine testing as a surveillance tool to monitor the impact of HPV immunization programs. J Med Virol 83(11):1983–1987. https://doi.org/10.1002/jmv.22183
Acknowledgements
We would like to express our gratitude to all women who volunteered to participate in this study, and thank Dr. L. Ameryckx for her assistance in recruiting participants. We are grateful for the statistical support of N. Hens.
Funding
This study was funded by the Industrial Research Fund of the University of Antwerp, Belgium (PS ID 32387), and S. Van Keer is supported by a Ph.D. fellowship of the Research Foundation – Flanders (FWO), Belgium (1120816 N).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
P. Van Damme and A. Vorsters are co-founders of Novosanis (Belgium), a spin-off company of the University of Antwerp. All other authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (UZA/University of Antwerp, Belgium (B300201525585)) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
ESM 1
(DOCX 140 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Van Keer, S., Tjalma, W.A.A., Pattyn, J. et al. Human papillomavirus genotype and viral load agreement between paired first-void urine and clinician-collected cervical samples. Eur J Clin Microbiol Infect Dis 37, 859–869 (2018). https://doi.org/10.1007/s10096-017-3179-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-017-3179-1