Abstract
Hospital-acquired infections (HAIs) are a cause of continuously increasing morbidity and mortality. Most of these infections are caused by a limited set of bacterial species, which share the capability to efficiently spread from patient to patient and to easily acquire antibiotic resistance determinants. This renders correct and rapid species identification and antibiotic susceptibility testing (AST) important and underscores the relevance of bacterial epidemiological typing. The latter is needed for the sensitive detection and exact tracing of nosocomial spread of these potentially multidrug-resistant microorganisms (MDRO). Many microbial typing technologies have been developed and put to some level of executive practice, but it seems that the continued evolution in methodology has currently reached an apex: there is likely to be scientific and practical consensus on the ultimate typing potential of bacterial whole-genome sequencing (WGS). The possibility to perform pan-genomic nucleotide-to-nucleotide comparisons between strains belonging to a single species and to detect even minute changes in nucleotide order will identify closely related organisms, while upon accumulation of such mutations, independent descend can be assumed. Calibration of difference levels [i.e. number of single nucleotide polymorphisms (SNPs)] into categories of inter-strain relatedness needs to be performed in order to generate robust, portable typing schemes. Here, we will briefly discuss the state of affairs regarding bacterial epidemiology based upon WGS, its relatedness with the nomenclature of former typing approaches and the continuing need for a global typing language.
Similar content being viewed by others
Introduction
Hospital-acquired infections (HAIs) are infamous and widespread. A variety of microbial organisms can give rise to HAI and, with emerging and increasing antibiotic resistance among those nosocomial pathogens, the importance of HAI has been increasing steadily as well. HAI outbreaks are defined upon an increase in the frequency of hospital-acquired or healthcare facility-acquired cases of disease among patients or staff, over and above the expected base-line number of cases in a given setting. Healthcare facilities where HAI outbreaks can occur are hospitals, nursing homes, rehabilitation centres, (private) clinics, dialysis or cancer treatment centres, ambulatory surgery centres, physician offices, dental clinics, laboratories and any other facilities which provide healthcare or diagnostic services to individuals, whether public or privately owned [1]. To control HAI effectively, a combination of strategies must be used, including preventive measures such as education and environmental control, active surveillance of infection events, and recognition of and intervention into ongoing disease outbreaks (e.g. [2]). Molecular epidemiological investigations, critical to surveillance and intervention, rely on rapid and effective assessment of phenotypic and/or genetic relatedness among strains and help to distinguish outbreak situations from non-outbreak-related colonisation or infection events.
The impact and importance of HAI will continue to rise for the years to come and both detection of the HAI agents and their more detailed (clinical) epidemiological analyses need to be improved. Classical typing technologies need to be replaced by ones with improved reproducibility, data exchangeability and, most importantly, resolution. Only then will better tracing of HAIs, blocking their further spread and their elimination from the hospital eco-system, be feasible. Where, in the past, phenotyping was most important (from bacteriophage susceptibility testing, serological and antigen-based typing and more), over the past decades, different molecular typing methods have been developed. These ranged from plasmid characterisation, restriction enzyme analyses, various DNA amplification-mediated methods, multi-locus sequence typing (MLST) to the reigning gold standard technology for many species, pulsed-field gel electrophoresis (PFGE). Most recently, high-throughput next-generation nucleic acid sequencing was introduced, which initially focused on specific, pre-selected gene targets. To date, full microbial genome analysis by whole-genome sequencing (WGS) is even feasible and is, by many, considered to be the Holy Grail of typing. Many singular studies have already shown the feasibility of this approach [3, 4] and there are now even (commercial) service offers intended to provide extensive WGS characterisation of HAI isolates including direct typing for epidemiology purposes but also for the characterisation of antibiotic resistance and virulence factors [5, 6].
Here, we will describe the most important species involved in HAI, the gold standard typing technologies for their epidemiological typing and the perspective for fighting HAI caused by multidrug-resistant organisms (MDRO) with the newest generation of WGS-based methods. We exemplify several of these features using Clostridium difficile as a model organism.
Epidemiological context
Modern healthcare employs many types of invasive procedures and devices to treat (increasingly older and feeble) patients. Infections are often associated with the devices used in medical procedures, such as catheters or ventilators. These mostly HAIs include central line-associated bloodstream infections, catheter-associated, urinary tract infections, ventilator-associated pneumonia and several others. Infections may also occur at surgical sites (surgical site infections, SSIs) and the most common HAIs have been reviewed and discussed before [7]. The major HAIs include infections of the lung (22%), surgical sites (22%) and the gastro-intestinal system (13%).
In 2014, the results of a project known as the HAI Prevalence Survey were published. The survey described the burden of HAIs in US hospitals and reported that, in 2011, there were an estimated 722,000 HAIs occurring in US acute-care hospitals [8]. About 90,000 patients with HAIs died during hospitalisation. More than half of all HAIs occurred outside of the intensive care unit (ICU). This clearly shows the medical value of HAI, also on a global scale of course. Hence, HAI is a troublesome issue to the healthcare industry. The Centers for Disease Control and Prevention (CDC) estimates that 1 in 20 patients will contract an HAI each day and estimates suggest the economic burden of HAIs to soon reach $35.7 billion a year [9]. Costs are, in the major part, due to an extended hospital stay of around 17–18 days when an HAI is acquired. In the USA, close to 100.000 people die annually due to HAI (CDC general publication, 2009). The clinicians and organisations focused on hospital care quality are collaborating to improve infection control and reduce the number of patients whom contract HAI. However, outbreaks of HAI continue to occur.
Several studies show the distribution of pathogens involved in HAI. Depending on the country, the medical unit or the type of infection observed, several microorganisms are identified as major causative agents for HAIs. The more frequently detected outbreak-associated species are the following: Pseudomonas aeruginosa, Escherichia coli, Klebsiella pneumoniae, Clostridium difficile, Acinetobacter spp., Enterobacter spp., Enterococcus spp., Serratia marcescens, Staphylococcus aureus and several somewhat more minor species [1]. The majority of the problematic strains of these species have the capacity to quickly evolve (multiple) resistance to antibiotics. In this outbreak-associated, epidemiological context, cure of the infected is urgent, science should be translational and infection prevention is of utmost importance. New initiatives are in constant need.
Molecular bacterial typing methods
The goals of HAI outbreak investigation are to identify the pathogen that caused the outbreak, identify the source of the infection and, most importantly, control and prevent further spread of the infection. To establish the relatedness between strains, several molecular methods have been developed to calibrate and define genetic differences. Technologies have been optimised with respect to (minimal) costs, efficiency and discriminatory power. The more classical molecular methods most often used and cited for HAI are ribotyping, PFGE and MLST. In Table 1, mostly molecular methods of bacterial typing found in the scientific literature for the major species involved in HAI are summarised. The principles and (dis)advantages of a few frequently used and popular molecular typing methods, including WGS, will be briefly described below. Of course, there is a plethora of additional methods available and technical reviews have been published by many (e.g. [10,11,12]).
Ribotyping
The currently most popular format of ribotyping is based on polymerase chain reaction (PCR)-mediated detection of polymorphism in the 16S–23S intergenic spacer region [13]. Recently, it has been mostly used to investigate outbreaks due to C. difficile infection. However, this method generates bands of high and close molecular masses, which are difficult to separate by agarose gel electrophoresis. To improve the reading of banding patterns of PCR-ribotyping applied to C. difficile, partial sequencing of the rRNA genes (16S and 23S) and intergenic spacer region was performed, and then a new set of primers located closer to the intergenic spacer region has been defined [14]. The new PCR gave reproducible patterns of bands which were easier to separate by agarose gel electrophoresis. Two major kinds of PCR-based ribotyping exist: the PCR amplification followed by agarose gel electrophoresis and the ones followed by sequencer-based capillary separation. This typing method has evidenced major qualities such as ease of use, rapidity and reproducibility. A global reference library has been established and is available. Ribotyping is accurate and reproducible and the obtained data can be shared between laboratories [15].
Pulsed-field gel electrophoresis (PFGE)
Using this technique, the restriction pattern of the complete bacterial genome is visualised. Specific degradation of the bacterial chromosome is performed by infrequently cutting restriction enzymes. No mechanical damage occurs because of prior immobilisation of the DNA into agarose blocks. After enzymatic restriction, electrophoretic migration is performed in gel. PFGE is a highly discriminatory method: point mutations, deletions, insertions and loss or acquisition of plasmid might account for minor differences in profiles within a subtype or among epidemiologically related strains [16]. The PFGE method, however, is labourious and the results cannot be easily compared between laboratories, although the PulseNet project is proving the opposite of this statement [17]. Essentially, PFGE can be done for all bacterial species as long as the DNA is susceptible to restriction. However, it seems as if the technology is a bit on the return and likely to be replaced by sequencing-based technologies, even for the “big” public health applications.
Multi-locus sequence typing (MLST)
This method determines the genetic relatedness among strains by analysing the sequences of multiple genes that are compared for single nucleotide polymorphisms (SNPs) [18]. Since genes display varying degrees of genetic drift, housekeeping genes are most often sequenced because they are present in all isolates within a species and, genetically speaking, relatively stable. However, since they are under strong selective and functional pressure, their rate of genetic variability is relatively low and may not always provide adequate discrimination among unrelated isolates. For MLST, to be effective as an epidemiological tool, the selection of genes and their number needs to be adequate to distinguish among isolates which more recently diverged. For each of the genes sequenced, the allelic group including the isolate can be established as a sequence type (ST). A globally well-defined database allows scientists to register their strains and corresponding STs in the PubMLST database (https://pubMLST.org) hosted at the university of Oxford [19], where one can find the definition of even the most recently described STs.
Table 2 shows the housekeeping genes used to determine the ST of various bacterial species. For Acinetobacter baumannii, two MLST schemes have been described, one by Bartual et al. [20] in Oxford (UK) and the second by researchers from the Institute Pasteur (https://pubmlst.org/bigsdb?db=pubmlst_abaumannii_pasteur_seqdef). The two schemes do correlate well of course [21,22,23,24]. For Escherichia coli, even three schemes have been described, Pasteur’s (France) [25], Warwick’s [26] and the rarely used “st7” scheme [27]. Again, there is good correlation between the different nomenclatures despite the obvious use of different categorisation codes [28,29,30].
Although typing of C. difficile strains is usually done by ribotyping [31], more and more scientists use MLST for this species as well [32]. Correlation between ribotye (RT) and ST results is possible (Table 3). MLST is a highly discriminative method for typing microorganisms and has been applied successfully for the epidemiologic characterisation of a variety of clinically important bacterial pathogens. This method offers to the users near-perfect stability and transferability of data. As presented before, the pubMLST database allows for international sharing of the results and a worldwide distribution view of the strains by simply tracing their STs. The negative point is that the costs are high due to the need for DNA sequencing [34].
Major clones involved in HAI outbreaks
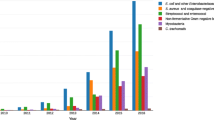
Bibliographic research was performed using targeted PubMed searches (September 2017) to better understand the involvement of bacterial species in HAI events and identify the ribotyping- and serotyping-defined major clones involved in local and more extensive outbreaks. In Table 4, we present both the most and least frequently reported STs and ribotypes involved in HAI and their worldwide geographic repartition on a per publication account. We included data from the German outbreaks database at http://www.outbreak-database.com (Institute for Medical Microbiology and Hospital Epidemiology, Medical School Hannover; Schülke & Mayr Company; Institute for Hygiene and Environmental Medicine, University Medicine of Berlin). This is an online database documenting outbreaks that took place in the healthcare setting and were published in the peer-reviewed scientific literature. This database currently contains 3536 outbreaks published from the years 1936 to 2016 with 305 different pathogens. No results are presented for Serratia marcescens and Enterobacter aerogenes (no formally accepted MLST scheme existing and limited numbers of outbreaks documented). Note that the data displayed in Table 4 have been calculated using numbers of publications assuming that this approximately equals the numbers of outbreak events. The table does not provide exact information on absolute numbers of bacterial strains but sketches a more relative global picture. For that reason, we also decided not to use the bibliographic data to depict historic timelines. The table does, however, underscore the fact that, if one uses a universal typing language, a global picture on the clonal dissemination of outbreak-related bacterial strains can be sketched. The use of such a language, which is feasible with ribotyping and serotyping, should be core to future developments using alternative technologies, including WGS.
Typing by WGS
WGS technology allows for the precise and rapid sequencing of the full genome of bacteria and defines, essentially, the ultimate global typing language using solely the four base characters: G, A, T and C. Different techniques are being continuously developed and refined by technology leaders in the sequencing market, including Illumina, PacBio, Oxford Nanopore and several others. For epidemiological investigation of potential outbreak situations, most clinicians and laboratory scientists combine clinical data related to the strains and the patient in combination with the results obtained by conventional typing methods. A combination of such data and high-resolution WGS has been shown to be valuable for fine-tuning the investigations into outbreaks for many, if not all, bacterial pathogens [3]. This technology is being transformed into an automated process and will offer truly accurate and reproducible digital data with very high discriminatory power. Data can be shared between laboratories and easily interpreted by software analysis. WGS analyses will bring ultimate information on genes, resistance markers, virulence factors and global genomic characteristics, including all types of mutations and detailed differences between the genomes of different but possibly very closely related strains within a microbial species [35]. To obtain this important information, the need for (bio-)informatics expertise is obvious, since there are many possible ways to extract comprehensive information from massive amounts of raw data. Quality filtration, assembly and many other steps allow the utilisation of sequenced genome. It would be beyond the scope of the present manuscript to survey all the published applications of WGS for analysis of the epidemiology of the HAI pathogens. However, we will perform a brief summary of the current state of affairs in this field for C. difficile, which presents an important and clinically highly relevant example.
After comparative technology papers [36], the first papers on the epidemiological tracing of C. difficile using WGS started appearing in 2013. Again, Eyre et al. [37] developed interpretational software not only for genomic comparison but also for the assessment of mixed infections. Mixed infections were reliably identified and new strain transmission events were documented. Data presented by the same group [38] showed that, besides patient-to-patient transmission, many nosocomial infections were due to as yet unidentified reservoirs. A little later, it was also shown that, using WGS, it was easier and more detailed to define overall genetic diversity [39,40,41] and to distinguish relapsing infection from re-infection [42]. Obviously, WGS allowed for the detection of circulating sub-clones and straightforward confirmation of ongoing, longitudinal, inter-institutional, sometimes geographically disperse C. difficile outbreaks [43,44,45,46,47]. Finally, Stoesser et al. [48] demonstrated that WGS may lead to the identification of new reservoirs (pets in this particular case), show overlap between different community-based reservoirs and that it adequately highlights colonisation events and transfer of strains.
Pathogenicity markers can be catalogued based on WGS as well [49] and C. difficile virulence is largely attributed to its toxins. However, upon the emergence of more virulent clones, WGS showed that additional factors may drive invasive potential as well. Quesada-Gómez et al. [50] demonstrated that a particularly virulent type harboured gyrA resistance mutations, 10% more predicted genes including phages and mobile genetic elements and a deletion in the tcdC gene. Assessing phenotypes based on genome sequences was investigated in a large study from the UK [51]. A combination of clinical, resistance and genomic data allowed to conclude that restriction of fluoroquinolone usage led to a decline in the regional incidence of certain clonal types of C. difficile. Confirmatory observations were published by Caspers et al. [52] while using alternative models. Data such as those presented in this manuscript should be used to fine-tune local and regional antibiotic stewardship.
The example of C. difficile WGS pinpoints the many added values that WGS has for more refined studies in the colonisation, infection, epidemiology and molecular characterisation of medically important bacterial pathogens. This technology will continue to have an increasing impact on clinical decision-making.
Conclusion
Classical typing technologies have led the way towards a universal typing language. Serotyping and ribotyping have been instrumental, although the language as such was still rather “primitive”. Even though it uses a four-letter alphabet only, whole-genome sequencing (WGS) has the clear capacity to develop a better and even more broadly accepted universal dialect. It has provided spectacular opportunities for the investigation of organisms causing hospital-acquired infections (HAIs) through resistance prevalence studies in combination with genomic epidemiology. Despite this progress, one has to realise that, for many clinicians and clinical microbiologists, such methods will remain out of reach for the decade to come. This provides us with the obligation to keep a close track between data generated using more classical technologies and those generated by WGS. In the end, only the close “linguistic” coordination of datasets will provide global insights into the international dissemination of pathogens of concern. Special attention should be given to those pathogens that carry multi-antibiotic resistance markers in order to bring non-treatable infections to a full stop.
References
Tabatabaei SM, Pour FB, Osmani S (2015) Epidemiology of hospital-acquired infections and related anti-microbial resistance patterns in a tertiary-care teaching hospital in Zahedan, Southeast Iran. Int J Infect 2:e29079
Dasgupta S, Das S, Chawan NS, Hazra A (2015) Nosocomial infections in the intensive care unit: incidence, risk factors, outcome and associated pathogens in a public tertiary teaching hospital of eastern India. Indian J Crit Care Med 19(1):14–20
Quainoo S, Coolen JPM, van Hijum SAFT, Huynen MA, Melchers WJG, van Schaik W, Wertheim HFL (2017) Whole-genome sequencing of bacterial pathogens: the future of nosocomial outbreak analysis. Clin Microbiol Rev 30(4):1015–1063
Le VTM, Diep BA (2013) Selected insights from application of whole genome sequencing for outbreak investigations. Curr Opin Crit Care 19(5):432–439
Dheda K, Gumbo T, Maartens G, Dooley KE, McNerney R, Murray M, Furin J, Nardell EA, London L, Lessem E, Theron G, van Helden P, Niemann S, Merker M, Dowdy D, Van Rie A, Siu GKH, Pasipanodya JG, Rodrigues C, Clark TG, Sirgel FA, Esmail A, Lin H-H, Atre SR, Schaaf HS, Chang KC, Lange C, Nahid P, Udwadia ZF, Horsburgh CR Jr, Churchyard GJ, Menzies D, Hesseling AC, Nuermberger E, McIlleron H, Fennelly KP, Goemaere E, Jaramillo E, Low M, Jara CM, Padayatchi N, Warren RM (2017) The epidemiology, pathogenesis, transmission, diagnosis, and management of multidrug-resistant, extensively drug-resistant, and incurable tuberculosis. Lancet Respir Med 5(4):291–360
Chalker VJ, Smith A, Al-Shahib A, Botchway S, Macdonald E, Daniel R, Phillips S, Platt S, Doumith M, Tewolde R, Coelho J, Jolley KA, Underwood A, McCarthy ND (2016) Integration of genomic and other epidemiologic data to investigate and control a cross-institutional outbreak of Streptococcus pyogenes. Emerg Infect Dis 22(6):973–980
Dabar G, Harmouche C, Salameh P, Jaber BL, Jamaleddine G, Waked M, Yazbeck P (2015) Community- and healthcare-associated infections in critically ill patients: a multicenter cohort study. Int J Infect Dis 37:80–85
Magill SS, Edwards JR, Bamberg W, Beldavs ZG, Dumyati G, Kainer MA, Lynfield R, Maloney M, McAllister-Hollod L, Nadle J, Ray SM, Thompson DL, Wilson LE, Fridkin SK (2014) Multistate point-prevalence survey of health care-associated infections. N Engl J Med 370(13):1198–1208
Zimlichman E, Henderson D, Tamir O, Franz C, Song P, Yamin CK, Keohane C, Denham CR, Bates DW (2013) Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med 173(22):2039–2046
Dunne MW Jr, Pouseele H, Monecke S, Ehricht R, van Belkum A (2017) Epidemiology of transmissible diseases: array hybridization and next generation sequencing as universal nucleic acid-mediated typing tools. Infect Genet Evol (in press). pii: S1567-1348(17)30324-6
Goering RV (2010) Pulsed field gel electrophoresis: a review of application and interpretation in the molecular epidemiology of infectious disease. Infect Genet Evol 10(7):866–875
Singh A, Goering RV, Simjee S, Foley SL, Zervos MJ (2006) Application of molecular techniques to the study of hospital infection. Clin Microbiol Rev 19(3):512–530
Gürtler V, Grando D (2013) New opportunities for improved ribotyping of C. difficile clinical isolates by exploring their genomes. J Microbiol Methods 93(3):257–272
Zhu S, Zhang L, Zhang C, Chen X, Chen Q, Li Z (2014) Comparison of polymerase chain reaction ribotyping, toxinotyping and nutritional aspects of toxin production of Clostridium difficile strains. Biomed Rep 2(4):477–480
Fawley WN, Knetsch CW, MacCannell DR, Harmanus C, Du T, Mulvey MR, Paulick A, Anderson L, Kuijper EJ, Wilcox MH (2015) Development and validation of an internationally-standardized, high-resolution capillary gel-based electrophoresis PCR-ribotyping protocol for Clostridium difficile. PLoS One 10(2):e0118150
Wardal E, Markowska K, Żabicka D, Wróblewska M, Giemza M, Mik E, Połowniak-Pracka H, Woźniak A, Hryniewicz W, Sadowy E (2014) Molecular analysis of vanA outbreak of Enterococcus faecium in two Warsaw hospitals: the importance of mobile genetic elements. Biomed Res Int 2014:575367
Gerner-Smidt P, Scheutz F (2006) Standardized pulsed-field gel electrophoresis of Shiga toxin-producing Escherichia coli: the PulseNet Europe feasibility study. Foodborne Pathog Dis 3(1):74–80
Maiden MC, Bygraves JA, Feil E, Morelli G, Russell JE, Urwin R, Zhang Q, Zhou J, Zurth K, Caugant DA, Feavers IM, Achtman M, Spratt BG (1998) Multilocus sequence typing: a portable approach to the identification of clones within populations of pathogenic microorganisms. Proc Natl Acad Sci U S A 95(6):3140–3145
Jolley KA, Maiden MC (2010) BIGSdb: scalable analysis of bacterial genome variation at the population level. BMC Bioinf 11:595
Bartual SG, Seifert H, Hippler C, Luzon MA, Wisplinghoff H, Rodríguez-Valera F (2005) Development of a multilocus sequence typing scheme for characterization of clinical isolates of Acinetobacter baumannii. J Clin Microbiol 43(9):4382–4390
Da Silva GJ, Mendonça N, Batista G, Duarte A (2010) Sequence types of Portuguese carbapenem-resistant Acinetobacter baumannii isolates collected over 10 years. J Antimicrob Chemother 65(10):2254–2256
Tomaschek F, Higgins PG, Stefanik D, Wisplinghoff H, Seifert H (2016) Head-to-head comparison of two multi-locus sequence typing (MLST) schemes for characterization of Acinetobacter baumannii outbreak and sporadic isolates. PLoS One 11(4):e0153014
Karah N, Haldorsen B, Hermansen NO, Tveten Y, Ragnhildstveit E, Skutlaberg DH, Tofteland S, Sundsfjord A, Samuelsen Ø (2011) Emergence of OXA-carbapenemase- and 16S rRNA methylase-producing international clones of Acinetobacter baumannii in Norway. J Med Microbiol 60(4):515–521
Grosso F, Quinteira S, Peixe L (2011) Understanding the dynamics of imipenem-resistant Acinetobacter baumannii lineages within Portugal. Clin Microbiol Infect 17(8):1275–1279
Jaureguy F, Landraud L, Passet V, Diancourt L, Frapy E, Guigon G, Carbonnelle E, Lortholary O, Clermont O, Denamur E, Picard B, Nassif X, Brisse S (2008) Phylogenetic and genomic diversity of human bacteremic Escherichia coli strains. BMC Genomics 9:560
Wirth T, Falush D, Lan R, Colles F, Mensa P, Wieler LH, Karch H, Reeves PR, Maiden MC, Ochman H, Achtman M (2006) Sex and virulence in Escherichia coli: an evolutionary perspective. Mol Microbiol 60(5):1136–1151
Lacher DW, Steinsland H, Blank TE, Donnenberg MS, Whittam TS (2007) Molecular evolution of typical enteropathogenic Escherichia coli: clonal analysis by multilocus sequence typing and virulence gene allelic profiling. J Bacteriol 189(2):342–350
Lara FB, Nery DR, de Oliveira PM, Araujo ML, Carvalho FR, Messias-Silva LC, Ferreira LB, Faria-Junior C, Pereira AL (2017) Virulence markers and phylogenetic analysis of Escherichia coli strains with hybrid eaec/upec genotypes recovered from sporadic cases of extraintestinal infections. Front Microbiol 8:146
Clermont O, Gordon D, Denamur E (2015) Guide to the various phylogenetic classification schemes for Escherichia coli and the correspondence among schemes. Microbiology 161(5):980–988
Bae IK, Kim J, Sun JY, Jeong SH, Kim YR, Wang KK, Lee K (2014) Comparison of pulsed-field gel electrophoresis & repetitive sequence-based PCR methods for molecular epidemiological studies of Escherichia coli clinical isolates. Indian J Med Res 140(5):679–685
Griffiths D, Fawley W, Kachrimanidou M, Bowden R, Crook DW, Fung R, Golubchik T, Harding RM, Jeffery KJ, Jolley KA, Kirton R, Peto TE, Rees G, Stoesser N, Vaughan A, Walker AS, Young BC, Wilcox M, Dingle KE (2010) Multilocus sequence typing of Clostridium difficile. J Clin Microbiol 48(3):770–778
Lemee L, Dhalluin A, Pestel-Caron M, Lemeland JF, Pons JL (2004) Multilocus sequence typing analysis of human and animal Clostridium difficile isolates of various toxigenic types. J Clin Microbiol 42(6):2609–2617
Dingle KE, Griffiths D, Didelot X, Evans J, Vaughan A, Kachrimanidou M, Stoesser N, Jolley KA, Golubchik T, Harding RM, Peto TE, Fawley W, Walker AS, Wilcox M, Crook DW (2011) Clinical Clostridium difficile: clonality and pathogenicity locus diversity. PLoS One 6(5):e19993
Adams-Haduch JM, Onuoha EO, Bogdanovich T, Tian GB, Marschall J, Urban CM, Spellberg BJ, Rhee D, Halstead DC, Pasculle AW, Doi Y (2011) Molecular epidemiology of carbapenem-nonsusceptible Acinetobacter baumannii in the United States. J Clin Microbiol 49(11):3849–3854
Salipante SJ, SenGupta DJ, Cummings LA, Land TA, Hoogestraat DR, Cookson BT (2015) Application of whole-genome sequencing for bacterial strain typing in molecular epidemiology. J Clin Microbiol 53(4):1072–1079
Eyre DW, Fawley WN, Best EL, Griffiths D, Stoesser NE, Crook DW, Peto TE, Walker AS, Wilcox MH (2013a) Comparison of multilocus variable-number tandem-repeat analysis and whole-genome sequencing for investigation of Clostridium difficile transmission. J Clin Microbiol 51(12):4141–4149
Eyre DW, Cule ML, Griffiths D, Crook DW, Peto TE, Walker AS, Wilson DJ (2013b) Detection of mixed infection from bacterial whole genome sequence data allows assessment of its role in Clostridium difficile transmission. PLoS Comput Biol 9(5):e1003059
Eyre DW, Cule ML, Wilson DJ, Griffiths D, Vaughan A, O’Connor L, Ip CLC, Golubchik T, Batty EM, Finney JM, Wyllie DH, Didelot X, Piazza P, Bowden R, Dingle KE, Harding RM, Crook DW, Wilcox MH, Peto TEA, Walker AS (2013c) Diverse sources of C. difficile infection identified on whole-genome sequencing. N Engl J Med 369(13):1195–1205
Janezic S, Rupnik M (2015) Genomic diversity of Clostridium difficile strains. Res Microbiol 166(4):353–360
Zhou Y, Burnham CA, Hink T, Chen L, Shaikh N, Wollam A, Sodergren E, Weinstock GM, Tarr PI, Dubberke ER (2014) Phenotypic and genotypic analysis of Clostridium difficile isolates: a single-center study. J Clin Microbiol 52(12):4260–4266
Knight DR, Elliott B, Chang BJ, Perkins TT, Riley TV (2015) Diversity and evolution in the genome of Clostridium difficile. Clin Microbiol Rev 28(3):721–741
Mac Aogáin M, Moloney G, Kilkenny S, Kelleher M, Kelleghan M, Boyle B, Rogers TR (2015) Whole-genome sequencing improves discrimination of relapse from reinfection and identifies transmission events among patients with recurrent Clostridium difficile infections. J Hosp Infect 90(2):108–116
Cairns MD, Preston MD, Lawley TD, Clark TG, Stabler RA, Wren BW (2015) Genomic epidemiology of a protracted hospital outbreak caused by a toxin A-negative Clostridium difficile sublineage PCR ribotype 017 strain in London, England. J Clin Microbiol 53(10):3141–3147
Kumar N, Miyajima F, He M, Roberts P, Swale A, Ellison L, Pickard D, Smith G, Molyneux R, Dougan G, Parkhill J, Wren BW, Parry CM, Pirmohamed M, Lawley TD (2016) Genome-based infection tracking reveals dynamics of Clostridium difficile transmission and disease recurrence. Clin Infect Dis 62(6):746–752
Mawer DPC, Eyre DW, Griffiths D, Fawley WN, Martin JSH, Quan TP, Peto TEA, Crook DW, Walker AS, Wilcox MH (2017) Contribution to Clostridium difficile transmission of symptomatic patients with toxigenic strains who are fecal toxin negative. Clin Infect Dis 64(9):1163–1170
Eyre DW, Fawley WN, Rajgopal A, Settle C, Mortimer K, Goldenberg SD, Dawson S, Crook DW, Peto TEA, Walker AS, Wilcox MH (2017) Comparison of control of Clostridium difficile infection in six English hospitals using whole-genome sequencing. Clin Infect Dis 65(3):433–441
Qin J, Dai Y, Ma X, Wang Y, Gao Q, Lu H, Li T, Meng H, Liu Q, Li M (2017) Nosocomial transmission of Clostridium difficile genotype ST81 in a general teaching hospital in China traced by whole genome sequencing. Sci Rep 7(1):9627
Stoesser N, Eyre DW, Quan TP, Godwin H, Pill G, Mbuvi E, Vaughan A, Griffiths D, Martin J, Fawley W, Dingle KE, Oakley S, Wanelik K, Finney JM, Kachrimanidou M, Moore CE, Gorbach S, Riley TV, Crook DW, Peto TEA, Wilcox MH, Walker AS; Modernising Medical Microbiology Informatics Group (MMMIG) (2017) Epidemiology of Clostridium difficile in infants in Oxfordshire, UK: risk factors for colonization and carriage, and genetic overlap with regional C. difficile infection strains. PLoS One 12(8):e0182307
Lewis BB, Carter RA, Ling L, Leiner I, Taur Y, Kamboj M, Dubberke ER, Xavier J, Pamer EG (2017) Pathogenicity locus, core genome, and accessory gene contributions to Clostridium difficile virulence. MBio 8(4). pii: e00885-17
Quesada-Gómez C, López-Ureña D, Acuña-Amador L, Villalobos-Zúñiga M, Du T, Freire R, Guzmán-Verri C, del Mar Gamboa-Coronado M, Lawley TD, Moreno E, Mulvey MR, de Castro Brito GA, Rodríguez-Cavallini E, Rodríguez C, Chaves-Olarte E (2015) Emergence of an outbreak-associated Clostridium difficile variant with increased virulence. J Clin Microbiol 53(4):1216–1226
Dingle KE, Didelot X, Quan TP, Eyre DW, Stoesser N, Golubchik T, Harding RM, Wilson DJ, Griffiths D, Vaughan A, Finney JM, Wyllie DH, Oakley SJ, Fawley WN, Freeman J, Morris K, Martin J, Howard P, Gorbach S, Goldstein EJC, Citron DM, Hopkins S, Hope R, Johnson AP, Wilcox MH, Peto TEA, Walker AS, Crook DW; Modernising Medical Microbiology Informatics Group (2017) Effects of control interventions on Clostridium difficile infection in England: an observational study. Lancet Infect Dis 17(4):411–421
Caspers P, Locher HH, Pfaff P, Diggelmann S, Rueedi G, Bur D, Ritz D (2017) Different resistance mechanisms for cadazolid and linezolid in C. difficile found by whole genome sequencing analysis. Antimicrob Agents Chemother 61(8). pii: e00384-17
Acknowledgements
We would like to acknowledge the much appreciated help of many of our colleagues from bioMérieux Microbiology Research and Development and the bioMérieux Data Analytics Unit.
Funding
No external funding was acquired in the context of the work described in the present publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors were or still are employees of bioMérieux, a company developing and selling infectious disease diagnostics.
Ethics approval and informed consent
Not applicable.
Rights and permissions
About this article
Cite this article
Mirande, C., Bizine, I., Giannetti, A. et al. Epidemiological aspects of healthcare-associated infections and microbial genomics. Eur J Clin Microbiol Infect Dis 37, 823–831 (2018). https://doi.org/10.1007/s10096-017-3170-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-017-3170-x