Abstract
Objective
To systematically evaluate the rehabilitation effect of non-invasive brain stimulation (NIBS) on disorder of consciousness (DOC) after brain injury and compare the effects of different NIBSs.
Methods
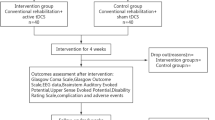
Randomized controlled trials (RCTs) on the effect of NIBS on DOC after brain injury were retrieved from the PubMed, Cochrane Library, Web of Science, CNKI, VIP, Wanfang Data, and CBM databases from inception to October 2022. The risk of bias and quality of the trials were assessed following the Cochrane Handbook of Systematic Reviews and the physiotherapy evidence database Jadad Scale. Statistical analysis was conducted with RevMan 5.4 and R Studio. This study was registered on PROSPERO (No. CRD42022371334).
Results
A total of 28 articles were included involving 1118 patients. Meta-analysis showed that NIBS combined with routine rehabilitation had the highest effect than the routine rehabilitation and the sham NIBS combined with routine rehabilitation. The cumulative probability ranking results showed that the rTMS was best. The order of network meta-analysis with GCS (Glasgow Coma Scale) as the outcome index is rTMS combined with routine rehabilitation > tDCS combined with routine rehabilitation > routine rehabilitation > NIBS sham stimulation combined with routine rehabilitation. The order of network meta-analysis with CRS-R (Coma Recovery Scale–Revised) as the outcome index is rTMS combined with routine rehabilitation > tDCS combined with routine rehabilitation > NIBS sham stimulation combined with routine rehabilitation > routine rehabilitation. For patients with different conditions of DOC, the subgroup analysis results showed that rTMS improved the effect of patients with severe DOC better than those with unclear conditions of DOC, but the overall results of the two groups were not significantly different. On the contrary, the effect of tDCS on patients with DOC whose condition was not clear was better than that on patients with severe DOC, and the effect on patients with severe DOC was not significant (P > 0.05). In terms of safety, only 9 articles mentioned ADRs in the included literature, including 8 articles without ADRs, and 1 article with ADRs.
Conclusion
Based on the research results of various indicators, NIBS can improve DOC after brain injury, and the rTMS is the best. Limited by the number and the quality of literature, the above conclusions need more high-quality research to verify.












Similar content being viewed by others
Data Availability
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
References
Zhang YH, Zeng XL, Shen W et al (2017) Statical analysis of the sensitivity of CRS-R Scale projects in consciousness evaluation. Rehabil Med 27(05):17–21+28. https://doi.org/10.3724/sp.j.1329.2017.05017
Zhao JZ (2020) Clinical diagnosis and treatment of consciousness disorders. J Clin Neurosurg 17(01):1–3+7. https://doi.org/10.3969/j.issn.1672-7770.2020.01.001
Pisegna JM, Kaneoka A, Pearson WG Jr et al (2016) Effects of non-invasive brain stimulation on post-stroke dysphagia: a systematic review and meta-analysis of randomized controlled trials. Clin Neurophysiol 127(1):956–968. https://doi.org/10.1016/j.clinph.2015.04.069
Palm U, Hasan A, Strube W et al (2016) tDCS for the treatment of depression: a comprehensive review. Eur Arch Psychiatry Clin Neurosci 266(8):681–694. https://doi.org/10.1007/s00406-016-0674-9
Hara T, Shanmugalingam A, McIntyre A et al (2021) The effect of non-invasive brain stimulation (NIBS) on attention and memory function in stroke rehabilitation patients: a systematic review and meta-analysis. Diagnostics (Basel) 11(2):227. https://doi.org/10.3390/diagnostics11020227
Liew S-L, Santarnecchi E, Buch ER et al (2014) Non-invasive brain stimulation in neurorehabilitation: local and distant effects for motor recovery. Front Hum Neurosci 8:378. https://doi.org/10.3389/fnhum.2014.00378
Lefaucheur J-P, André-Obadia N, Antal A et al (2014) Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS). Clin Neurophysiol 125(11):2150–2206. https://doi.org/10.1016/j.clinph.2014.05.021
Tremblay S, Lepage J-F, Latulipe-Loiselle A et al (2014) The uncertain outcome of prefrontal tDCS. Brain Stimul 7(6):773–783. https://doi.org/10.1016/j.brs.2014.10.003
Diana M, Raij T, Melis M et al (2017) Rehabilitating the addicted brain with transcranial magnetic stimulation. Nat Rev Neurosci 18(11):685–693. https://doi.org/10.1038/nrn.2017.113
Terao Y, Ugawa Y (2002) Basic mechanisms of TMS. J Clin Neurophysiol 19(4):322–343. https://doi.org/10.1097/00004691-200208000-00006
Li LL, Huang HL (2022) Noninvasive neuromodulation for unilateral neglect after stroke: a systematic review and network meta-analysis. Neurol Sci 43(10):5861–5874. https://doi.org/10.1007/s10072-022-06187-5
Kiefer C, Sturtz S, Bender R (2015) Indirect comparisons and network meta-analyses. Dtsch Arztebl Int 112(47):803–808. https://doi.org/10.3238/arztebl.2015.0803
Jadad AR, Moore RA, Carroll D et al (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17(1):1–12. https://doi.org/10.1016/0197-2456(95)00134-4
Shen LB, Ou YH, Yang CY et al (2019) The effect of high- frequency repetitive transcranial magnetic stimulation on consciousness recovery in traumatic brain injury patients with disorders of consciousness. Chin J Rehabil Med 34(12):1411–1417. https://doi.org/10.3969/j.issn.1001-1242.2019.12.004
Xia XY, Bai Y, Yang Y et al (2020) Study on repetitive transcranial magnetic stimulation in MCS patients after TBI. J Clin Neurosurg 17(01):11–15. https://doi.org/10.3969/j.issn.1672-7770.2020.01.004
Huang XY (2020) The value analysis of repeated transcranial magnetic stimulation in patients with severe head injury. Health Manag 23:100
Li YL, Li JL, Wang DD et al (2021) Effect of high-frequency repetitive transcranial magnetic stimulation on neuroelectrophysiology and cerebrospinal fluid excitatory amino acid level in patients with disorders of consciousness after severe craniocerebral injury. J Clin Med Pract 25(17):57–60. https://doi.org/10.7619/jcmp.20211483
Xie Y, He YJ, Chen Y et al (2011) Effect on cerebral blood flow velocity and electro neurophysiology in unconscious patients with brain injury after repetitive transcranial magnetic stimulation. Chin J Clinicians (Electronic Edition) 5(18):5375–5379. https://doi.org/10.3877/cma.j.issn.1674-0785.2011.18.030
Feng F (2020) The role of repetitive transcranial magnetic stimulation combined with conventional wake-up therapy in the treatment of patients with disturbance of consciousness after craniocerebral injury. Shanxi Med J 49(04):442–445. https://doi.org/10.3969/j.issn.1000-7377.2020.04.014
Zhu X, Jiang WY, Wang WS et al (2019) The clinical and imaging study of patients with severe consciousness disorder with repeated transcranial magnetic stimulation. Modern Med Health Res 3(03):49–50
Liu H, He JH, Xiong YJ et al (2021) The effect of repeated transcranial magnetic stimulation on neuroelectric physiology and clinical efficacy of children with severe brain injury. Chin J Rehabil 36(01):34–37. https://doi.org/10.3870/zgkf.2021.01.008
Zhu X, Jiang WY, Lin W et al (2020) The effect of repeated transcranial magnetic stimulation on plant state after brain injury was analyzed. Electron J Clin Med Lit 7(04):74–75+164. https://doi.org/10.16281/j.cnki.jocml.2020.04.045
Li SX, Li MH, Wu XP et al (2021) Observation of the effect of repeated transcranial magnetic stimulation combined with acupuncture on the awakening of patients with severe craniocerebral injury and coma. Clin J Chin Med 13(18):40–41+64. https://doi.org/10.3969/j.issn.1674-7860.2021.18.016
Lv C, Fei Z, Hu XA et al (2016) Awakening efficacy of low frequency repetitive transcranial magnetic stimulation for the patients with vegetative state after craniocerebral injury. China Med Herald 13(17):69–72
Li H, Xu J, Tian M et al (2021) The value of transcranial magnetic stimulation under the guidance of stereotactic in treatment of severe cranial-cerebral injury. Anhui Med Pharm J 25(05):979–982. https://doi.org/10.3969/j.issn.1009-6469.2021.05.033
Zhang Y, Du JB, Li R et al (2020) The application of P300 in evaluating therapeutic efficacy of transcranial direct current stimulation in patients with minimally conscious state. Chin J Rehabil Med 35(01):22–28. https://doi.org/10.3969/j.issn.1001-1242.2020.01.005
Feng F, Sun XL, Ju F et al (2020) Clinical effect of transcranial direct current stimulation in the treatment of consciousness disorder after severe craniocerebral injury and its influence on patients’ neurological function. Clin Res Pract 5(15):7–8+16. https://doi.org/10.19347/j.cnki.2096-1413.202015003
Fan J, Zhong Y, Wang H et al (2022) Repetitive transcranial magnetic stimulation improves consciousness in some patients with disorders of consciousness. Clin Rehabil 36(7):916–925. https://doi.org/10.1177/02692155221089455
He RH, Wang HJ, Zhou Z et al (2021) The influence of high-frequency repetitive transcranial magnetic stimulation on endogenous estrogen in patients with disorders of consciousness. Brain Stimuli 14(3):461–466. https://doi.org/10.1016/j.brs.2021.02.014
He F, Wu M, Meng F et al (2018) Effects of 20 Hz repetitive transcranial magnetic stimulation on disorders of consciousness: a resting-state electroencephalography study. NeuralPlast 2018:5036184. https://doi.org/10.1155/2018/5036184
Cincotta M, Giovannelli F, Chiaramonti R et al (2015) No effects of 20 Hz-rTMS of the primary motor cortex in vegetative state: a randomized, sham-controlled study. Cortex 71:368–376. https://doi.org/10.1016/j.cortex.2015.07.027
Zhang XH, Han P, Zeng YY et al (2021) The clinical effect of repetitive transcranial magnetic stimulation on the disturbance of consciousness in patients in a vegetative state. Front Neurosci 15:647517. https://doi.org/10.3389/fnins.2021.647517
Martens G, Fregni F, Carrière M et al (2019) Single tDCS session of motor cortex in patients with disorders of consciousness: a pilot study. Brain Inj 33(13–14):1679–1683. https://doi.org/10.1080/02699052.2019.1667537
Martens G, Lejeune N, O’Brien AT et al (2018) Randomized controlled trial of homebased 4-week tDCS in chronic minimally conscious state. Brain Stimul 11(5):982–990. https://doi.org/10.1016/j.brs.2018.04.021
Martens G, Kroupi E, Bodien Y et al (2020) Behavioral and electrophysiological effects of network-based frontoparietal tDCS in patients with severe brain injury: a randomized controlled trial. Neuroimage Clin 28:102426. https://doi.org/10.1016/j.nicl.2020.102426
Estraneo A, Pascarella A, Moretta P et al (2017) Repeated transcranial direct current stimulation in prolonged disorders of consciousness: a double-blind cross-over study. Neurol Sci 375:464–470. https://doi.org/10.1016/j.jns.2017.02.036
Thibaut A, Wannez S, Donneau AF et al (2017) Controlled clinical trial of repeated prefrontal tDCS in patients with chronic minimally conscious state. Brain Inj 31(4):466–474. https://doi.org/10.1080/02699052.2016.1274776
Wu M, Yu Y, Luo L et al (2019) Efficiency of repetitive transcranial direct current stimulation of the dorsolateral prefrontal cortex in disorders of consciousness: a randomized sham-controlled study. Neural Plast 2019:7089543. https://doi.org/10.1155/2019/7089543
Thibaut A, Bruno MA, Ledoux D et al (2014) tDCS in patients with disorders of consciousness: sham-controlled randomized double-blind study. Neurology 82(13):1112–1118. https://doi.org/10.1212/WNL.0000000000000260
Zhang Y, Song W, Du J et al (2017) Transcranial direct current stimulation in patients with prolonged disorders of consciousness: combined behavioral and event-related potential evidence. Front Neurol 8:620. https://doi.org/10.3389/fneur.2017.00620
Kumar R, Yadav R, Prajapati HP et al (2022) Effect of Transcranial direct current stimulation (tDCS) on altered conscious patients after traumatic brain injury & cerebrovascular accident: a randomized clinical control trial. Neurol Asia 27(2):457–463. https://doi.org/10.54029/2022nre
Barra A, Rosenfelder M, Mortaheb S et al (2022) Transcranial pulsed-current stimulation versus transcranial direct current stimulation in patients with disorders of consciousness: a pilot, sham-controlled cross-over double-blind study. Brain Sci 12(4):429. https://doi.org/10.3390/brainsci12040429
Mancuso M, Abbruzzese L, Canova S et al (2017) Transcranial random noise stimulation does not improve behavioral and neurophysiological measures in patients with subacute vegetative-unresponsive wakefulness state (VS-UWS). Front Hum Neurosci 11:524. https://doi.org/10.3389/fnhum.2017.00524
Chen CC, Hong WJ, Wang SZ et al (2022) Advances in the application of transcranial electrical stimulation in stroke rehabilitation. Chin J Phys Med Rehabil 44(08):754–760. https://doi.org/10.3760/cma.j.issn.0254-1424.2022.08.020
Wu JJ, Du JB, Zhang Y et al (2019) Advances in the treatment of patients with consciousness disorder after brain injury. Chin J Rehabil Med 34(09):1125–1130. https://doi.org/10.3969/j.issn.1001-1242.2019.09.026
Wagner T, Valero-Cabre A, Pascual-Leon A (2007) Noninvasive human brain stimulation. Annu Rev Biomed Eng 9:527–565
Wijdicks EF (2006) Clinical scales for comatose patients: the Glasgow Coma Scale in historical context and the new FOUR Score. Rev Neurol Dis 3(3):109–117
American Congress of Rehabilitation Medicine, Brain Injury-Interdisciplinary Special Interest Group, Disorders of Consciousness Task Force, Seel RT, Sherer M, Whyte J, Katz DI, Giacino JT, Rosenbaum AM, Hammond FM, Kalmar K, Pape TL, Zafonte R, Biester RC, Kaelin D, Kean J, Zasler N (2010) Assessment scales for disorders of consciousness: evidence-based recommendations for clinical practice and research. Arch Phys Med Rehabil 91(12):1795–813. https://doi.org/10.1016/j.apmr.2010.07.218
Lvstad M, Frslie KF, Giacino JT et al (2010) Reliability and diagnostic characteristics of the JFK coma recovery scale-revised: exploring the influence of rater’s level of experience. J Head Trauma Rehabil 25(5):349–356. https://doi.org/10.1097/HTR.0b013e3181cec841
Di Lorenzo F et al (2018) Impaired spike timing dependent cortico-cortical Plasticity in Alzheimer’s disease patients. J Alzheimers Dis: JAD 66(3):983–991. https://doi.org/10.3233/JAD-180503
O’Neal CM, Schroeder LN, Wells AA et al (2021) Patient outcomes in disorders of consciousness following transcranial magnetic stimulation: a systematic review and meta-analysis of individual patient data. Front Neurol 12:694970. https://doi.org/10.3389/fneur.2021.694970
Li S, Zaninotto AL, Neville IS et al (2015) Clinical utility of brain stimulation modalities following traumatic brain injury: current evidence. Neuropsychiatr Dis Treat 11:1573–1586. https://doi.org/10.2147/NDT.S65816
Author information
Authors and Affiliations
Contributions
Yaning Li: study conception and design, data acquisition, and analysis. Yaning Li, Lingling Li, Hailiang Huang: data interpretation, drafting and revising the manuscript. Hailiang Huang provided guidance regarding the methodology. All the authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, Y., Li, L. & Huang, H. Effect of non-invasive brain stimulation on conscious disorder in patients after brain injury: a network meta-analysis. Neurol Sci 44, 2311–2327 (2023). https://doi.org/10.1007/s10072-023-06743-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-06743-7