Abstract
Based on the concept of the individualized nature of sepsis, we investigated the significance of the −251 A/T (rs4073) single nucleotide polymorphism (SNP) of interleukin (IL)-8 in relation to the underlying infection. Genotyping was performed in 479 patients with severe acute pyelonephritis (UTI, n = 146), community-acquired pneumonia (CAP, n = 109), intra-abdominal infections (IAI, n = 119), and primary bacteremia (BSI, n = 105) by restriction fragment length polymorphism of the polymerase chain reaction (PCR) product and compared with 104 healthy volunteers. Circulating IL-8 was measured within the first 24 h of diagnosis by an immunosorbent assay. Carriage of the AA genotype was protective from the development of UTI (odds ratio 0.38, p: 0.007) and CAP (odds ratio 0.30, p: 0.004), but not from IAI and BSI. Protection from the development of severe sepsis/septic shock was provided for carriers of the AA genotype among patients with UTI (odds ratio 0.15, p: 0.015). This was accompanied by greater concentrations of circulating IL-8 among patients with the AA genotype. It is concluded that carriage of rs4073 modifies susceptibility for severe infection in an individualized way. This is associated with a modulation of circulating IL-8.
Similar content being viewed by others
Introduction
Severe sepsis and septic shock are major healthcare problems, affecting millions of people around the world each year, killing one in four and increasing in incidence [1]. The pathophysiology of sepsis is a complex and dynamic process that originates from the host immune response to infection and varies according to the genetic predisposition, immune status of the host, the pathogen, and the type of infection [2].
The Hellenic Sepsis Study Group has been intensively working since 2007 to provide evidence for the individualized nature of the pathogenesis of sepsis. To this end, immunophenotyping on a large scale of 505 patients was conducted during the first 24 h from sepsis onset and ended up with the result that the alterations of the innate and adaptive immune responses that take place upon transition from sepsis to severe sepsis and septic shock differ in relation to the type of underlying infection [3]. A similar analysis indicated that the level of systemic endotoxemia varies, being far greater among patients with primary Gram-negative bacteremia and community-acquired pneumonia (CAP) than among patients with intra-abdominal infections (IAI), acute pyelonephritis (UTI), and ventilator-associated pneumonia [4]. Towards this same concept of individualized pathophysiology, it was recently described that circulating angiopoietin-2 is primarily expressed in sepsis syndrome developing in the field of lung infections [5]. These findings generate the following question: can genetic predisposition for sepsis severity differ considerably in relation with the type of underlying infection? Studies published so far on the impact of single nucleotide polymorphisms (SNPs) of genes encoding cytokine and receptors implicated in the inflammatory cascade never took this as a confounding factor in the analysis or they did not enrol a vast number of patients to allow adequate subgrouping into infection type. However, recent animal data generated in mice with homozygous deficiency for the IL-10 gene showed that this hypothesis may be true [6].
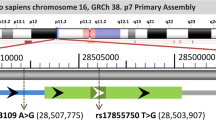
Interleukin (IL)-8 is a proinflammatory cytokine, which possesses a key role in the pathophysiology of sepsis through the activation and chemotaxis of neutrophils [7, 8]. There are 235 SNPs in the IL-8 gene. Among them, the most broadly studied is the −251 A/T SNP (rs4073), which is located in the long arm of chromosome 4, at the position −251 of the gene promoter. Although it is reported that the presence of one A allele increases susceptibility for UTI in the early stages of life [9], these findings cannot be generalizable for all cases of sepsis.
Our hypothesis is that, if this SNP modifies the production of IL-8, it can influence sepsis severity. The aim of the present study was to explore the individualized importance of the carriage of SNP alleles at the −251 promoter position of IL-8 for sepsis severity in light of the type of underlying infection.
Patients and methods
Study design
This multicenter study was conducted in 50 participating departments of the Hellenic Sepsis Study Group. The study protocol was reviewed and approved by the ethics committees of all hospitals of the participating study sites. Written informed consent was provided from all patients or the next of kin for patients unable to consent. Every patient was enrolled once in the study.
The inclusion criteria were: (a) age ≥18 years; (b) Caucasian origin; (c) diagnosis of one of the following infections: CAP, UTI, acute IAI, and primary Gram-negative bacteremia (BSI); (d) presence of sepsis, severe sepsis, or septic shock; and (e) blood sampling within the first 24 h from the first signs of systemic inflammatory response syndrome (SIRS). The exclusion criteria were: (a) infection by human immunodeficiency virus (HIV) infection and (b) neutropenia defined as less than 1000 neutrophils/mm3.
Patients were classified as suffering from uncomplicated sepsis, severe sepsis, or septic shock according to international criteria [10]. Encountered signs of SIRS were the following: (a) body temperature >38 °C or <36 °C; (b) heart rate >90/min; (c) respiratory rate >20/min or PaCO2 <32 mmHg; and (d) white blood cell (WBC) count >12,000 mm3 or <4000 mm3 or >10 % bands [10]. Diagnosis of CAP, UTI, IAI, and BSI was done by internationally accepted criteria [11–13].
One hundred and four healthy volunteers were also enrolled after written informed consent. Criteria for the enrolment of volunteers as controls in the study were negative history of severe infections and negative history of any chronic illness.
Laboratory investigation
Eight milliliters of whole blood were collected after venipuncture of one forearm vein under aseptic conditions within the first 24 h from the presentation of the first signs of SIRS. Three milliliters of whole blood were collected into EDTA tubes and stored at −80 °C until it was processed. The remainder was collected into sterile and pyrogen-free tubes and centrifuged; serum was stored at −80 °C until it was assayed. A second blood drawing or 3 ml of whole blood was randomly performed on day 3, i.e., 48 h after the first blood sampling, for a small subgroup of patients.
Genomic DNA was extracted by the Puregene Blood Core Kit C (Qiagen, Hilden, Germany), according to the manufacturer’s instructions. The restriction fragment length polymorphism-polymerase chain reaction (RFLP-PCR) method was applied to genotype IL-8 promoter SNPs on a SensoQuest Thermal Cycler LabCycler Gradient using 50 ng of genomic DNA at a final volume of 27 μl with 50 mmol l−1 of MgCl2, 20 mmol l−1 of dNTPs, and 1 mmol l−1 of Taq DNA Polymerase (New England BioLabs, Ipswich, MA, USA). For the −251 (A/T) SNP (rs4073), a 349-bp fragment was amplified with the following published primer pairs [14]: forward primer 5′-CAT GAT AGC ATC TGT AAT TAA CTG-3′ and reverse primer 5′-CTC ATC TTT TCA TTA TGT CAG AG-3′. PCR conditions involved an initial denaturation step of 94 °C 5 min, followed by 35 cycles of 94 °C for 45 s and 52 °C for 45 s. Then, another cycle of 72 °C for 7 min was carried out before termination. Ten microliters of the PCR product was digested after incubation for 60 min at 37 °C with 0.5 U of the restriction enzyme MfeI (New England BioLabs, Ipswich, MA, USA). To analyze the −251 A/T polymorphism, gel electrophoresis was performed on the digested PCR products; the AA homozygotes yielded bands of 202 bp and 147 bp, the TT wild type yielded one band of 349 bp, and the TA heterozygotes yielded three bands of 349 bp, 202 bp, and 147 bp. Digested RFLP products were electrophoresed in 2 % agarose gels, stained with ethidium bromide, visualized under ultraviolet light, and photodocumented.
Concentrations of IL-8 in sera were estimated in duplicate by an enzyme-linked immunosorbent assay (eBioscience, Inc., San Diego, CA, USA). The lower limit of detection was 2 pg/ml.
Study endpoints
The primary endpoint was the association of the AA genotypes of the rs4073 SNP of IL-8 for the risk for specific severe infections. The secondary endpoints were the impacts of the AA genotype of the rs4073 SNP of IL-8 on: (i) sepsis severity in relation to the underlying type of infection and (ii) circulating IL-8 in relation to the type of underlying infection.
Statistical analysis
Patients within each infection subgroup were divided into those classified as sepsis and those classified as severe sepsis/septic shock. Comparisons of genotype frequencies in relation to the presence of sepsis or severe sepsis/septic shock for each infection type were done by the Chi-square test. Odds ratios (ORs) and 95 % confidence intervals (CIs) for severe sepsis/septic shock were calculated by Mantel and Haenszel’s statistics. Comparisons of demographics and clinical characteristics between patients bearing specific genotypes were done by the Student’s t-test for quantitative variables with normal distribution of values and by Fisher’s test for qualitative variables. Circulating IL-8 was expressed as medians and 95 % CIs. Comparisons between genotypes were done by the Mann–Whitney U-test because of the linear distribution of values. The percentage changes of IL-8 on day 3 from the baseline were compared between genotypes for patients having the same infection by the Mann–Whitney U-test. Any value of p below 0.05 after adjustment for multiple comparisons was considered significant.
Results
A total of 479 patients were studied: 146 had UTI, 109 had CAP, 119 had IAI, and 105 had BSI. The genotype distribution was in Hardy–Weinberg equilibrium in all infection groups and in healthy controls, as shown in Fig. 1. However, patients with BSI had a trend to be outside the Hardy–Weinberg equilibrium (p: 0.088). Overall, the comparison of genotype frequencies between patients and healthy controls was significant (Chi-square: 12.370, df = 4, p: 0.015). This was due to the frequency of the AA genotype being lower in patients with UTI and CAP than healthy controls (Table 1). This was also the case for the frequency of the A allele; it was significantly lower among patients with UTI and CAP than healthy controls.
In the next step, we studied the genotype distributions between patients admitted with sepsis and those admitted with severe sepsis/septic shock in each infection group (Table 2). These did not differ among patients with CAP and IAI. However, they differed significantly within patients with UTI and BSI. More precisely, the frequency of the AA genotype was lower among patients with UTI admitted with severe sepsis/septic shock, with the OR for severe sepsis/septic shock being 0.15 (95 % CI: 0.03–0.69; p: 0.015). Although the genotype distribution differed significantly between patients with sepsis and severe sepsis/septic shock suffering from BSI, no difference was found between patients with AA and the other genotypes (p: 0.220).
In order to decipher if the reported genotypes are, per se, protective from severe sepsis/septic shock or if this was an epiphenomenon of their clinical severity, the demographic and clinical characteristics were compared between patients of the TT/AT genotypes and patients of the AA genotype. As shown in Table 3, patients with the AA genotype and UTI were younger. They also had lower Acute Physiology and Chronic Health Evaluation II (APACHE II) scores, but this was anticipated because the frequency of severe sepsis/septic shock was lower among them.
Among patients with UTI, carriers of the AA genotype had greater circulating concentrations of IL-8 than carriers of the TT/TA genotypes. No impact of rs4073 AA IL-8 genotypes on circulating IL-8 of patients with CAP, IAI, and BSI was found (Fig. 2).
Impact of rs4073 IL-8 genotypes on circulating IL-8 in relation to the type of underlying infection. Panels A to D provide circulating IL-8 on baseline day 1. The results are provided as medians and 95 % confidence intervals. The circles denote outliers. n is the number of patients for which IL-8 was measured. Panel E provides the percentage of changes of circulating IL-8 on day 3 for a small subgroup of patients. N is the number of patients for which IL-8 was measured. p-Values refer to statistical comparisons between patients with the TT/TA genotypes and patients with the AA genotype. BSI primary bacteremia; CAP community-acquired pneumonia; IAI intra-abdominal infections; UTI acute pyelonephritis
Discussion
This is the first study showing that a specific gene SNP may modulate host susceptibility for a severe infection and clinical severity of sepsis in an individualized module that depends on the type of underlying infection. Our findings suggest that the carriage of the AA genotype of the IL-8 −251A/T SNP is protective from the development of severe UTI and CAP, but not of IAI and BSI. Furthermore, carriage of the AA genotype is protective from the development of severe sepsis/septic shock after UTI.
There are some recent examples of publications focusing on the importance of one gene SNP for the clinical phenotype of one single severe infection instead of studying the severity of sepsis that comprises more than one infection etiology. Most of these studies have been conducted in patients with CAP. One recent genome-wide study revealed that the CC genotype of rs4957796 was associated with favorable outcomes of patients with severe CAP compared to patients of the CT and TT genotypes [15]. In their study, Madách et al. demonstrated that, among patients hospitalized with severe CAP, carriers of the PAI-1 4G/4G and 4G/5G genotypes have higher risk for multiorgan dysfunction and septic shock [16]. Eklund et al. investigated the association between the CRP −717 A > G promoter region polymorphism and mortality from bacteremia caused by Streptococcus pneumoniae and found that mortality was increased in patients homozygous for the CRP −717 GG genotype [17]. However, no published study has, until now, enrolled such a broad study population, as our study and analyzed the results to explore the diverse impact of one gene SNP in the severity of different infections.
Only two studies are available on the impact of the carriage of the −251A IL-8 SNP allele for susceptibility to infection; both were conducted in patients with UTI. More precisely, Artifoni et al. studied a cohort of 265 children with UTI; they found that carriage of the A SNP allele increases the risk of infection of the upper urinary tract with an OR of 2.45 [9]. In their study, Javor et al. demonstrated that the carriage of this SNP increased the likelihood for recurrent attacks of UTI after the first episode of UTI by 62.7 % [18]. The results of both these studies seem to be discrepant compared to our findings. However, all patients with UTI enrolled in the present study had clinical signs of systemic inflammation aggravated or not by organ failures; the studies of Artifoni et al. [9] and Javor et al. [18] did not comprise a similar study population.
The only available observation that one specific gene may affect sepsis differently in relation to the underlying focus of infection comes from two studies in mice. In the first study, mice knock-out for both SR-A and CD36 genes encoding for the scavenger receptors SR-1 and CD36 on neutrophils underwent either lung infection by the intranasal instillation of Staphylococcus aureus or IAI by the intraperitoneal injection of S. aureus. The results revealed that the concomitant lack of genes was deleterious for lung infection and protective from intraperitoneal infection [19]. To the same end, mice knocked out for the IL-10 gene encoding for the anti-inflammatory cytokine IL-10 underwent experimental tularemia by the subcutaneous or intranasal instillation of Francisella tularensis. The absence of the IL-10 gene accelerated death by lung infection, whereas it protected against skin infection [6]. It is evident that studies with knockout mice for a specific gene are not comparable to studies of humans who carry SNPs for one gene. However, these recent animal results start to build the concept that one gene may have a different effect on the phenotype in relation to the studied type of infection and they provide, at least to some extent, indirect support on the individualized impact of SNPs in humans.
One question is how the studied SNP may affect disease severity. A study using splenocytes isolated from recent human cadavers by severe sepsis made it evident that immunosuppression is a common denominator in these patients. When splenocytes were ex vivo stimulated, they failed to produce adequate concentrations of proinflammatory cytokines [20]. As shown in CAP and IAI, where the SNP did not impact clinical severity, circulating IL-8 was similar in all genotypes. However, patients with the TT/TA genotype and UTI had lower circulating IL-8 than patients with the AA genotype. Circulating IL-8 remains unchangeable in these patients during the first 48 h. This finding is compatible with lower immunosuppression after UTI and explains the lower acquisition of severe disease. Contrary to patients with UTI, patients with the TT/TA genotype and BSI present with greater over-time increases of IL-8 than patients with the AA genotype. This is compatible with the greater frequency of severe sepsis/septic shock among these patients.
The present study is the first to provide clear-cut evidence that the nature of sepsis is individualized at a genetic level. The AA genotype of rs4074 of IL-8 modifies the severity of the infection developing after UTI. This is associated with a modulation of the SNP on cytokine production. It is evident that these findings can be conceived as a broadening of our understanding of the pathophysiology of sepsis and point towards the era of personalized medicine, where the genetic fingerprint of the host is of major importance.
References
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb SA, Beale RJ, Vincent JL, Moreno R; Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup (2013) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 41:580–637
Christaki E, Giamarellos-Bourboulis EJ (2014) The beginning of personalized medicine in sepsis: small steps to a bright future. Clin Genet 86:56–61
Gogos C, Kotsaki A, Pelekanou A, Giannikopoulos G, Vaki I, Maravitsa P, Adamis S, Alexiou Z, Andrianopoulos G, Antonopoulou A, Athanassia S, Baziaka F, Charalambous A, Christodoulou S, Dimopoulou I, Floros I, Giannitsioti E, Gkanas P, Ioakeimidou A, Kanellakopoulou K, Karabela N, Karagianni V, Katsarolis I, Kontopithari G, Kopterides P, Koutelidakis I, Koutoukas P, Kranidioti H, Lignos M, Louis K, Lymberopoulou K, Mainas E, Marioli A, Massouras C, Mavrou I, Mpalla M, Michalia M, Mylona H, Mytas V, Papanikolaou I, Papanikolaou K, Patrani M, Perdios I, Plachouras D, Pistiki A, Protopapas K, Rigaki K, Sakka V, Sartzi M, Skouras V, Souli M, Spyridaki A, Strouvalis I, Tsaganos T, Zografos G, Mandragos K, Klouva-Molyvdas P, Maggina N, Giamarellou H, Armaganidis A, Giamarellos-Bourboulis EJ (2010) Early alterations of the innate and adaptive immune statuses in sepsis according to the type of underlying infection. Crit Care 14:R96
Kritselis I, Tzanetakou V, Adamis G, Anthopoulos G, Antoniadou E, Bristianou M, Kotanidou A, Lignos M, Polyzos K, Retsas T, Sassopoulou P, Papaioannou AI, Sinapidis D, Sereti K, Vittoros V, Ghanas P, Gogos C, Giamarellos-Bourboulis EJ (2013) The level of endotoxemia in sepsis varies in relation to the underlying infection: impact on final outcome. Immunol Lett 152:167–172
Lymperopoulou K, Velissaris D, Kotsaki A, Antypa E, Georgiadou S, Tsaganos T, Koulenti D, Paggalou E, Damoraki G, Karagiannidis N, Orfanos SE (2015) Angiopoietin-2 associations with the underlying infection and sepsis severity. Cytokine 73:163–168
Metzger DW, Salmon SL, Kirimanjeswara G (2013) Differing effects of interleukin-10 on cutaneous and pulmonary Francisella tularensis live vaccine strain infection. J Immunol 81:2022–2027
Marshall JC (2005) Neutrophils in the pathogenesis of sepsis. Crit Care Med 33:S502–S505
Hack CE, Hart M, Van Schijndel RJ, Eerenberg AJ, Nuijens JH, Thijs LG, Aarden LA (1992) Interleukin-8 in sepsis: relation to shock and inflammatory mediators. Infect Immun 60:2835–2842
Artifoni L, Negrisolo S, Montini G, Zucchetta P, Molinari PP, Cassar W, Destro R, Anglani F, Rigamonti W, Zacchello G, Murer L (2007) Interleukin-8 and CXCR1 receptor functional polymorphisms and susceptibility to acute pyelonephritis. J Urol 177:1102–1106
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G; International Sepsis Definitions Conference (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Intensive Care Med 29:530–538
Pinson AG, Philbrick JT, Lindbeck GH, Schorling JB (1997) Fever in the clinical diagnosis of acute pyelonephritis. Am J Emerg Med 15:148–151
Christ-Crain M, Stolz D, Bingisser R, Müller C, Miedinger D, Huber PR, Zimmerli W, Harbarth S, Tamm M, Müller B (2006) Procalcitonin guidance of antibiotic therapy in community-acquired pneumonia: a randomized trial. Am J Respir Crit Care Med 174:84–93
Calandra T, Cohen J; International Sepsis Forum Definition of Infection in the ICU Consensus Conference (2005) The international sepsis forum consensus conference on definitions of infection in the intensive care unit. Crit Care Med 33:1538–1548
Andia DC, de Oliveira NF, Letra AM, Nociti FH Jr, Line SR, de Souza AP (2011) Interleukin-8 gene promoter polymorphism (rs4073) may contribute to chronic periodontitis. J Periodontol 82:893–899
Rautanen A, Mills TC, Gordon AC, Hutton P, Steffens M, Nuamah R, Chiche JD, Parks T, Chapman SJ, Davenport EE, Elliott KS, Bion J, Lichtner P, Meitinger T, Wienker TF, Caulfield MJ, Mein C, Bloos F, Bobek I, Cotogni P, Sramek V, Sarapuu S, Kobilay M, Ranieri VM, Rello J, Sirgo G, Weiss YG, Russwurm S, Schneider EM, Reinhart K, Holloway PA, Knight JC, Garrard CS, Russell JA, Walley KR, Stüber F, Hill AV, Hinds CJ; ESICM/ECCRN GenOSept Investigators (2015) Genome-wide association study of survival from sepsis due to pneumonia: an observational cohort study. Lancet Respir Med 3:53–60
Madách K, Aladzsity I, Szilágyi A, Fust G, Gál J, Pénzes I, Prohászka Z (2010) 4G/5G polymorphism of PAI-1 gene is associated with multiple organ dysfunction and septic shock in pneumonia induced severe sepsis: prospective, observational, genetic study. Crit Care 14:R79
Eklund C, Huttunen R, Syrjänen J, Laine J, Vuento R, Hurme M (2006) Polymorphism of the C-reactive protein gene is associated with mortality in bacteraemia. Scand J Infect Dis 38:1069–1073
Javor J, Bucova M, Cervenova O, Kralinsky K, Sadova E, Suchankova M, Liptakova A (2012) Genetic variations of interleukin-8, CXCR1 and CXCR2 genes and risk of acute pyelonephritis in children. Int J Immunogenet 39:338–345
Blanchet C, Jouvion G, Fitting C, Cavaillon JM, Adib-Conquy M (2014) Protective or deleterious role of scavenger receptors SR-A and CD36 on host resistance to Staphylococcus aureus depends on the site of infection. PLoS One 9:e87927
Boomer JS, To K, Chang KC, Takasu O, Osborne DF, Walton AH, Bricker TL, Jarman SD 2nd, Kreisel D, Krupnick AS, Srivastava A, Swanson PE, Green JM, Hotchkiss RS (2011) Immunosuppression in patients who die of sepsis and multiple organ failure. JAMA 306:2594–2605
Acknowledgments
The study was funded by the Hellenic Institute for the Study of Sepsis.
M.G.N. was supported by a Vici grant of the Netherlands Organisation for Scientific Research.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Georgitsi, M.D., Vitoros, V., Panou, C. et al. Individualized significance of the −251 A/T single nucleotide polymorphism of interleukin-8 in severe infections. Eur J Clin Microbiol Infect Dis 35, 563–570 (2016). https://doi.org/10.1007/s10096-015-2571-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-015-2571-y