Abstract
We compared the clinical findings and survival in patients with Mycobacterium avium complex (MAC) and other non-tuberculous mycobacteria (NTM). A total of 167 adult non-human immunodeficiency virus (HIV) patients with at least one positive culture for NTM were included. Medical records were reviewed. The patients were categorised according to the 2007 American Thoracic Society (ATS) criteria. MAC comprised 59 % of all NTM findings. MAC patients were more often female (70 % vs. 34 %, p < 0.001) and had less fatal underlying diseases (23 % vs. 47 %, p = 0.001) as compared to other NTM patients. Symptoms compatible with NTM infection had lasted for less than a year in 34 % of MAC patients but in 54 % of other NTM patients (p = 0.037). Pulmonary MAC patients had a significantly lower risk of death compared to pulmonary other NTM (hazard ratio [HR] 0.50, 95 % confidence interval [CI] 0.33–0.77, p = 0.002) or subgroup of other slowly growing NTM (HR 0.55, 95 % CI 0.31–0.99, p = 0.048) or as rapidly growing NTM (HR 0.47, 95 % CI 0.25–0.87, p = 0.02). The median survival time was 13.0 years (95 % CI 5.9–20.1) for pulmonary MAC but 4.6 years (95 % CI 3.4–5.9) for pulmonary other NTM. Serious underlying diseases (HR 3.21, 95 % CI 2.05–5.01, p < 0.001) and age (HR 1.07, 95 % CI 1.04–1.09, p < 0.001) were the significant predictors of mortality and female sex was a predictor of survival (HR 0.38, 95 % CI 0.24–0.59, p < 0.001) in the multivariate analysis. Pulmonary MAC patients had better prognosis than pulmonary other NTM patients. The symptom onset suggests a fairly rapid disease course.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of non-tuberculous mycobacteria (NTM) in clinical samples has been reported to increase, and they have become a more common finding than classical Mycobacterium tuberculosis in many countries [1–3]. M. avium complex (MAC) has been the most commonly found NTM in human infections in most parts of the world, but in Europe, it makes up only about one-third of NTM isolations [3–6]. Other NTM species in clinical findings are all clearly less common but also variable in different geographical regions. In Europe, M. gordonae consisted of up to 17 %, rapidly growing mycobacteria (RGM) 16 %, M. xenopi 14 % and M. malmoense 1 % of all NTM isolations in 2008 [6]. However, in northern Europe, M. malmoense has been the second or third most common isolate [7–9]. In other parts of the world, M. kansasii, M. abscessus and M. chelonae have been common isolations and, especially in Asia, RGM have been commonly reported [4–6]. During the last year, the interest in NTM infections has increased, with the result of almost an explosion of published articles. NTM have been reported more often in patients with underlying diseases like autoimmune diseases and bronchiectasis or cystic fibrosis [1, 10–13]. Almost 10 % of patients with bronchiectasis have been observed to have NTM and NTM have been suggested to increase the risk of chronic obstructive lung disease [12, 14]. Furthermore, NTM have been reported to be associated with an increased proportion of deaths in USA and increased risk of respiratory failure [15, 16].
MAC has generally been considered to be more pathogenic and more often disease-causing than the other NTM strains [17–19]. This has resulted in the American Thoracic Society (ATS) publishing criteria to discern NTM pulmonary disease from colonisation and the criteria were designed for MAC, M. kansasii and M. abscessus [17]. However, recent studies have shown that ATS criteria did not predict fatal outcome in patients with an NTM isolation [1, 10]. In a population-based study from Denmark, M. xenopi was associated to poorer prognosis than MAC [1]. Furthermore, ATS criteria-positive MAC patients had total mortality of 24 % but MAC-specific mortality was as low as 5 % [20]. A very recent study observed that a single isolation of M. fortuitum in a respiratory specimen seldom indicated progression of disease and, after single isolations of other NTM species, progression was dependent on patient age and radiographic changes, but not on the NTM species [21]. Indeed, the prognostic value of non-MAC NTM isolation still seems to be largely unclarified.
The clinical picture of disease caused by various NTM species has been divergent and even stereotypic in the literature. MAC has been reported to affect more often female non-smokers without underlying diseases and to cause either pulmonary nodules or bronchiectasis with less cavities [7, 20, 22]. Patients with M. xenopi infections have generally been described as middle-aged smoking males with chronic obstructive pulmonary disease (COPD) or prior tuberculosis with upper lobe cavitary infections [23]. M. malmoense has been linked to fibrocavitary disease with tuberculosis or MAC-like symptoms in males with COPD [6]. M. kansasii has been linked to disease indistinguishable from tuberculosis, with a clear male predominance [24, 25]. However, several recent follow-up studies have indicated that pulmonary NTM findings carry a high mortality rate, ranging from 29 to 69 % within 5 years [1, 7, 20]. Most data from disease due to various NTM species come from studies collecting data from patients with one particular NTM. Prognosis, symptoms and underlying factors as compared to MAC with similar setting and follow-up are scarce.
The aim of this study was to ascertain underlying diseases, symptoms and prognostic factors in relation to mortality in NTM infections. In this study, firstly, we retrospectively followed patients with an NTM isolation for, on average, 7 years. Secondly, we evaluated the survival, clinical differences and characteristics in NTM infections between MAC and other NTM.
Materials and methods
Study population
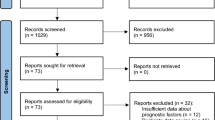
Human immunodeficiency virus (HIV)-negative patients with at least one positive culture finding for NTM from 1990 to the end of 1998 and from 2004 to the end of 2009 were included in the study. Samples for mycobacterial culture were analysed by the Central Microbiological Laboratory of Helsinki City, later Helsinki University Central Hospital Laboratory (HUSLAB), and patients were identified and matched with their records and isolates by using their unique personal identity number; these numbers are given to all residents of Finland.
All patients had been referred to a pulmonary specialist in some of the eight different hospitals in the area of Helsinki University Central Hospital because of pulmonary symptoms compatible with NTM infection. One patient with concomitant findings of M. tuberculosis and M. avium was excluded. Altogether, 167 patients (adults aged 16–94 years) were included in the study population. The patient material has been, in part, presented in our previous studies [7, 26]. For analyses of pulmonary NTM infection, all six patients with a cutaneous NTM isolation were excluded. The numbers of subsequent positive or negative mycobacterial smears, cultures and sampling sites were recorded. Demographic characteristics (age, sex, occupation, body weight, height) were obtained from the patient records. The concomitant diseases were classified as described by McCabe and Jackson [27] as follows: (1) healthy, i.e. no other diseases; (2) chronic non-fatal diseases; (3) ultimately fatal diseases with expected life expectancy of 5 years maximum, such as carcinoma with local spreading and uncompensated hepatic cirrhosis; (4) rapidly fatal diseases with expected survival of no more than 6 months, such as carcinoma with widespread metastases. In particular, information on previous pulmonary diseases, such as bronchiectasis, COPD, pulmonary fibrosis, prior tuberculosis, asthma, pulmonary malignancies and pneumonias, were retrieved. The signs, symptoms, microbiological data and other laboratory findings were all reviewed at the time of the first positive NTM culture and at patient visits closest (6 months) to 1 year after the positive culture. The radiological findings of chest X-ray, computed tomography (CT) scans and high-resolution computed tomography (HRCT) were collected from the original radiologist statements at patient visits closest (6 months) to 1 year after the positive culture and classified as infiltrates, nodules, cavities or bronchiectasis according to the 2007 ATS criteria [17]. Only data relevant to ATS criteria were collected, and in unclear cases, a radiologist was consulted. Previous (6 months) immunosuppressive treatments were reviewed. Systemic or inhalation corticosteroid treatment was recorded when continued for longer than 1 month. Information on previous pulmonary diseases was retrieved. Data on smoking habits were retrieved from the medical records and pulmonary function test questionnaires. The date of death was ascertained from the Finnish Population Register Centre records or patient records.
Microbiological methods
Clinical specimens, except for blood samples, were stained with auramine-O-fluorochrome dye and examined microscopically for acid-fast bacilli (AFB). Cultures positive for AFB were identified by conventional biochemical tests and hybridisation with DNA probes (AccuProbe; Gen-Probe, San Diego, CA, USA). Cultures negative for M. tuberculosis and MAC were identified by amplification and sequencing of the 16S rRNA gene. For those NTM patients with a positive culture finding for NTM from 2004 to the end of 2009, cultures positive for AFB were identified by DNA strip assays (GenoType Mycobacterium CM/AS, Hain Lifescience, Nehren, Germany). MAC, M. avium, and M. intracellulare were all classified as MAC due to changing nomenclature during the study period.
Case definitions
The NTM patients were categorised according to the 2007 ATS criteria [25] in order to reveal how many fulfilled the ATS diagnosis for NTM disease. ATS-positive patients had to meet microbiological, radiological and symptoms criteria. According to these diagnostic criteria, a patient should have the NTM isolated in at least two sputum cultures or one positive culture from a bronchoscopy sample (by lavage or by brush) or from a lung biopsy to fulfill the microbiological criteria. One positive culture from a skin or lymphatic tissue biopsy fulfilled the microbiological criteria for extrapulmonary disease. Radiographic criteria were fulfilled when nodular or cavitary opacities were found on chest radiographs or CT, or when bronchiectasis with multiple small nodules were found by CT/HRCT. The patient had to have symptoms compatible with NTM disease and they included: cough, dyspnoea, fatigue, fever, weight loss, haemoptysis or decreased appetite. If the patient did not meet these microbiological, radiographic and symptomatic criteria, he/she was categorised as ATS-negative.
Statistical methods
The patients having MAC were compared to patients with other NTM strains. The independent samples t-test was used for continuous variables. The Mann–Whitney U-test was used if the assumption of normality was not achieved using transformations. The Chi-squared test and Fisher’s exact test were used for categorical variables. The Kaplan–Meier method was used to estimate the median survival times with 95 % confidence intervals (CIs). The univariate Cox proportional hazards model was used to compare the survival times of the MAC patients to the patients with other NTM strains. Also, the survival times between different mycobacterial species and groups of species were compared. The results are given as hazard ratios (HRs) with 95 % CIs. In addition, two predefined adjusted survival time comparisons between MAC and other NTM strains were conducted, including ATS 2007 positivity (positive vs. negative) and underlying diseases according to the McCabe classification (3–4 vs. 1–2) as additional dichotomous covariates. The interactions were tested including appropriate interaction terms in the models. In the next phase, smoking, fulfilment of ATS 2007 criteria, underlying diseases according to the McCabe classification (1–2 or 3–4), age, gender and smoking were considered as potential additional predictors, as they were all significant predictors in the univariate models. They were introduced to the forward stepwise (criterion for entry p < 0.05) multivariate Cox proportional hazards model. The assumption of proportional hazards was graphically assessed. We obtained plots of log (log S(t)) versus time in order to see the difference between the survival curves. If the survival curves were approximately parallel, then the proportionality assumption was reasonable. Based on those graphical plots, the proportionality assumption was not rejected for any predictor. The number of multivariate analyses was three. They were performed according to the predefined analysis plan. Other multivariate analyses were mainly exploratory or stepwise Cox models using different variable selection methods (different cut-off values for p-values and different blocks of variables). These additional models were performed in order to confirm the results. The predictors in the three final models were: (1) multivariate model with two predictors: fulfilment of MAC and fulfilment of ATS 2007 criteria (Fig. 2, panel A). (2) Multivariate model with two predictors: fulfilment of MAC and underlying diseases according to the McCabe classification (Fig. 2, panel B). (3) Age, gender, smoking, McCabe classification, ATS 2007 fulfilment and MAC fulfilment were introduced as potential predictors to the stepwise multivariate model. Three predictors were selected: McCabe classification, age and gender. Analysis were performed using IBM SPSS Statistics for Windows (version 21.0; IBM Corp., Armonk, NY, USA).
Results
Mycobacterial strains and patient characteristics
MAC comprised the majority (99/167, 59 %) of all NTM findings. Other NTM were isolated in 68 (41 %) patients. RGM M. fortuitum, M. chelonae and M. abscessus comprised 13 % (22/167) of all NTM findings and M. malmoense 9 % (15/167). M. gordonae was found in 10 % (16/167), M. xenopi in 2 % (4/167), M. marinum and M. terrae in 1 % of cases each (2/167). M. paraffinicum and M. triplex were both cultured in one patient (1 %) and other non-specified NTM species in five patients (3 %). Two cases of both M. fortuitum and M. marinum were cultured from skin, like one M. chelonae and one non-specified NTM species, which were not included in the mortality analyses for pulmonary NTM infection.
The mean age of the patients was 66 (range 16–94) years, with no difference between MAC and other NTM patients (Table 1). The majority of MAC patients were female (70 %), whereas only 34 % of patients with other NTM were female (p < 0.001). MAC patients were more lean than other NTM patients, as assessed by the body mass index (BMI, 20.3 kg/m2 vs. 22.9 kg/m2, respectively, p = 0.001). There were also other significant differences between MAC and other NTM patients; MAC patients had less often fatal underlying diseases (23 % vs. 47 %) or a malignancy (12 % vs. 22 %) but more often bronchiectasis (25 % vs. 7 %), more often inhalation corticosteroid use (27 % vs. 13 %) and they were more often non-smokers (58 % vs. 29 %) as compared to patients with other NTM (Table 1).
Symptoms and clinical findings on presentation
Symptoms compatible with NTM disease had lasted for less than a year in 34 % of MAC patients but in 54 % of patients with other NTM (p = 0.01, Table 2). Cough was the most common symptom, reported by 77 % of all patients. MAC patients had more often systemic symptoms like fever (48 % vs. 31 %, p < 0.02) and fatigue (47 % vs. 32 %, p = 0.05) as compared to patients with other NTM.
Only one patient with M. marinum isolated from skin had normal chest X-ray, whereas all the other patients in both groups who had chest X-ray taken had pathological findings (Table 3). There were significantly more patients with nodules in CT or HRCT in the MAC group (34 %) compared with the other NTM group (13 %, p = 0.003, Table 3). Also, bronchiectasis was more common in MAC than other NTM patients (31 % vs. 13 %, p = 0.009, Table 3), whereas infiltrates (42 % vs. 40 %) and cavities (10 % vs. 6 %) were not significantly different between the groups. The radiological findings were concentrated in the right upper and middle lobes in both groups, without any significant difference (Table 3). Diffuse pulmonary findings in the MAC group were more common than in the other NTM group (29 % vs. 15 %, p = 0.03, Table 3).
There were no differences in elementary laboratory tests like haemoglobin, alkaline phosphatase and alanine transaminase levels between the groups (data not shown). The median C-reactive protein (CRP) was 11.0 mg/L (interquartile range, IQR 2.5–45.0) and the median erythrocyte sedimentation rate was 25 mm/h (IQR 11–58) in the MAC group and the corresponding median CRP and erythrocyte sedimentation rate were 18.0 mg/L (IQR 5.0–42.0) and 21 mm/h (IQR 11–42) in the group with other NTM.
Mortality and follow-up
The median follow-up time of these patients was 7.0 (range 0.1–24.5) years, without significant differences between the study populations (6.1 years in patients from 1990 to 1998 vs. 7.4 years in patients from 2004 to 2009, p = 0.12). The follow-up time was at least 5 years in 63.5 % of all patients (60.0 % in patients from 1990 to 1998 vs. 72.3 % in patients from 2004 to 2009, p = 0.14). Patients with pulmonary MAC had a significantly lower risk of death as compared to patients with pulmonary infection of other NTM (HR 0.50, 95 % CI 0.33-0.77, p = 0.002, Fig. 1, panel A). The median survival time was 13.0 years (95 % CI 5.9–20.1) for pulmonary MAC patients and 4.6 years (95 % CI 3.4–5.9) for pulmonary other NTM patients (Fig. 1, panel A). Patients with pulmonary MAC also had significantly lower risk of death as compared to patients with pulmonary infection due to other slowly growing NTM (M. malmonese, M. xenopi, M. paranifficum, M. terrae, M. triplex) (HR 0.55, 95 % CI 0.31–0.99, p = 0.048, Fig. 1, panel B. Also, when compared to patients with pulmonary infection caused by RGM, the risk of death was lower with pulmonary MAC patients (HR 0.47, 95 % CI 0.25–0.87, p = 0.02, Fig. 1, panel C).
Kaplan–Meier survival curves for patients having at least one pulmonary isolation of various non-tuberculous mycobacteria (NTM). Panel A: Mycobacterium avium complex (MAC) (n = 99) compared to all other NTM species (n = 62). The univariate Cox proportional hazards model was applied for the comparison of MAC vs. other NTM; hazard ratio (HR) 0.50, 95 % confidence interval (CI) 0.33–0.77, p = 0.002. Panel B: MAC (n = 99) vs. subgroup 1 of other slowly growing NTM species, including M. malmoense, M. xenopi, M. paranifficum, M. terrae and M. triplex (n = 23). MAC vs. subgroup 1; HR 0.55, 95 % CI 0.31–0.99, p = 0.048. Panel C: MAC (n = 99) vs. a subgroup of rapidly growing mycobacteria (RGM), including M. fortuitum, M. chelonae and M. abscessus (n = 19). MAC vs. RGM; HR 0.47, 95 % CI 0.25–0.87, p = 0.02. Panel D: MAC (n = 99) vs. the most common other NTM (M. fortuitum n = 12, M. malmoense n = 15 or M. gordonae n = 16). MAC vs. M. malmoense; HR 0.64, 95 % CI 0.31–1.31, p = 0.22. MAC vs. M. gordonae; HR 0.64, 95 % CI 0.31–1.31, p = 0.22. MAC vs. M. fortuitum; HR 0.46, 95 % CI 0.22–0.98, p = 0.045
Further, subgroup analysis was done to compare the risk for fatal outcome between pulmonary MAC patients and patients with pulmonary infection due to some defined NTM species. Patients with pulmonary MAC had a significantly lower risk of death as compared to pulmonary M. fortuitum (HR 0.46, 95 % CI 0.22–0.98, p = 0.045) but not a significantly different risk of death as compared to patients with M. malmoense (HR 0.64, 95 % CI 0.31–1.31, p = 0.22) or M. gordonae (HR 0.64, 95 % CI 0.31–1.31, p = 0.22, Fig. 1, panel D).
Among the other NTM group, three analyses were performed using the whole follow-up time and the follow-up time restricted to the first 3 and 5 years. RGM was chosen to be the reference group. There was no significant difference in survival between RGM, M. gordonae or M. malmoense during the first 3 years (p = 0.85). Also, the pairwise comparisons to RGM were non-significant (HR 0.77, 95 % CI 0.26–2.29, p = 0.64 and HR 0.77, 0.26–2.28, p = 0.63 for M. gordonae and M. malmoense, respectively). During the first 5 years, the difference was also non-significant (p = 0.63), and the pairwise comparisons to RGM were HR 0.99, 95 % CI 0.40–2.47, p = 0.99 and HR 0.61, 95 % CI 0.21–1.76, p = 0.36 for M. gordonae and M. malmoense, respectively. During the whole follow-up time, the global test was non-significant (p = 0.90) and the pairwise comparisons were also non-significant (HR 0.89, 95 % CI 0.38–2.07, p = 0.79 and HR 0.82, 95 % CI 0.36–1.90, p = 0.65 for M. gordonae and M. malmoense as compared RGM, respectively).
When fulfilment of MAC and fulfilment of ATS 2007 criteria were predictors in the same multivariate Cox proportional hazards model, the survival among the MAC group (n = 99) was significantly higher than in the other NTM group (n = 68) (HR 0.57, 95 % CI 0.37–0.88, p = 0.01, Fig. 2, panel A) and, among the ATS 2007-positive patients, the survival tended to be higher than among the ATS 2007-negative patients (HR 0.66, 95 % CI 0.44–1.01, p = 0.06, Fig. 2, panel A). The interaction term between these two predictors was non-significant (p = 0.89) and was excluded from the multivariate model. Furthermore, when fulfilment of MAC and fatal underlying diseases (McCabe 3–4 vs. 1–2) were predictors in the same multivariate Cox proportional hazards model, the MAC group had significantly better survival than the other NTM group (HR 0.65, 95 % CI 0.42–1.00, p = 0.048, Fig. 2, panel B) and patients with McCabe 3–4 had significantly worse survival than patients with McCabe 1–2 (HR 3.33, 95 % CI 2.16–5.12, p < 0.001, Fig. 2, panel B). The interaction term between these two predictors was non-significant (p = 0.24) and was excluded from the multivariate model. According to univariate analyses, gender, age and smoking were also significant predictors for fatal outcome (HR 0.40, 95 % CI 0.26–0.62, p < 0.001 for female gender, HR 1.05, 95 % CI 1.03–1.07, p < 0.001 for age in years and HR 1.69, 95 % CI 1.10–2.60, p = 0.02 for smoking). Thus, in addition to fulfilment of MAC, the forward stepwise multivariate Cox model (with p < 0.05) included gender, age, smoking, McCabe classification and ATS 2007 fulfilment as potential predictors. According to this multivariate stepwise model, the only and equally important predictors, were ultimately or rapidly fatal disease (McCabe 3–4) (HR 3.21, 95 % CI 2.05–5.01, p < 0.001), age in years (HR 1.07, 95 % CI 1.04–1.09, p < 0.001) and female sex (HR 0.38, 95 % CI 0.24–0.59, p < 0.001). Thus, fulfilment of MAC or ATS 2007 criteria did not significantly improve the prediction model when McCabe classification, age and gender were already included.
Kaplan–Meier survival curves for all patients with at least one isolation of MAC (n = 99) or other NTM species (n = 68). Panel A: grouped according to American Thoracic Society (ATS) 2007 criteria fulfilment as either positive or negative. The multivariate Cox proportional hazards model yielded a significant effect for MAC (HR 0.57, 95 % CI 0.37–0.88, p = 0.01). The effect of ATS 2007 positivity was non-significant (HR 0.66, 95 % CI 0.44–1.01, p = 0.06). Panel B: grouped according to those with fatal underlying diseases (McCabe 3–4) or without fatal underlying diseases (McCabe 1–2). The multivariate Cox proportional hazards model yielded a significant effect for MAC (HR 0.65, 95 % CI 0.42–1.00, p = 0.048) and for McCabe 3–4 (HR 3.33, 95 % CI 2.16–5.12, p < 0.001)
Discussion
Knowledge on the prognostic factors in NTM infection is limited. Predictors of mortality among NTM infection are unclear and the pathogenicity of various NTM species may be variable. In this study, we observed that patients with MAC had significantly better prognosis as compared to patients with other NTM infections. Pulmonary MAC patients had significantly lower risk of death as compared to patients with pulmonary infection of other slowly growing NTM and as compared to patients with pulmonary RGM. The main predictors of mortality in our study were both ultimately and rapidly fatal underlying diseases, older age and male gender. The findings are consistent with prognostic factors in recent studies [1, 20]. In another recent study, haemoptysis and consolidation in radiological imaging were also found to be signs of poor prognosis [28].
Somewhat surprisingly, in our study, the patients with other NTM had worse prognosis than MAC patients. In accordance with our results, in a recent study, M. xenopi was found to be related to poorer prognosis as compared to MAC [1]. The overall mortality of our MAC patients (median survival of 13.0 years) and other NTM patients (median survival of 4.6 years) corresponded to those observed in recent studies [1, 20]. These results challenge our current view on NTM infections where MAC has been regarded as the main pathogen.
Ultimately and rapidly fatal underlying diseases were the main predictors for mortality and seemed to be the major predisposing factors for infection due to other NTM in our material. Further, MAC patients had significantly less severe underlying diseases and they were more often non-smoking females as compared to other NTM patients. In a subgroup analysis, which included only patients without any fatal underlying diseases, the Kaplan–Meyer survival curves for MAC and other NTM patients were almost superimposable during the 8 years of follow-up (Fig. 2, panel B). Yet, MAC patients who had a fatal underlying disease seemed to have better prognosis than those with isolation of other NTM (Fig. 2, panel B). MAC patients had better outcome than the other NTM patients, even when severe underlying diseases were taken into account in the Cox proportional hazards model analysis. However, it has to be pointed out that 77 % of MAC and 53 % of other NTM patients did not have any fatal underlying diseases.
We could not highlight any single underlying disease behind NTM infections, because we did not test single underlying diseases statistically. However, 74 % of patients in both groups had a previous pulmonary disease. Equally, smoking seemed to be common among our patients. Two-thirds of the other NTM group and less than half of the MAC group were smokers. Smoking was related, for the most part, to male gender, COPD and systemic or inhaled corticosteroid treatment. In a recent study, COPD and corticosteroid treatment was found to be strong risk factors for NTM disease [29]. However, which comes first, the hen or the egg, has evidently not been settled and, at least in some patients, it might be asked whether it is NTM disease or COPD that precedes the other. Namely, NTM infection was suggested to be one of the risk factors for COPD [30]. Heavy smoking history has been previously related to M. malmoense and M. xenopi infection, but the two other common isolations in our material, M. chelonae and M. fortuitum, have not been related to smoking to the same extent [8, 17, 23, 31]. Plausibly, smoking is a contributing factor in the prognosis of NTM infection. This could also partly explain the difference in outcome between MAC and other NTM, as MAC patients were more often female and over half of them were non-smokers, as also described in other studies [22, 32, 33]. The result of ATS criteria fulfilment as a predictor of mortality was controversial when compared to their original idea. Although ATS criteria have been used to select patients for antimycobacterial treatment, ATS criteria fulfilment was not a marker for poor but rather improved prognosis in both MAC and other NTM groups (Fig. 2, panel A). This observation is in line with our previous finding with partly the same patient material and also with a larger registry-based material [1, 10]. Unfortunately, one limitation of this retrospective and descriptive study was that we cannot discern what contribution the NTM infection had in the fatal outcome of the patients and which deaths were due to other causes. Plausibly, severe underlying diseases explain the mortality rate in ATS-negative patients. The lack of severe underlying diseases may be one explaining factor behind the better prognosis of MAC (Fig. 2, panel B).
The short time interval from symptom onset in our study suggests, together with the poor prognosis, that NTM infections are more rapid than generally emphasised. Overall, in 43 % of the patients, symptoms had lasted for less than a year and in 75 % less than 2 years before the first positive NTM culture (Table 3). Of the respiratory symptoms in this study, dyspnoea was complained by half of all patients already when NTM was isolated, which is consistent with other studies [34]. The short time frame from symptom onset is consistent with a recent nationwide cohort study, which suggested that respiratory failure may appear in the first 6 months post-diagnosis and the risk is greater among NTM patients with COPD or MAC [16]. Moreover, pulmonary infections due to M. xenopi or M. malmoense and infections due to M. chelonae or M. abscessus among organ transplant patients have been reported to progress to death within a few years [8, 23, 29, 35, 36]. Interestingly, other NTM infections in our study had a short symptom duration more often than MAC. Systemic symptoms such as fever, fatigue and lower BMI in our MAC patients would all also comply with the longer disease duration in MAC as compared to other NTM. This would fit into prolonged disease history in MAC because low BMI in NTM disease has been associated to abnormal control of leptin and adipokines, suggesting a prolonged disease history [30, 32].
M. malmoense was the third most common NTM isolation, as could be expected and as reported in other studies from Nordic countries [8, 9, 37]. However, RGM (M. fortuitum, M. chelonae, M. abscessus) together formed one-third of all the other NTM isolations. M. gordonae was common in cancer patients. It is often regarded a contamination and its role in clinical infections has been questioned, although it has been reported in patients with cancer or immunosuppression [17]. Although our material was small for detailed analyses between NTM strains, we did not observe any difference in prognosis between patients with M. malmoense, M. gordonae and RGM isolations. Although the precise role of NTM infection for the poor prognosis is still open, it would warrant studies on the effect of medical treatment on prognosis. Namely, in our previous analysis, we could look for the effect of treatment of 3 months with at least two effective drugs and found it to have no effect on prognosis [10]. Accordingly, in a recent analysis on only MAC disease, antimycobacterial therapy was not found to affect prognosis [20]. Clearly, studies on the effect of adequate treatment on the outcome on NTM infection in immunocompetent patients would be needed and the present study cannot give any answer on this. The effect of treatment of severe underlying diseases in the outcome of NTM patients has not been studied either. However, in recent studies, COPD, bronchiectasis and interstitial pulmonary diseases were related to high mortality in patients with NTM infection [15, 38].
Our data show that, together with other recent studies, NTM isolation was a sign of poor prognosis. Pulmonary MAC patients had better prognosis than patients with pulmonary infection due to other NTM. In one-third of MAC patients and a half of other NTM patients, NTM isolation was made within a year of symptom onset, suggesting a fairly rapid disease course. Underlying diseases were the main explanation for poor prognosis. Patients who fulfilled the ATS criteria had better prognosis than ATS-negative patients. The results indicate that the current understanding on the importance of an NTM isolation is insufficient.
References
Andréjak C, Thomsen VØ, Johansen IS, Riis A, Benfield TL, Duhaut P, Sørensen HT, Lescure F-X, Thomsen RW (2010) Nontuberculous pulmonary mycobacteriosis in Denmark: incidence and prognostic factors. Am J Respir Crit Care Med 181:514–521
Cassidy PM, Hedberg K, Saulson A, McNelly E, Winthrop KL (2009) Nontuberculous mycobacterial disease prevalence and risk factors: a changing epidemiology. Clin Infect Dis 49:e124–e129
Marras TK, Mendelson D, Marchand-Austin A, May K, Jamieson FB (2013) Pulmonary nontuberculous mycobacterial disease, Ontario, Canada, 1998–2010. Emerg Infect Dis 19:1889–1891
Simons S, van Ingen J, Hsueh P-R, Van Hung N, Dekhuijzen PNR, Boeree MJ, van Soolingen D (2011) Nontuberculous mycobacteria in respiratory tract infections, Eastern Asia. Emerg Infect Dis 17:343–349
de Mello KGC, Mello FCQ, Borga L, Rolla V, Duarte RS, Sampaio EP, Holland SM, Prevots DR, Dalcolmo MP (2013) Clinical and therapeutic features of pulmonary nontuberculous mycobacterial disease, Brazil, 1993–2011. Emerg Infect Dis 19:393–399
Hoefsloot W, van Ingen J, Andrejak C, Ängeby K, Bauriaud R, Bemer P, Beylis N, Boeree MJ, Cacho J, Chihota V, Chimara E, Churchyard G, Cias R, Daza R, Daley CL, Dekhuijzen PN, Domingo D, Drobniewski F, Esteban J, Fauville-Dufaux M, Folkvardsen DB, Gibbons N, Gómez-Mampaso E, Gonzalez R, Hoffmann H, Hsueh PR, Indra A, Jagielski T, Jamieson F, Jankovic M, Jong E, Keane J, Koh WJ, Lange B, Leao S, Macedo R, Mannsåker T, Marras TK, Maugein J, Milburn HJ, Mlinkó T, Morcillo N, Morimoto K, Papaventsis D, Palenque E, Paez-Peña M, Piersimoni C, Polanová M, Rastogi N, Richter E, Ruiz-Serrano MJ, Silva A, da Silva MP, Simsek H, van Soolingen D, Szabó N, Thomson R, Tórtola Fernandez T, Tortoli E, Totten SE, Tyrrell G, Vasankari T, Villar M, Walkiewicz R, Winthrop KL, Wagner D; Nontuberculous Mycobacteria Network European Trials Group (2013) The geographic diversity of nontuberculous mycobacteria isolated from pulmonary samples: an NTM-NET collaborative study. Eur Respir J 42:1604–1613
Kotilainen H, Valtonen V, Tukiainen P, Poussa T, Eskola J, Järvinen A (2011) Clinical symptoms and survival in non-smoking and smoking HIV-negative patients with non-tuberculous mycobacterial isolation. Scand J Infect Dis 43:188–196
Hoefsloot W, van Ingen J, de Lange WCM, Dekhuijzen PNR, Boeree MJ, van Soolingen D (2009) Clinical relevance of Mycobacterium malmoense isolation in the Netherlands. Eur Respir J 34:926–931
Petrini B (2006) Non-tuberculous mycobacterial infections. Scand J Infect Dis 38:246–255
Kotilainen H, Valtonen V, Tukiainen P, Poussa T, Eskola J, Järvinen A (2013) Prognostic value of American Thoracic Society criteria for non-tuberculous mycobacterial disease: a retrospective analysis of 120 cases with four years of follow-up. Scand J Infect Dis 45:194–202
Ito Y, Hirai T, Fujita K, Maekawa K, Niimi A, Ichiyama S, Mishima M (2015) Increasing patients with pulmonary Mycobacterium avium complex disease and associated underlying diseases in Japan. J Infect Chemother 21:352–356
Chu H, Zhao L, Xiao H, Zhang Z, Zhang J, Gui T, Gong S, Xu L, Sun X (2014) Prevalence of nontuberculous mycobacteria in patients with bronchiectasis: a meta-analysis. Arch Med Sci 10:661–668
Russell CD, Claxton P, Doig C, Seagar A-L, Rayner A, Laurenson IF (2014) Non-tuberculous mycobacteria: a retrospective review of Scottish isolates from 2000 to 2010. Thorax 69:593–595
Yeh JJ, Wang YC, Sung FC, Chou CY, Kao CH (2014) Nontuberculosis mycobacterium disease is a risk factor for chronic obstructive pulmonary disease: a nationwide cohort study. Lung 192:403–411
Mirsaeidi M, Machado RF, Garcia JGN, Schraufnagel DE (2014) Nontuberculous mycobacterial disease mortality in the United States, 1999–2010: a population-based comparative study. PLoS One 9:e91879
Yeh J-J, Wang Y-C, Lin C-L, Chou CY-T, Yeh T-C, Wu B-T, Sung F-C, Kao C-H (2014) Nontuberculous mycobacterial infection is associated with increased respiratory failure: a nationwide cohort study. PLoS One 9:e99260
Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, Holland SM, Horsburgh R, Huitt G, Iademarco MF, Iseman M, Olivier K, Ruoss S, von Reyn CF, Wallace RJ Jr, Winthrop K; ATS Mycobacterial Diseases Subcommittee; American Thoracic Society; Infectious Disease Society of America (2007) An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med 175:367–416
Piersimoni C, Scarparo C (2008) Pulmonary infections associated with non-tuberculous mycobacteria in immunocompetent patients. Lancet Infect Dis 8:323–334
El Helou G, Viola GM, Hachem R, Han XY, Raad II (2013) Rapidly growing mycobacterial bloodstream infections. Lancet Infect Dis 13:166–174
Hayashi M, Takayanagi N, Kanauchi T, Miyahara Y, Yanagisawa T, Sugita Y (2012) Prognostic factors of 634 HIV-negative patients with Mycobacterium avium complex lung disease. Am J Respir Crit Care Med 185:575–583
Lee MR, Yang CY, Shu CC, Lin CK, Wen YF, Lee SW, Ko JC, Wang JY, Lee LN, Yu CJ (2015) Factors associated with subsequent nontuberculous mycobacterial lung disease in patients with a single sputum isolate on initial examination. Clin Microbiol Infect 21:250.e1–250.e7
Kim RD, Greenberg DE, Ehrmantraut ME, Guide SV, Ding L, Shea Y, Brown MR, Chernick M, Steagall WK, Glasgow CG, Lin J, Jolley C, Sorbara L, Raffeld M, Hill S, Avila N, Sachdev V, Barnhart LA, Anderson VL, Claypool R, Hilligoss DM, Garofalo M, Fitzgerald A, Anaya-O’Brien S, Darnell D, DeCastro R, Menning HM, Ricklefs SM, Porcella SF, Olivier KN, Moss J, Holland SM (2008) Pulmonary nontuberculous mycobacterial disease: prospective study of a distinct preexisting syndrome. Am J Respir Crit Care Med 78:1066–1074
Varadi RG, Marras TK (2009) Pulmonary Mycobacterium xenopi infection in non-HIV-infected patients: a systematic review. Int J Tuberc Lung Dis 13:1210–1218
Arend SM, Cerdá de Palou E, de Haas P, Janssen R, Hoeve MA, Verhard EM, Ottenhoff THM, van Soolingen D, van Dissel JT (2004) Pneumonia caused by Mycobacterium kansasii in a series of patients without recognised immune defect. Clin Microbiol Infect 10:738–748
Corbett EL, Churchyard GJ, Clayton T, Herselman P, Williams B, Hayes R, Mulder D, De Cock KM (1999) Risk factors for pulmonary mycobacterial disease in South African gold miners. A case–control study. Am J Respir Crit Care Med 159:94–99
Kotilainen H, Lokki M-L, Paakkanen R, Seppänen M, Tukiainen P, Meri S, Poussa T, Eskola J, Valtonen V, Järvinen A (2014) Complement C4 deficiency—a plausible risk factor for non-tuberculous mycobacteria (NTM) infection in apparently immunocompetent patients. PLoS One 9:e91450
McCabe WR, Jackson GG (1962) Gram-negative bacteremia: I. Etiology and ecology. Arch Intern Med 110:847–855
Gommans EPAT, Even P, Linssen CFM, van Dessel H, van Haren E, de Vries GJ, Dingemans AMC, Kotz D, Rohde GGU (2015) Risk factors for mortality in patients with pulmonary infections with non-tuberculous mycobacteria: a retrospective cohort study. Respir Med 109:137–145
Andréjak C, Nielsen R, Thomsen VØ, Duhaut P, Sørensen HT, Thomsen RW (2013) Chronic respiratory disease, inhaled corticosteroids and risk of non-tuberculous mycobacteriosis. Thorax 68:256–262
Kartalija M, Ovrutsky AR, Bryan CL, Pott GB, Fantuzzi G, Thomas J, Strand MJ, Bai X, Ramamoorthy P, Rothman MS, Nagabhushanam V, McDermott M, Levin AR, Frazer-Abel A, Giclas PC, Korner J, Iseman MD, Shapiro L, Chan ED (2013) Patients with nontuberculous mycobacterial lung disease exhibit unique body and immune phenotypes. Am J Respir Crit Care Med 187:197–205
Taiwo B, Glassroth J (2010) Nontuberculous mycobacterial lung diseases. Infect Dis Clin North Am 24:769–789
Mirsaeidi M, Hadid W, Ericsoussi B, Rodgers D, Sadikot RT (2013) Non-tuberculous mycobacterial disease is common in patients with non-cystic fibrosis bronchiectasis. Int J Infect Dis 17:e1000–e1004
Chan ED, Iseman MD (2010) Slender, older women appear to be more susceptible to nontuberculous mycobacterial lung disease. Gend Med 7:5–18
Lee M-R, Yang C-Y, Chang K-P, Keng L-T, Yen DH-T, Wang J-Y, Wu H-D, Lee L-N, Yu C-J (2013) Factors associated with lung function decline in patients with non-tuberculous mycobacterial pulmonary disease. PLoS One 8:e58214
Cordonnier C, Martino R, Trabasso P, Held TK, Akan H, Ward MS, Fabian K, Ullmann AJ, Wulffraat N, Ljungman P, Alessandrino EP, Pretnar J, Gmür J, Varela R, Vitek A, Sica S, Rovira M; European Blood and Marrow Transplant Group Infectious Diseases Working Party (2004) Mycobacterial infection: a difficult and late diagnosis in stem cell transplant recipients. Clin Infect Dis 38:1229–1236
Knoll BM, Kappagoda S, Gill RR, Goldberg HJ, Boyle K, Baden LR, Fuhlbrigge AL, Marty FM (2012) Non-tuberculous mycobacterial infection among lung transplant recipients: a 15-year cohort study. Transpl Infect Dis 14:452–460
Henriques B, Hoffner SE, Petrini B, Juhlin I, Wåhlén P, Källenius G (1994) Infection with Mycobacterium malmoense in Sweden: report of 221 cases. Clin Infect Dis 18:596–600
Henry MT, Inamdar L, O’Riordain D, Schweiger M, Watson JP (2004) Nontuberculous mycobacteria in non-HIV patients: epidemiology, treatment and response. Eur Respir J 23:741–746
Acknowledgements
The authors declare that they have no conflict of interest. For this type of study, formal consent is not required.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kotilainen, H., Valtonen, V., Tukiainen, P. et al. Clinical findings in relation to mortality in non-tuberculous mycobacterial infections: patients with Mycobacterium avium complex have better survival than patients with other mycobacteria. Eur J Clin Microbiol Infect Dis 34, 1909–1918 (2015). https://doi.org/10.1007/s10096-015-2432-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-015-2432-8