Abstract
Aim
The study aims to increase understanding of edaravone’s efficacy and safety as an amyotrophic lateral sclerosis (ALS) treatment and provide significant insights regarding this field’s future research.
Methods
We conducted a comprehensive search of the Embase, PubMed, Cochrane Library, Web of Science, and Scopus databases for randomized controlled trials and observational studies up until September 2022. We evaluated the studies’ quality using the Cochrane risk of bias tool and the National Institutes of Health tool.
Results
We included 11 studies with 2845 ALS patients. We found that edaravone improved the survival rate at 18, 24, and 30 months (risk ratio (RR) = 1.03, 95% confidence interval (CI) [1.02 to 1.24], P = 0.02), (RR = 1.22, 95% CI [1.06 to 1.41], P = 0.007), and (RR = 1.17, 95% CI [1.01 to 1.34], P = 0.03), respectively. However, the administration of edaravone did not result in any significant difference in adverse effects or efficacy outcomes between the two groups, as indicated by a P value greater than 0.05.
Conclusion
Edaravone improves survival rates of ALS patients at 18, 24, and 30 months with no adverse effects. However, edaravone does not affect functional outcomes. In order to ensure the validity of our findings and assess the results in accordance with the disease stage, it is essential to carry out additional prospective, rigorous, and high-quality clinical trials. The current study offers preliminary indications regarding the effectiveness and safety of edaravone. However, further comprehensive research is required to establish the generalizability and sustainability of the findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Amyotrophic lateral sclerosis (ALS) is a degenerative neurological condition characterized by the gradual deterioration of the motor neurons located in the brain and spinal cord, which are responsible for regulating voluntary muscle movement [1, 2]. ALS is distinguished by muscular weakness, atrophy, and spasticity, resulting in challenges with speech, swallowing, and respiration. It is estimated that there are 4.42 cases of ALS for every 100,000 people in the world’s population, whereas there are 7.7 cases of ALS for every 100,000 people in the USA [3, 4]. Unfortunately, most patients die within 2–3 years after diagnosis due to the failure of respiratory muscles, with a median survival time ranging from 1.5 to 4 years [5, 6]. Although 90 – 95% of cases are sporadic, 5–10% of patients are considered to have the familial form of ALS [5]. It increases the economic burden on health systems [7]. The national cost of ALS may reach € 130 million [7].
Although the pathophysiological mechanisms and environmental factors that affect the disease are still unclear, the evidence suggests that free radicals play a crucial role in the progression of ALS [8, 9]. Free radicals can harm the central nervous system (CNS) by limited ability to scavenge free radicals and weak capability for regeneration [10]. Furthermore, reactive oxygen species (ROS) cause genetic mutations by changing the actions of some enzymes, such as superoxide dismutase and glutamate synthetase [11]. The literature supports the oxidative stress hypothesis by concluding that the CNS tissue of ALS patients contained a higher level of 3-nitrotyrosine (3-NT), a biomarker for oxidative stress [12].
Although many drugs have been tested to treat ALS, riluzole was the only approved drug for about 20 years. Riluzole functions as an anti-glutamatergic agent by diminishing the discharge of glutamate, a neurotransmitter that is hypothesized to be involved in the deterioration of motor neurons in ALS. Clinical trials have demonstrated that riluzole has the potential to decelerate the advancement of ALS and extend the patient’s lifespan [13, 14]. Additional drugs, such as Nuedexta, have received authorization for the management of ALS. It is hypothesized that this drug selectively addresses distinct manifestations of ALS, specifically emotional instability.
Edaravone is a newly tested free radical-scavenging medication that prevents neural cell damage by eliminating hydroxyl radicals and lipid peroxides [15, 16]. Many studies investigated the antioxidant effects of edaravone [17,18,19,20,21]. Yoshino and Kimura concluded that following 14 days of edaravone treatment, the level of 3NT in CSF fluid was considerably lower than at the beginning [22]. Also, edaravone was found to increase plasma uric acid, indicating that it effectively scavenges peroxynitrite [23]. This study aims to update the evidence of edaravone regarding efficacy, safety, and survival outcomes in ALS patients.
Methods
The authors conducted a systematic review and meta-analysis in adherence to the most recent PRISMA updates and Cochrane standards [24, 25].
Literature search and data collection
We searched PubMed, Cochrane library, Embase, Scopus, and Web of Science databases for relevant trials until September 2022. Our search was done using the following search strategy: (edaravone OR norantipyrine OR norphenazone OR edarabone OR radicava OR fraseda OR radicut OR phenylmethylpyrazolone OR methylphenylpyrazolone OR nuravon OR aravon OR “MCI 186” OR “MCI-186” OR “MCI186”) AND (“amyotrophic lateral sclerosis” OR ALS OR “gehrig’s disease” OR “gehrig disease” OR “gehrigs disease” OR “lou gehrig’s” OR “lou-gehrigs” OR “lou gehrig disease”).
Studies selection and eligibility criteria
We included randomized control trials (RCTs) and observational studies that compared edaravone versus control in patients with ALS regarding safety, efficacy, and survival outcomes. We removed the duplicates using EndNote software and screened the title and abstract of all the remaining studies. Studies that might fit the eligibility criteria were full-text screened. Additionally, we screened the references of the included articles to find any missing relevant studies. Two authors did the previous steps, and the third author solved any conflict.
Quality assessment
The Cochrane risk of bias tool (version 1) was used to assess the degree to which the studies under consideration may have been biased [24]. The purpose of this tool is to evaluate diverse forms of bias that may potentially impact the reliability of the study’s outcomes. The application of this tool offers a systematic and precise methodology for identifying and addressing potential bias factors, thus enhancing the general quality and dependability of the research outcomes. Non-RCTs were assessed by the NIH tool [26]. NIH tool for observational studies is composed of 14 questions, and the details about each question are provided in this reference [26]. The quality of evidence for the analyzed outcomes was evaluated using the GRADE methodology (version 20 of GRADEpro, McMaster University, 2013) [27].
Data extraction
The following data were retrieved in Excel sheets:
-
1)
Summary data: study design, site, registration, follow-up duration, inclusion criteria, and outcomes.
-
2)
Baseline data: arms, patients’ number, age, gender, ALS diagnosis definite ALS diagnosis probable, ALS severity grade, duration of disease, riluzole use, and ALS Functional Rating Scale-Revised (ALSFRS-R score) before the observation period.
-
3)
Outcomes:
-
4)
Primary outcomes include survival rates, changes in the 40-item ALS assessment questionnaire (ALSAQ-40 score) and ALSFRS-R score, and any adverse events or serious adverse events.
-
5)
Secondary outcomes: changes in forced vital capacity (FVC), grip strength in Kg and modified Norris scale score, and other adverse events (dysphagia, constipation, gait disturbance, insomnia, musculoskeletal disorders, and upper respiratory tract inflammation).
Data analysis
The process of analyzing data was carried out through the utilization of Review Manager (RevMan) software version 5.4. The measure of effect utilized in the study was either risk ratio (RR) or mean difference (MD), along with 95% confidence intervals (CI), based on the nature of the data (dichotomous or continuous). We reported the significance at P value < 0.05. We assessed the heterogeneity using I-square (I2) and chi-square tests. Homogeneous data (P ≥ 0.1 or I2 < 50%) were pooled in a fixed-effect model, while heterogeneous data (P < 0.1 or I2 > 50%) were analyzed in a random-effect model. We performed subgroup analyses depending on the number of cycles and months of survival.
Results
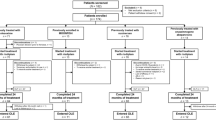
Literature search
After removing duplicate results, the initial search returned a total of 720 unique articles. A subset of 23 studies were determined to be suitable for full-text assessment after undergoing a thorough screening process that involved evaluating the relevance of titles and abstracts. In the end, eleven articles fulfilled the inclusion criteria for our quantitative study after a thorough evaluation [18,19,20,21, 26, 28,29,30,31,32,33] (Fig. 1).
Study characteristics
The studies included in this review comprised four RCTs [18,19,20,21] and seven retrospective cohort articles [26, 28,29,30,31,32,33]. Studies were conducted in the USA, Japan, Italy, Germany, and Iran. The total sample size was 2845 ALS patients, with a disease duration ranging from 1 to 2 years. There was quite a variety of ages represented among the people who took part in the research, with the youngest person being 55 years old and the oldest participant being 71 years old. In order to achieve comprehensive assessment of the outcomes being studied, we have included research works with varying follow-up durations, spanning from 1.5 to 40 months. Most patients were males and were administered riluzole (Tables 1 and 2).
The quality of the included studies
The quality of the RCTs that were incorporated in our analysis was rigorously evaluated to ensure the dependability and accuracy of our results. The majority of the RCTs exhibited a low probability of bias, suggesting a considerable degree of methodological quality and a reliable basis for our analysis. Upon further examination, it was discovered that the study conducted by Eishi-Oskouei et al. exhibited a higher probability of bias [21], which revealed an unclear selection bias risk and a high detection bias risk (Fig. 2). Our cohort studies had a fair quality; the details are in Online Resource 1. Using the GRADE method, the quality of the evidence in its entirety was ranked as being somewhere between moderate and very low (Online Resource 2).
Primary outcomes
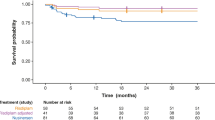
Survival rate
Our findings indicate that edaravone exhibited a favorable outcome in comparison to the control group (RR = 1.11, 95% CI [1.05 to 1.18], P = 0.0004). The results obtained through pooling of data were found to be heterogeneous (P < 0.001, I2 = 96%) (Fig. 3).
At 6 months
Seven studies with 2480 ALS patients reported survival rates at 6 months. The results were insignificant (RR = 1.04, 95% CI [0.94 to 1.14], P value = 0.45) and heterogeneous (P < 0.001, I2 = 98%) (Fig. 3).
At 12 months
The pooled data of six articles with 1485 ALS patients revealed an insignificant difference between the two groups (RR = 1.09, 95% CI [0.95 to 1.25], P = 0.23). The results obtained through pooling of data were found to be heterogeneous (P < 0.001, I2 = 93%) (Fig. 3).
At 18 months
Our findings indicate that the edaravone group exhibited a statistically significant increase in survival rate compared to the control group, as observed in a meta-analysis of five studies involving a total of 1485 patients diagnosed with ALS (RR = 1.13, 95% CI [1.02 to 1.24], P = 0.02). The results obtained through pooling of data were found to be heterogeneous (P = 0.03, I2 = 64%) (Fig. 3).
At 24 months
The survival rate at 24 months was reported in five studies with 1485 ALS patients. The results significantly favored the edaravone group over the control group (RR = 1.22, 95% CI [1.06 to 1.41], P = 0.007). The results obtained through pooling of data were found to be heterogeneous (P = 0.01, I2 = 69%) (Fig. 3).
At 30 months
Five studies were pooled with a sample size of 1485. The survival rate at 30 months was higher in the edaravone group (RR = 1.17, 95% CI [1.01 to 1.34], P = 0.03). The results obtained through pooling of data were found to be homogeneous (P = 0.11, I2 = 48%) (Fig. 3).
Change in ALSAQ 40 score
The pooled estimate (sample size = 367) showed no difference between both groups (MD = − 4.78, 95% CI [− 11.05 to 1.5], P = 0.14). The results obtained through pooling of data were found to be homogeneous (P = 0.63, I2 = 0%) (Fig. 4).
Change in ALSFRS-R score
The overall effect estimate showed no difference in ALSAQ 40 score between both groups (MD = 1.14, 95% CI [− 0.30 to 2.58], P = 0.12). The results obtained through pooling of data were found to be heterogeneous (P < 0.00001, I2 = 93%) (Fig. 5).
After one cycle
Three studies reported this score after the first cycle with a sample size of 253 ALS patients. There was insignificant variation between the groups (MD = 0.02, 95% CI [− 0.47 to 0.51], P = 0.93). The results were homogeneous (P = 0.98, I2 = 0%) (Fig. 5).
After three cycles
Six studies with 1638 ALS patients mentioned this outcome. There were insignificant results (MD = 1.34, 95% CI [− 2.38 to 5.07], P = 0.48). The results obtained through pooling of data were found to be heterogeneous (P < 0.001, I2 = 98%) (Fig. 5).
After six cycles
The pooled data of seven articles with 818 ALS patients showed insignificant results (MD = 2.03, 95% CI [− 0.30 to 4.37], P = 0.09). The results obtained through pooling of data were found to be heterogeneous (P < 0.001, I2 = 84%) (Fig. 5).
After nine cycles
The analysis of 138 ALS patients revealed insignificant results (MD = − 0.63, 95% CI [− 10.69 to 9.44], P = 0.90). The studies were heterogeneous (P = 0.02, I2 = 82%) (Fig. 5).
After 12 cycles
The results of three studies with 129 ALS patients were insignificant (MD = 2.06, 95% CI [− 2.87 to 6.98], P = 0.41). The results obtained through pooling of data were found to be homogeneous (P = 0.11, I2 = 54%) (Fig. 5).
Any adverse event
Five articles (sample size = 1305) revealed insignificant variation between both groups (RR = 1.04, 95% CI [0.96 to 1.13], P = 0.32). The results obtained through pooling of data were found to be homogeneous (P = 0.64, I2 = 0%) (Fig. 6).
Serious adverse events
There were five studies total that documented serious adverse effects. The pooled data showed insignificant results (RR = 0.79, 95% CI [0.52 to 1.18], P = 0.25). The results obtained through pooling of data were found to be homogeneous (P = 0.71, I2 = 0%) (Fig. 7).
Secondary outcomes
Change in FVC (%)
Five articles reported the FVC for 782 ALS patients. There was no improvement in FVC score in ALS patients treated with edaravone (MD = 0.02, 95% CI [− 5.69 to 5.74], P = 0.99). Heterogeneity was observed (P = 0.008, I2 = 71%) (Online Resource 3; Fig. A1).
Change in modified Norris scale
The analyzed data (sample size = 350) showed no variation between the edaravone and control groups (MD = 2.93, 95% CI [− 0.82 to 6.69], P = 0.13). The results obtained through pooling of data were found to be homogeneous (P = 0.63, I2 = 0%) (Online Resource 3; Fig. A2).
Change in grip strength (kg)
Three studies reported this outcome with 358 ALS patients. There was an insignificant difference between both groups (MD = 0.44, 95% CI [− 0.69 to 1.57], P = 0.44). The analysis showed homogeneity (P = 0.81, I2 = 0%) (Online Resource 3; Fig. A3).
Change in pinch strength
The pooled data of 358 ALS patients revealed insignificant differences (MD = 0.09, 95% CI [− 0.17 to 0.35], P = 0.50). The data were homogeneous (P = 0.57, I2 = 0%) (Online Resource 3; Fig. A4).
Other adverse events
The results showed that the edaravone-treated patients had significantly lower musculoskeletal disorders than the control group (RR = 0.84, 95% CI [0.74 to 0.95], P = 0.005). Our results were homogeneous (P = 0.96, I2 = 0%) (Online Resource 3; Fig. A5). Other adverse events such as gait disturbance, dysphagia, constipation, insomnia, and upper respiratory tract inflammation showed insignificant results (P > 0.05). Moreover, the most commonly reported adverse events were gait disturbance [18, 20, 21, 28] and dysphagia [18, 19, 21, 28], reported by four studies with a total of 160 events out of 443 patients in the edaravone-treated patients and 183 out of 444 patients in the control group regarding gait disturbance and 154 out of 499 in the edaravone group and 160 out of 500 in the control group regarding the dysphagia. Nevertheless, we found adverse events with lower incidence than the above such as constipation reported by three studies [18, 19, 21] and insomnia reported by two studies [18, 19] with a total of 24 constipation events out of 181, and 14 insomnia events out of 171 in the edaravone group, and 25 out of 182, and 14 out of 172 in the control group respectively. Finally, upper respiratory tract inflammation was only reported by two studies [19, 20] with a total of 8 events out of 82 patients in the edaravone-treated group, and 3 events out of 80 patients in the control group A10(Online Resource 3; Fig. A6-A10).
Sensitivity analysis
The survival rates at 18 and 24 months were homogeneous after excluding Houzen et al. (2021) [31] (P = 0.1) and Lunetta et al. (2020) [32] (P = 0.53), respectively. The results remained significant (P < 0.05) (Online Resource 3; Fig. A11). The heterogeneity of the change in ALSFRS-R score after six cycles was solved by removing Okada et al. (2018) [33] (P = 0.22). The results remained insignificant (P = 0.3) (Online Resource 3; Fig. A12). The results of FVC were homogeneous (P = 0.77) and still insignificant (P = 0.12) after sensitivity analysis (Online Resource 3; Fig. A13).
Discussion
Our analysis showed that edaravone improved ALS patients’ survival rates after 18, 24, and 30 months compared to the control group. Moreover, edaravone was generally safe and associated with fewer musculoskeletal disorders than the control group. None of the other assessed outcomes differed significantly between the two groups. The aforementioned findings have the potential to guide forthcoming investigations and inform medical professionals’ clinical judgements concerning the administration of edaravone in relation to these particular outcomes.
A limited number of our included studies reported the dropout rate for some reasons. Witzel et al. reported that 6.9% of patients treated with edaravone died before the follow-up endpoint and 3.8% of patients discontinued therapy before follow-up in the same group [29]. Also, Abe et al. mentioned that eight out of 68 patients assigned to the placebo group discontinued due to different reasons; four for adverse events, two withdrew their consent, one had a tracheotomy, and one because of the investigator’s decision [19]. Furthermore, Abe et al. reported that only two patients out of 69 patients assigned to the edaravone group discontinued treatment; one was due to respiratory abnormalities and the other had a tracheotomy [19]. Abe et al. (Grade 3) 2017 reported that four patients discontinued treatment in the edaravone-treatment group; two patients due to their desire, one because of adverse events, and the last one because of worsening ALS that made the hospital visit very hard [20]. However, most of the included studies have addressed this issue by using the intention to treat analysis method accounting for any dropout.
Patients with ALS had a 3-year median survival time after first experiencing symptoms [34]. Current survival data of edaravone were contradictory and were mainly reported in retrospective studies with most studies showing the beneficial effect of Edaravone in overall survival rates [28, 31, 33], which is similar to our analysis results that showed improved survival rates measured at 18, 24, and 30 months. However, in contrast to our results Lunetta et al. and Witel et al. reported no significant difference with Edaravone in survival rates measured up to D-50 and 33 months respectively. [29, 32]
The major purpose of this research was to determine if edaravone is effective for treating ALS, with a particular emphasis on the ALSFRS-R score. ALSFRS-R is a revised version of the ALSFRS, and it encompasses an assessment of respiratory function and has been found to exhibit a significant correlation with the quality of life of a patient [35]. Among those diagnosed with early-stage ALS, edaravone has been shown to be effective in eliciting significant improvements in the ALSFRS-R score compared to a placebo [19]. In contrast to a prior meta-analysis [17], we found no evidence of a significant improvement in ALSFRS-R scores after giving edaravone to a larger sample of ALS patients. The aforementioned results could hold significant implications for the use of edaravone as a therapeutic option for ALS and highlight the necessity for additional investigation in this domain to gain an in-depth understanding of the possible advantages of this intervention.
The results of our study suggest that there was insufficient statistical significance observed in the incidence of most adverse events when comparing both groups, which was also similar to the findings of the last meta-analysis [17]; however, we found significantly fewer musculoskeletal disorders with Edaravone.
Our study provides an updated analysis of the recently published data on the safety and efficacy of Edaravone in ALS. Moreover, this is the first meta-analysis to address survival outcomes. On the other hand, our study had several limitations. First, it included patients who were already taking riluzole and did not consider any interactions between both drugs. Second, many studies did not report the grade of the disease [21, 26, 28,29,30,31,32,33]; therefore, we cannot know the drug’s effect on different stages of the disease. Third, we have data from retrospective studies, which may be affected by selection bias. And finally, the pooled analysis data showed significant heterogeneity in most of the assessed outcomes.
Conclusion
According to our results, the administration of edaravone could potentially improve the survival rates of individuals diagnosed with amyotrophic lateral sclerosis at the 18, 24, and 30-month intervals relative to the control group. Additionally, the use of edaravone appears to be linked with a lower incidence of musculoskeletal disorders, but other assessed outcomes, such as the ALSFRS-R scores, exhibited no significant differences between the two groups. However, more research is required to ascertain its effectiveness in particular patient cohorts and stages of illness.
Data availability
The data supporting this study’s findings are available on request from the corresponding author.
References
Brotman RG, Moreno-Escobar MC, Joseph J et al (2022) Amyotrophic lateral sclerosis. In: StatPearls. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556151/
Raymond J, Oskarsson B, Mehta P, Horton K (2019) Clinical characteristics of a large cohort of US participants enrolled in the National Amyotrophic Lateral Sclerosis (ALS) Registry, 2010–2015. Amyotroph Lateral Scler Frontotemporal Degener 20(5–6):413–420
Xu L, Liu T, Liu L, Yao X, Chen L, Fan D et al (2020) Global variation in prevalence and incidence of amyotrophic lateral sclerosis: a systematic review and meta-analysis. J Neurol 267(4):944–953
Mehta P, Raymond J, Punjani R, Han M, Larson T, Kaye W et al (2017) Prevalence of amyotrophic lateral sclerosis in the United States using established and novel methodologies. Amyotroph Lateral Scler Frontotemporal Degener 2022:1–9
Wijesekera LC, Nigel LP (2009) Amyotrophic lateral sclerosis. Orphanet J Rare Dis 4(1):3
Chiò A, Logroscino G, Hardiman O, Swingler R, Mitchell D, Beghi E et al (2009) Prognostic factors in ALS: a critical review. Amyotroph Lateral Scler 10(5–6):310–323
Achtert K, Kerkemeyer L (2021) The economic burden of amyotrophic lateral sclerosis: a systematic review. Eur J Health Econ 22(8):1151–1166
Polymenidou M, Cleveland DW (2011) The seeds of neurodegeneration: prion-like spreading in ALS. Cell 147(3):498–508
Philips T, Robberecht W (2011) Neuroinflammation in amyotrophic lateral sclerosis: role of glial activation in motor neuron disease. Lancet Neurol 10(3):253–263
Liu Z, Zhou T, Ziegler AC, Dimitrion P, Zuo L (2017) Oxidative stress in neurodegenerative diseases: from molecular mechanisms to clinical applications. Oxid Med Cell Longev 2017:2525967
Zuo L, Zhou T, Pannell BK, Ziegler AC, Best TM (2015) Biological and physiological role of reactive oxygen species—the good, the bad and the ugly. Acta Physiol (Oxf) 214(3):329–348
Beal MF, Ferrante RJ, Browne SE, Matthews RT, Kowall NW, Brown RH Jr (1997) Increased 3-nitrotyrosine in both sporadic and familial amyotrophic lateral sclerosis. Ann Neurol 42(4):644–654
Petrov D, Mansfield C, Moussy A, Hermine O (2017) ALS clinical trials review: 20 years of failure. Are we any closer to registering a new treatment? Front Aging Neurosci 9:68
Miller RG, Mitchell JD (2012) Moore DH 2012 Riluzole for amyotrophic lateral sclerosis (ALS)/motor neuron disease (MND). Cochrane Database Syst Rev 3:Cd001447
Fujisawa A, Yamamoto Y (2016) Edaravone, a potent free radical scavenger, reacts with peroxynitrite to produce predominantly 4-NO-edaravone. Redox Rep 21(3):98–103
Ito H, Wate R, Zhang J, Ohnishi S, Kaneko S, Ito H et al (2008) Treatment with edaravone, initiated at symptom onset, slows motor decline and decreases SOD1 deposition in ALS mice. Exp Neurol 213(2):448–455
Luo L, Song Z, Li X, Huiwang, Zeng Y, Qinwang et al (2019) Efficacy and safety of edaravone in treatment of amyotrophic lateral sclerosis-a systematic review and meta-analysis. Neurol Sci 40(2):235-41
Abe K, Itoyama Y, Sobue G, Tsuji S, Aoki M, Doyu M et al (2014) Confirmatory double-blind, parallel-group, placebo-controlled study of efficacy and safety of edaravone (MCI-186) in amyotrophic lateral sclerosis patients. Amyotroph Lateral Scler Frontotemporal Degener 15(7–8):610–617
Writing group; Edaravone (MCI-186) ALS 18 study group (2017) Safety and efficacy of edaravone in well defined patients with amyotrophic lateral sclerosis: a randomised, double-blind, placebo-controlled trial. Lancet Neurol 16(7):505–12
Writing group; Edaravone (MCI-186) ALS 19 study group. Exploratory double-blind, parallel-group, placebo-controlled study of edaravone (MCI-186) in amyotrophic lateral sclerosis (Japan ALS severity classification: Grade 3, requiring assistance for eating, excretion or ambulation). Amyotroph Lateral Scler Frontotemporal Degener. 2017;18(sup1):40–8
Eishi-Oskouei A, Basiri K (2021) Safety and efficacy of edaravone in well-defined Iranian patients with amyotrophic lateral sclerosis: A parallel-group single-blind trial. Curr J Neurology 20(1):1
Yoshino H, Kimura A (2006) Investigation of the therapeutic effects of edaravone, a free radical scavenger, on amyotrophic lateral sclerosis (Phase II study). Amyotroph Lateral Scler 7(4):241–245
Nagase M, Yamamoto Y, Miyazaki Y, Yoshino H (2016) Increased oxidative stress in patients with amyotrophic lateral sclerosis and the effect of edaravone administration. Redox Rep 21(3):104–112
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds) (2022) Cochrane handbook for systematic reviews of interventions version 6.3. Cochrane, available from https://www.training.cochrane.org/handbook
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Vu M, Tortorice K, Zacher J, Dong D, Hur K, Zhang R et al (2020) 2020 Assessment of use and safety of edaravone for amyotrophic lateral sclerosis in the veterans affairs health care system. JAMA Netw Open 3(10):e2014645-e
Mustafa RA, Santesso N, Brozek J, Akl EA, Walter SD, Norman G et al (2013) The GRADE approach is reproducible in assessing the quality of evidence of quantitative evidence syntheses. J Clin Epidemiol 66(7):736–42 (quiz 42.e1-5)
Brooks BR, Berry JD, Ciepielewska M, Liu Y, Zambrano GS, Zhang J et al (2022) Intravenous edaravone treatment in ALS and survival: an exploratory, retrospective, administrative claims analysis. EClinicalMedicine 52:101590
Witzel S, Maier A, Steinbach R, Grosskreutz J, Koch JC, Sarikidi A et al (2022) Safety and effectiveness of long-term intravenous administration of edaravone for treatment of patients with amyotrophic lateral sclerosis. JAMA Neurol 79(2):121–130
Fortuna A, Gizzi M, Bello L, Martinelli I, Bertolin C, Pegoraro E et al (2019) Safety and efficacy of edaravone compared to historical controls in patients with amyotrophic lateral sclerosis from North-Eastern Italy. J Neurol Sci 404:47–51
Houzen H, Kano T, Horiuchi K, Wakita M, Nagai A, Yabe I (2021) Improved long-term survival with edaravone therapy in patients with amyotrophic lateral sclerosis: A retrospective single-center study in japan. Pharmaceuticals 14(8):705
Lunetta C, Moglia C, Lizio A, Caponnetto C, Dubbioso R, Giannini F et al (2020) The Italian multicenter experience with edaravone in amyotrophic lateral sclerosis. J Neurol 267(11):3258–3267
Okada M, Yamashita S, Ueyama H, Ishizaki M, Maeda Y, Ando Y (2018) Long-term effects of edaravone on survival of patients with amyotrophic lateral sclerosis. ENeurologicalSci 11:11–14
Couratier P, Corcia P, Lautrette G, Nicol M, Preux PM, Marin B (2016) Epidemiology of amyotrophic lateral sclerosis: a review of literature. Rev Neurol (Paris) 172(1):37–45
Cedarbaum JM, Stambler N, Malta E, Fuller C, Hilt D, Thurmond B et al (1999) The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. BDNF ALS Study Group (Phase III). J Neurol Sci 169(1–2):13–21
Bailly C (2019) Potential use of edaravone to reduce specific side effects of chemo-, radio- and immuno-therapy of cancers. Int Immunopharmacol 77:105967
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by AZN, IK, AIH, and AGT. The first draft of the manuscript was written by MME, AHF, MMEE, and MSZ. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study does not involve human participants.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nourelden, A.Z., Kamal, I., Hagrass, A.I. et al. Safety and efficacy of edaravone in patients with amyotrophic lateral sclerosis: a systematic review and meta-analysis. Neurol Sci 44, 3429–3442 (2023). https://doi.org/10.1007/s10072-023-06869-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-06869-8