Abstract
In 2018, the first list of rare diseases was published by the National Health Council of China, and multiple sclerosis (MS) was included in this list. Since then, the Chinese government and neurologists have made efforts to improve the clinical outcomes of patients with MS. During last few years, the incidence of MS in China was also investigated. The early and accurate diagnosis of MS was improved due to the application and promotion of magnetic resonance imaging and new diagnosis criteria. The market for and medical insurance access to disease-modifying therapies (DMTs) has been greatly accelerated, which has provided more treatment options and improved clinical outcomes for patients with MS, as well as reduced treatment cost. The pattern of MS in China is gradually changing, from delayed to early diagnosis, and from no treatment to treatment with DMTs during remission. This narrative review aimed to summarize an update to the status of MS in China, including incidence and prevalence, diagnosis, and available treatments. This would help to better understand the diagnosis and treatment gap between mainland China and other Asian regions, demonstrating the necessity of accurate diagnosis and optimized treatment of MS in China.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple sclerosis (MS) is a chronic inflammatory and immune-mediated demyelinating disease of the central nervous system [1]. Reports from Atlas of MS estimated that there were 2.8 million people with MS in the world in 2020, a number that has increased by 0.5 million compared with 2013 [2, 3]. In China, the first list of rare diseases was published by the National Health Council of China until 2018, and MS was included in this list [4]. In the past 2 decades, several classes of disease-modifying therapies (DMTs) were approved by the US Food and Drug Administration (FDA) and European Medicines Agency (EMA) [5], changing the dynamics of MS and making MS a more manageable disease [6]. However, in China, interferon β injection was the only marketed DMT before 2018 [7]. Teriflunomide was the first oral DMT approved by China’s National Medical Products Administration (NMPA) in 2018, 6 years later than the FDA approval [7, 8]. This narrative review aims to summarize the current status of MS in China, including incidence/prevalence, diagnosis, and treatment, to characterize the diagnosis and treatment gap between China and other Asian countries, demonstrating the necessity of accurate diagnosis and optimized treatment of MS in China.
Incidence and prevalence of MS in China
In China, the first MS case was recorded by Peking Union Medical College Hospital in 1926, and the first autopsy report of MS was made by Shanghai Huashan Hospital in 1957 [9]. The first nationwide study reported that the incidence of MS in China was 0.235 per 100,000 person-years in 2018 based on an administrative database of the National Hospital Quality Monitoring System [10]. The incidence of MS in China was higher in high-latitude areas [10], which was similar to reports from other countries [11,12,13].
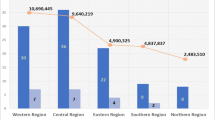
There are no nationwide studies assessing the general prevalence of MS in China, although several reports have been published that describe the prevalence of MS in different regions (Table 1) [14,15,16,17]. From these reports, the number of patients with MS in mainland China seems to have not changed significantly in the past 3 decades and is significantly lower compared with Europe and the USA (over 100/100,000 people) [18]. One of the regional reports, a door-to-door survey in 1992, revealed that the prevalence of MS was 2.1/100,000 people in an autonomous county, Yunnan Province [14]. Cheng et al. reported that the crude prevalence of MS was 1.39/100,000 people in Shanghai in 2005 [15]. In 2013, the estimated prevalence rate of MS was 5.2/100,000 people in Shandong Province [17]. Another population-based study using national medical insurance databases of six provinces in mainland China reported that the urban prevalence rate was 2.91, 2.32, and 2.44 per 100,000 people in 2012, 2015, and 2016, respectively [16]. Li et al. reported that the prevalence rate of MS was 2.39/100,000 people after comprehensive analysis of three prevalence studies [19]. In summary, based on these reports, the prevalence rate of MS ranges from one to five per 100,000 people in mainland China.
Unlike in mainland China, the number of patients with MS has greatly increased in Hong Kong and Taiwan during the past 40 years. The prevalence rate of MS in Hong Kong was 0.88 and 0.77 per 100,000 people in 1989 and 2002, respectively [20, 21]. In 2006, the prevalence rose to 4.8 per 100,000 people in Hong Kong due to the application of magnetic resonance imaging (MRI) and implementation of a hospital computerized surveillance system [22]. Similarly, the prevalence rate of MS among Chinese individuals was 0.8/100,000 population in northern Taiwan in 1976 [23]. According to a population-based epidemiological study, the prevalence rate of MS was 2.96/100,000 in 2005 in Taiwan [24] and rose to 6.69/100,000 in 2015 [25].
In other Asian countries like Japan, the prevalence of MS has also gradually increased in the past years [26, 27]. The prevalence rate was two to four per 100,000 people in the 1960s and one to four per 100,000 people in the 1980s [28, 29]. In 2003, the crude prevalence was 7.7/100,000 people [30]. Based on an analysis of a health insurance claims database, the prevalence rate of MS rose from 15/100,000 to 19/100,000 people between 2011 and 2015 in Japan [27]. The prevalence of MS in northern Japan was 8.1, 12.6, 16.2, and 18.6 per 100,000 people in 2001, 2006, 2011, and 2016, respectively [26].
In summary, the prevalence rate of MS did not change greatly in mainland China over the last decades, whereas it has gradually increased in Hong Kong, Taiwan, and Japan. Several factors may have contributed to this phenomenon: (1) the risk of developing MS might be lower in mainland China, which should be verified by nationwide prevalence studies; (2) the diagnosis of MS is delayed because of lack of disease awareness among neurologists and radiologists; (3) patients with MS are under-diagnosed because they have a lack of disease knowledge and no access to specialized MS centers; and (4) there is no nationwide registry system for MS in China.
In 2021, the China National Registry of Central Nervous System Inflammatory Demyelinating Diseases (CNRIDD; NCT05154370, www.clinicaltrials.gov) was initiated and focused on the establishment of a national, multicenter disease registry to provide disease-related information on patients with inflammatory demyelinating diseases (IDDs) in China. This project will generate a comprehensive picture about IDD including MS, providing the nationwide incidence and prevalence, diagnosis, treatment and facilitating management of patients with IDD in China in the future.
Delayed diagnosis of MS in mainland China
The currently used MS diagnosis criteria is the 2017 McDonald criteria, according to Expert Consensus for the Diagnosis and Treatment of Multiple Sclerosis in China 2018 (MS Expert Consensus) [31, 32], which indicates that the diagnosis criteria in China are consistent with international guidelines. The updated diagnosis criteria increased the sensitivity and accuracy of MS diagnosis in China.
According to evaluation results from Suzhou, China, the 2005 McDonald criteria were more sensitive than Poser criteria (90.2% vs. 72.0%) for MS diagnosis [33]. In Chinese patients with clinically isolated syndrome (CIS), the 2017 McDonald criteria had a higher sensitivity (75.0% vs. 14.6%) and higher accuracy (67.7% vs. 36.9%) compared with the 2010 version [34]. Therefore, the 2017 McDonald criteria are suitable for the early diagnosis of MS in Chinese patients. These findings may also be one of the explanations for the previous low prevalence of MS in mainland China, because the diagnosis criteria (Poser and McDonald 2010) with low sensitivity and accuracy could cause under-diagnosis in patients with MS.
Additionally, data suggest that MS diagnosis in Chinese patients is delayed for 5–10 years since the first disease onset, especially in smaller, nonspecialized centers. It was found that the mean age at MS diagnosis was 36 years, whereas the mean age at MS onset was 31 years, based on the analysis from Beijing Tiantan Hospital, a leading MS center in China [35]. Based on the nationwide hospital-based study, the mean age at MS diagnosis was 45.3 years old in tertiary hospitals of China [10]. In two review papers published in 2009, the age of MS onset was around 30 years in Chinese patients with MS [9, 36], which was similar to findings from other studies [37, 38]. This means that there was a delay of more than 10 years for MS diagnosis and/or a high proportion of misdiagnosis or missed diagnosis of MS.
One of the major reasons for the delayed diagnosis is seemingly a lack of knowledge about the disease among patients with MS. In the Multiple Sclerosis Patient Survival Report 2021 in China (MS Survival Report 2021), 1540 patients with MS from 41 centers in mainland China were included and completed the questionnaires prepared for this survival survey, including diagnosis, treatment, prognosis, and quality of life. In this report, 24.5% of the patients with MS did not seek clinicians’ help immediately upon initial onset of MS and there was a 1.33-year delay from MS onset to the first hospital visit. Among patients, 96.3% had never heard of MS at the time of diagnosis in this report [39], which was consistent with the results from the MS Social Survey 2020 and other smaller studies [40, 41].
Another factor for delayed MS diagnosis is misdiagnosis of MS. According to the MS Survival Report 2021, 50.3% of patients were initially misdiagnosed or under-diagnosed at the first hospital visit, with a 2.27-year delay of accurate diagnosis [39]. Based on the MS Social Survey 2020, the average interval was around 1 year from the first hospital visit to final diagnosis of MS; in one patient, the longest interval was 22 years [40]. A multicenter analysis of top hospitals in China showed 55.1% of patients did not get a confirmed diagnosis of MS during the first visit, with a delayed duration of 0.9 years [41], which did not change in the last few years [39].
Taken together, although the currently used MS diagnosis criteria in China are the 2017 McDonald criteria, which are recommended by various guidelines and consensus for early diagnosis, the accurate diagnosis of MS in China still seems considerably delayed. Most Chinese neurologists and radiologists are up-to-date in employing diagnostic tools for MS, including the use of recent diagnostic criteria and MRI. However, patients with MS generally lack insight on the disease, thus highlighting the importance of strengthening patient education and raising awareness of MS in order to promote early and accurate diagnosis of MS. It is likely that the real prevalence of MS might be much higher than current published data due to misdiagnosis and underdiagnosis of MS. Hopefully, this situation will be improved with the implementation of the CNRIDD program.
DMT availability for MS in mainland China
An increasing number of new MS drugs have been approved and marketed in the last 2 decades (Fig. 1) [5], and DMTs have become standard of care for patients with MS in many countries [42,43,44,45]. However, there are only seven DMTs approved by NMPA (Table 2) [46]. Before 2018, there was only one marketed DMT (interferon-beta) [7]; most patients were prescribed corticosteroids, immunosuppressants, immunoglobins, and interferons [36]. These medications were recommended in the MS Expert Consensus (2014) recommendations for the management of MS [47].
Since the first list of rare diseases was published in 2018 [4], the Chinese government has made efforts to accelerate medication access to improve the prognosis of patients with rare disease. In 2018, the first oral DMT (teriflunomide) was approved by the NMPA [5]. Siponimod, fingolimod, dimethyl fumarate and ofatumumab were also approved within 3 years [48,49,50], providing more treatment options for Chinese patients with MS. Furthermore, efforts have also been made to accelerate the access of medical insurance to reduce treatment cost of MS by National Healthcare Security Administration in China. In 2019, interferon β-1a and teriflunomide [51], and in 2020, fingolimod and siponimod, were included into national medical insurance [52]. In addition to DMTs, fampridine, the only FDA- and EMA-approved drug to improve walking impairments in patients with MS [53, 54] was granted accelerated approval in May 2021 [55] and was included in national medical insurance in December 2021 [56]. The fast access to market and medical insurance indicates that increasing attention has been paid to the management of clinical symptoms to improve the quality of life in patients with MS in China.
Although the Chinese government has made attempts to provide more cost-effective DMTs, the proportion of treated patients is still low [39, 40, 46]. According to the MS Survival Report 2021, 58% of patients with MS did not receive any medication during MS remission [39], which was similar to the MS Survival Report 2018 with 60% of untreated patients [57]. It has been noted that DMT coverage in patients with MS has almost doubled within 3 years, from 10 to 18% between 2018 and 2020 [39, 57]; however, this rate was still lower than Australia and Germany, where the DMT penetrance was 64% and 57%, respectively [58, 59].
As for the patients who did not receive any treatment, approximately 30% did not think it was necessary to receive a maintenance treatment during remission to prevent MS relapse [39, 57]. Around 30% of patients did not receive treatment because the cost of medication was high [39, 57], and 59% discontinued treatment because they could not afford the cost of medication [40].
In summary, treatment options are still limited for patients with MS in China, but attempts are being made to provide DMTs and medical insurance inclusion to provide more DMTs with reduced cost for these patients. It was noted that the approval interval of DMTs was greatly shortened from over 10 years to 1 year between FDA and NMPA (Table 2). In addition to providing access to DMTs, both neurologists and patients should be educated to increase the DMT coverage during MS remission, which will improve the prognosis of MS.
Future perspectives
To improve outcomes for patients with MS in China, and to raise the awareness of MS in China, measures should be taken to improve the early and accurate diagnosis and patient knowledge of MS. Moreover, treatment options are very limited in mainland China, with only four oral DMTs approved by the NMPA out of the nine approved by the FDA. All four of these oral DMTs were approved by NMPA since 2018, when MS was included in the first list of rare diseases. The Chinese government has made efforts to shorten the approval interval between NMPA and FDA; thus, it is expected that an increasing number of DMTs will be introduced to China in the near future, which might help to reduce MS disease activity and improve the quality of life in patients with MS.
The inclusion of medical insurance should be encouraged to reduce the cost of MS treatment, which will benefit more patients with MS. In addition to disease treatments, more attention should be paid to the management of clinical symptoms, such as cognition, fatigue, and mental health, to improve the quality of life in MS patients.
References
Oh J, Vidal-Jordana A, Montalban X (2018) Multiple sclerosis: clinical aspects. Curr Opin Neurol 31:752–759
Walton C, King R, Rechtman L, Kaye W, Leray E, Marrie RA et al (2020) Rising prevalence of multiple sclerosis worldwide: insights from the Atlas of MS third edition. Mult Scler 26:1816–1821
Browne P, Chandraratna D, Angood C, Tremlett H, Baker C, Taylor BV et al (2014) Atlas of Multiple Sclerosis 2013: a growing global problem with widespread inequity. Neurology 83:1022–1024
(2018) List of the first batch of rare diseases. National Health Council of China. http://www.gov.cn/zhengce/zhengceku/2018-12/31/content_5435167.htm. Accessed May 11 2018.
Doshi A, Chataway J (2016) Multiple sclerosis, a treatable disease. Clin Med (Lond) 16:s53–s59
Vargas DL, Tyor WR (2017) Update on disease-modifying therapies for multiple sclerosis. J Investig Med 65:883–891
Xu Y, Mao N, Chirikov V, Du F, Yeh Y-C, Liu L et al (2019) Cost-effectiveness of teriflunomide compared to interferon beta-1b for relapsing multiple sclerosis patients in China. Clin Drug Investig 39:331–340
English C, Aloi JJ (2015) New FDA-approved disease-modifying therapies for multiple sclerosis. Clin Ther 37:691–715
Cheng Q, Cheng XJ, Jiang GX (2009) Multiple sclerosis in China–history and future. Mult Scler 15:655–660
Tian DC, Zhang C, Yuan M, Yang X, Gu H, Li Z et al (2020) Incidence of multiple sclerosis in China: a nationwide hospital-based study. Lancet Reg Health West Pac 1:100010
Simpson S Jr, Blizzard L, Otahal P, Van der Mei I, Taylor B (2011) Latitude is significantly associated with the prevalence of multiple sclerosis: a meta-analysis. J Neurol Neurosurg Psychiatry 82:1132–1141
Lam T, VoPham T, Munger KL, Laden F, Hart JE (2020) Long-term effects of latitude, ambient temperature, and ultraviolet radiation on the incidence of multiple sclerosis in two cohorts of US women. Environ Epidemiol 4:e0105
Krökki O, Bloigu R, Reunanen M, Remes AM (2011) Increasing incidence of multiple sclerosis in women in Northern Finland. Mult Scler 17:133–138
Hou JB, Zhang ZX (1992) Prevalence of multiple sclerosis: a door-to-door survey in Lan Cang La Hu Zu Autonomous County. Yunnan Province of China Neuroepidemiology 11:52
Cheng Q, Miao L, Zhang J, Ding SJ, Liu ZG, Wang X et al (2007) A population-based survey of multiple sclerosis in Shanghai, China. Neurology 68:1495–1500
Xu L, Chen L, Wang S, Feng J, Liu L, Liu G et al (2021) Urban prevalence of multiple sclerosis in China: a population-based study in six provinces. Eur J Neurol 28:1636–1644
Liu X, Cui Y, Han J (2016) Estimating epidemiological data of multiple sclerosis using hospitalized data in Shandong Province. China Orphanet J Rare Dis 11:73
Howard J, Trevick S, Younger DS (2016) Epidemiology of multiple sclerosis. Neurol Clin 34:919–939
Li J, Mehta I, Lally C, Flanders WD, Tian D-C, Everage N, et al. (2021) Multiple sclerosis incidence and prevalence in China. In: 13th Congress of the Pan-Asian Committee for Treatment and Research in Multiple Sclerosis. Virtual
Yu YL, Woo E, Hawkins BR, Ho HC, Huang CY (1989) Multiple sclerosis amongst Chinese in Hong Kong. Brain 112(Pt 6):1445–1467
Lau KK, Wong LK, Li LS, Chan YW, Li HL, Wong V (2002) Epidemiological study of multiple sclerosis in Hong Kong Chinese: questionnaire survey. Hong Kong Med J 8:77–80
Lau KK, Wong WWY, Sheng B, Yu ITS, Fung BH, Li HL et al (2008) The clinical course of multiple sclerosis patients in Hong Kong. J Neurol Sci 268:78–82
Hung TP, Landsborough D, Hsi MS (1976) Multiple sclerosis amongst Chinese in Taiwan. J Neurol Sci 27:459–484
Lai CH, Tseng HF (2009) Population-based epidemiological study of neurological diseases in Taiwan: I. Creutzfeldt-Jakob Dis Multiple Sclerosis Neuroepidemiol 33:247–253
Fang CW, Wang HP, Chen HM, Lin JW, Lin WS (2020) Epidemiology and comorbidities of adult multiple sclerosis and neuromyelitis optica in Taiwan, 2001–2015. Mult Scler Relat Disord 45:102425
Houzen H, Kondo K, Horiuchi K, Niino M (2018) Consistent increase in the prevalence and female ratio of multiple sclerosis over 15 years in northern Japan. Eur J Neurol 25:334–339
Ogino M, Okamoto S, Ohta H, Sakamoto M, Nakamura Y, Iwasaki K et al (2017) Prevalence, treatments and medical cost of multiple sclerosis in Japan based on analysis of a health insurance claims database. Clin Exp Neuroimmunol 8:318–326
Okinaka S, Reese HH, Katsuki S, Ueki K, Kuroiwa Y, Araki S et al (1966) The prevalence of multiple sclerosis and other neurological diseases in Japan. Acta Neurol Scand 42:68–76
Kuroiwa Y (1982) Clinical and epidemiological aspects of multiple sclerosis in Japan. Jpn J Med 21:135–140
Kira J (2009) Recent advances of multiple sclerosis research in Japan. Rinsho Shinkeigaku 49:549–559
Thompson AJ, Banwell BL, Barkhof F, Carroll WM, Coetzee T, Comi G et al (2018) Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol 17:162–173
(2018) Expert consensus for the diagnosis and treatment of multiple sclerosis in China: 2018 version. Chinese Journal of Neuroimmunology and Neurology 25:387-394
Cheng XJ, Cheng Q, Xu LZ, Zhao HQ, Zhao Z, Wang W et al (2010) Evaluation of multiple sclerosis diagnostic criteria in Suzhou, China–risk of under-diagnosis in a low prevalence area. Acta Neurol Scand 121:24–29
Zheng Y, Shen C-H, Wang S, Yang F, Cai M-T, Fang W et al (2020) Application of the 2017 McDonald criteria in a Chinese population with clinically isolated syndrome. Ther Adv Neurol Disord 13:1756286419898083
Fan Y-p, You Y-z, Cheng K-l, Yang T, Wu W (2012) Clinical features and traditional Chinese medicine syndrome types presentation of multiple sclerosis: an analysis of 261 cases. Journal of Capital Medical University 33:301–306
Cheng XJ, Xu LZ (2009) Review of the diagnosis and clinical features of multiple sclerosis in China. Neurosci Bull 25:38–42
Liu G, Zhang F, Hu Y, Jiang Y, Gong Z, Liu S et al (2017) Multiple sclerosis risk pathways differ in Caucasian and Chinese populations. J Neuroimmunol 307:63–68
Zhang Y, Xu Y, Xu T, Yin H, Zhu Y, Peng B et al (2020) Prediction of long-term disability in Chinese patients with multiple sclerosis: a prospective cohort study. Mult Scler Relat Disord 46:102461
(2021) Multiple Sclerosis Patient Survival Report 2021. In: China Alliance for Rare Disease
Yu S, Zhang H, Li X, Yuan H, Liu Y, Xin Y (2020) 2020 General Social Survey on Patients with Multiple Sclerosis in China. In: China Alliance for Rare Disease
Liu X, Xu Y, Wang W, Wang L, Zhang M, Li C et al (2021) Clinical features and difficulties in diagnosis of multiple sclerosis in China. J Capital Med Univ 42:360–366
Yamout B, Sahraian M, Bohlega S, Al-Jumah M, Goueider R, Dahdaleh M et al (2020) Consensus recommendations for the diagnosis and treatment of multiple sclerosis: 2019 revisions to the MENACTRIMS guidelines. Mult Scler Relat Disord 37:101459
Marques VD, Passos GRD, Mendes MF, Callegaro D, Lana-Peixoto MA, Comini-Frota ER et al (2018) Brazilian Consensus for the Treatment of Multiple Sclerosis: Brazilian Academy of Neurology and Brazilian Committee on Treatment and Research in Multiple Sclerosis. Arq Neuropsiquiatr 76:539–554
Cristiano E, Rojas JI, Abad P, Adoni T, Barahona J, Becker J et al (2018) Consensus recommendations for the diagnosis and treatment of primary progressive multiple sclerosis in Latin America. J Neurol Sci 393:4–13
Hobart J, Bowen A, Pepper G, Crofts H, Eberhard L, Berger T et al (2019) International consensus on quality standards for brain health-focused care in multiple sclerosis. Multiple Sclerosis (Houndmills, Basingstoke, England) 25:1809–1818
Zhou R, Zeng Q, Yang H, Xu Y, Tan G, Liu H et al (2021) Status of immunotherapy acceptance in Chinese patients with multiple sclerosis: analysis of Multiple Sclerosis Patient Survival Report 2018. Front Neurol 12:651511–651511
Qiu W, Xu Y (2015) Expert consensus for the diagnosis and treatment of multiple sclerosis in China: 2014 version. In: Chinese Journal of Neuroimmunology and Neurology Neuroimmunology group of neurology branch for Chinese medical association and Neuroimmunology branch of China society of immunology, 362–367
(2020) Approval of siponimod by China National Medical Products Administration National Medical Products Administration. https://www.nmpa.gov.cn/directory/web/nmpa/yaowen/ypjgyw/20200511091401189.html. Accessed May 11 2020.
(2021) Announcement of granted drug approval certificate National Medical Products Administration. https://www.nmpa.gov.cn/zwfw/sdxx/sdxxyp/yppjfb/20210423084822190.html. Accessed April 23 2021.
(2021) Announcement of granted drug approval certificate. National Medical Products Administration https://www.nmpa.gov.cn/zwfw/sdxx/sdxxyp/yppjfb/20210415154452160.html.
(2019) Print and publish the 2019 national medical insurance negotiation admission drug list. The National Medical Insurance Bureau and the Ministry of Human Resources and Social Security. http://www.nhsa.gov.cn/art/2019/8/20/art_37_1666.html. Accessed August 20 2019.
(2020) 2020 drug list of national medical insurance. National Healthcare Security Administration. http://www.nhsa.gov.cn/art/2020/12/28/art_37_4220.html. Accessed December 28 2020.
Kim ES (2017) Fampridine prolonged release: a review in multiple sclerosis patients with walking disability. Drugs 77:1593–1602
McDonald S, Clements JN (2011) Dalfampridine: a new agent for symptomatic management of multiple sclerosis. Am J Health Syst Pharm 68:2335–2340
(2021) Announcement of granted drug approval certificate National Medical Products Administration. https://www.nmpa.gov.cn/zwfw/sdxx/sdxxyp/yppjfb/20210514104413133.html. Accessed May 14 2021.
(2021) 2021 drug list of national medical insurance. National Healthcare Security Administration. http://www.nhsa.gov.cn/art/2021/12/3/art_37_7429.html. Accessed December 3 2021.
(2019) Multiple Sclerosis Patient Survival Report 2018. In: Chinese Society of Neurology, China
Campbell JA, Simpson S Jr, Ahmad H, Taylor BV, van der Mei I, Palmer AJ (2020) Change in multiple sclerosis prevalence over time in Australia 2010–2017 utilising disease-modifying therapy prescription data. Mult Scler 26:1315–1328
Engelhard J, Oleske DM, Schmitting S, Wells KE, Talapala S, Barbato LM (2022) Multiple sclerosis by phenotype in Germany. Mult Scler Relat Disord 57:103326
Funding
This work was supported by Biogen Inc. and the National Natural Science Foundation of China (grant number 82171338).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
None.
Conflict of interest
YZ is an employee of Biogen Inc. DJ and CY declared that there were no conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jia, D., Zhang, Y. & Yang, C. The incidence and prevalence, diagnosis, and treatment of multiple sclerosis in China: a narrative review. Neurol Sci 43, 4695–4700 (2022). https://doi.org/10.1007/s10072-022-06126-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-06126-4