Abstract
Background
Available evidence reports conflicting data on retinal thickness in progressive supranuclear palsy (PSP). In studies including healthy controls, PSP showed either the thinning of the retinal nerve fiber layer, macular ganglion cell, inner nuclear, or outer retina layer.
Objectives
The goals of the present study were to describe retinal layer thickness in a large cohort of PSP compared to healthy controls and in PSP phenotypes using spectral-domain optical coherence tomography (SD-OCT). The additional objective was to verify the relationship between retinal layers thickness and clinical variables in PSP.
Methods
Using a cross-sectional design, we examined retinal structure in 27 PSP patients and 27 controls using standard SD-OCT. Motor and cognitive impairment in PSP was rated with the PSP rating scale and the Montreal Cognitive Assessment battery (MoCA), respectively. Eyes with poor image quality or confounding diseases were excluded. SD-OCT measures of PSP and controls were compared with parametric testing, and correlations between retinal layer thicknesses and disease severity were evaluated.
Results
PSP showed significant thinning of the inner retinal layer (IRL), ganglion cell layer (GCL), inner plexiform layer (IPL), and the outer plexiform layer (OPL) compared to healthy controls. PSP phenotypes showed similar retinal layer thicknesses. Retinal layer thickness correlated with MoCA visuospatial subscore (p < 0.001).
Conclusions
We demonstrated PSP patients disclosed thinner IRL, GCL, IPL, and OPL compared to healthy controls. Furthermore, we found a significant correlation between visuospatial abilities and retinal layers suggesting the existence of a mutual relationship between posterior cognitive function and retinal structure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
PSP is a rare, neurodegenerative tauopathy with relentless progression characterized by postural instability, oculomotor disturbances, akinesia, and cognitive deficits [1]. Based on the diverse combination of the core clinical features, different phenotypes of the disease have been described with the most common being Richardson’s syndrome (PSP-RS) [1].
Few neuroimaging markers have been reported to support the clinical diagnosis of PSP in comparison with healthy controls and other parkinsonian syndromes [2]. Complementary, no clinical or instrumental assessment showed sufficient reliability in discriminating between PSP-RS and the other variant syndromes of PSP (vPSP) [3,4,5].
Despite intense efforts from the research community, reliable in vivo biomarkers are lacking [1, 6]. Hence, a definite diagnosis and phenotypization of PSP still relies on pathological examination showing a high density of neurofibrillary tangles and neuropil threads in the basal ganglia and brainstem with a characteristic distribution associated with tau-positive astrocytes.
SD-OCT is a noninvasive, inexpensive technique providing high-resolution retinal imaging with elevated reproducibility. Given tau aggregates have been detected in retina layers in both mice expressing mutant tau and patients affected by PSP, in vivo imaging of the retina may represent a promising biomarker of PSP [7,8,9]. Yet, available evidence reports conflicting data on retinal thickness in PSP patients. In studies including healthy controls, PSP showed either thinning of retinal nerve fiber layer (RNFL), macular ganglion cell, inner nuclear, or outer retina layer [10,11,12,13]. However, several limitations including a limited number of patients examined and a lack of disease-specific clinical assessments hamper drawing any conclusion from previous studies on the importance of retinal thickness as an in vivo biomarker in PSP [10,11,12,13].
The goals of the present study were to evaluate retinal layer thickness in a large cohort of PSP compared to a healthy control group and in PSP phenotypes using SD-OCT. The additional objective was to verify the relationship between retinal layer thickness and clinical variables in PSP.
Patients and methods
Participants
Thirty-two patients diagnosed with PSP according to the Movement Disorder Society (MDS) criteria were invited to take part in the study and examined between June 2018 and December 2019 [1]. Detailed information on enrollment and application of the PSP diagnostic criteria to determine disease phenotype is available elsewhere [2,3,4,5]. Each patient contributed with one eye. Five patients were excluded for either incomplete data or confounding eye diseases. Thus, 27 PSP patients (27 eyes) were considered in the present analysis.
The severity of the disease was evaluated with the PSP rating scale (PSP-rs) total score and related subscores (mental, bulbar, ocular, limb, and gait), while cognitive abilities were rated with the MoCA and related subscores (visuospatial, executive, language, orientation, attention, and memory) [14, 15].
A group of 27 eyes from 27 sex-matched healthy controls (HC) with similar age and axial length, without diabetes, or other confounding eye diseases were enrolled (PSP:HC = 1:1). Healthy controls did not undergo formal neurological examination but had no history of any neurodegenerative disease.
Imaging protocol and image analysis
All participants underwent SD-OCT imaging with the Heidelberg SPECTRALIS (Heidelberg Engineering, Heidelberg, Germany) with a standard macular volume scan protocol and obtained the segmentation of the retinal layers using the instrument’s automatic algorithm. Poor quality images with a signal-to-noise score lower than 25 dB were excluded.
Using this system, 11 optical interfaces were obtained for the study of the 10 retinal layers [10]; using the standard Early Treatment Diabetic Retinopathy Study (ETDRS) grid, the thickness of the retinal layers at the circle centered on the fovea (1 mm in diameter), and the average of the 5 foveal and parafoveal zones (3 mm in diameter) were studied.
For the fovea (1 mm diameter), the values of the total thickness (total retina), photoreceptor layer, retinal pigment epithelium (RPE), outer nuclear layer (ONL), OPL, ONL/OPL ratio, and the IRL thickness were collected [16, 17]. This last value includes the sum of RNFL, the GCL, the IPL, and inner nuclear (INL) layers that are closely set together at the foveal center. For the parafoveal zone (3 mm diameter), however, the thickness value for these layers was also evaluated individually. Figure 1A shows the EDTRS grid and the 5 foveal and parafoveal zones; Fig. 1B outlines the segmentation of the retinal layers.
A ETDRS grid. A central circle at the fovea (diameter 1 mm). A + B + C + D + E = 5 central regions (3 mm diameter). Abbreviation: EDTRS: Early Treatment Diabetic Retinopathy Study. B Segmentation of the retinal layers using the instrument’s automatic algorithm. Abbreviations: GCL, ganglion cell layer; INL, inner nuclear layer; IPL, inner plexiform layer; IRL, inner retinal layer; ONL, outer nuclear layer; OPL, outer plexiform layer; RNFL, retinal nerve fiber layer; RPE, retinal pigment epithelium
The eyes of PSP patients and controls were evaluated with an IOL Master (5.4.4.0006; Carl Zeiss Meditec AG) to measure the axial length and to match the results. The mean of at least three measurements with the highest signal-to-noise ratio at least above 2 was considered.
Statistical analysis
After checking for normal distribution of data with the Kolmogorov–Smirnov test, parametric testing was used to compare the thickness measures of retinal layers between PSP and healthy controls. Then, the layers showing significant differences between groups were analyzed with the area under the receiver operating characteristics (ROC) to quantify their ability to discriminate between patients and controls.
The relationship between retinal layers and cognitive (MoCA total score and subscores) and motor (PSP-rs total score and subscores) measures was evaluated with Pearson’s correlation. Multiple comparisons were corrected with the Bonferroni test (p < 0.001).
Statistical analyses were performed with SPSS v.23 and a two-sided p < 0.05 was considered statistically significant.
Standard protocol approvals, registrations, and patient consent
This study was approved by the local ethics committee, and all participants were included upon signature of the written informed consent form.
Results
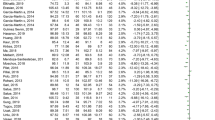
Demographic characteristics and axial length of enrolled PSP and HC are detailed in Table 1. Enrolled PSP had a disease duration of 2.41 ± 1.08 years. Seventeen patients (62.9%) presented PSP-RS, and 10 presented the other variant syndromes of PSP (vPSP) including 6 PSP with predominant parkinsonism and 4 PSP with progressive gait freezing.
Table 2 shows the central circle at the fovea (diameter 1 mm) and the average of the central 5 regions (diameter 3 mm) for PSP and HC. When considering the central 5 regions, PSP patients showed significant thinning of the IRL, OPL, IPL, and GCL compared to HC (Table 2). The ROC analysis for discriminating patients from controls found that the area under the curve (AUC) was 0.684 (95% confidence interval 0.536–0.831) for IRL, 0.698 (95% confidence interval 0.556–0.839) for OPL, 0.689 (95% confidence interval 0.689 to 0.834) for IPL and 0.655 (95% confidence interval 0.509–0.801) for GCL (Fig. 2). PSP-RS showed similar retinal thicknesses as vPSP (Table 3). PSP-RS and vPSP did not present any difference in terms of age, sex distribution, and axial length (data not shown).
In PSP, MoCA visuospatial subscore was positively correlated with IRL and total retinal thickness of the fovea (r = 0.565, p = 0.004 and r = 0.563, p = 0.004, respectively) and with IRL (r = 0.660, p < 0.001), OPL (r = 0.565, p = 0.004), INL (r = 0.702, p < 0.001), IPL (r = 0.556, p = 0.005), GCL (r = 0.496, p = 0.014), total retina thickness (r = 0.636, p < 0.001) of the 5 central regions. As for motor variables, photoreceptor of the fovea was negatively correlated with PSP-rs bulbar subscore (r = − 0.413, p = 0.036) and IRL and total retinal thickness of the 5 central regions with PSP-rs limb subscore (r = − 0.388, p = 0.045 and r = − 0.403, p = 0.037, respectively). Also, the photoreceptor of the 5 central regions was negatively correlated with PSP-rs bulbar subscore (r = − 0.538, p = 0.004) and IPL and GCL of the 5 central regions with PSP-rs gait subscore (r = − 0.438, p = 0.022 and r = − 0.493, p = 0.009, respectively). No other significant correlations were detected. The correlation between MoCA visuospatial subscore and IRL, INL, and total retina of the 5 central regions remained significant after correction for multiple comparisons (p < 0.001).
Discussion
Herein, we showed PSP is associated with the thinning of IRL, OPL, IPL, and GCL compared to healthy controls in all the five central regions, except in the foveal central circle. Such difference was present only when considering the average of the 5 central regions and not when considering the central circle at the fovea. The reduced representation of retinal layers in the foveal central circle, mainly concerning the IRL, may account for such findings.
Few studies investigated retinal layers’ thickness by SD-OCT in PSP patients showing a thinning of INL and ONL compared to other forms of parkinsonism [16, 17]. In contrast with our findings, Schneider et al. found thicker OPL in PSP patients [17]. Such discrepancy between our findings and previous data may be explained in part by differences in the segmentation method of the retinal layers. As such, while Albrecht et al. carried out a manual segmentation of the parafoveal retinal layers and Schneider et al. used a semiautomatic algorithm, in the present study, we adopted an automatic segmentation [16, 17]. More recently, Woo et al. found thinner peripapillary RNFL in 21 PSP compared to 22 HC [18]. As opposite to this study, ours included a 1:1 match between PSP and HC eyes also taking into account axial length [18].
Both in vivo and postmortem studies suggest a decreased number of ganglion cells and an RNFL thinning, and in general of the inner retina, in Alzheimer’s disease [19, 20]. On the other hand, scant data is available on retinal thickness in non-Alzheimer’s dementia. Recent evidence would support a selective thinning of the outer retina in patients affected by frontotemporal degeneration (FTD) clinical syndromes [10]. In detail, Kim et al. reported the outer retina thinning driven by the ONL thinning in 27 FTD patients, including 12 PSP, compared to healthy controls [10]. Contradicting previous findings, our study does not support this simplistic differential involvement of retinal layers according to the dementia type, i.e., Alzheimer’s disease associated with inner retina thinning and FTD with outer retina thinning [10]. Instead, our data would support a patchy involvement of retinal layers in PSP, involving both the inner (i.e., IRL) and outer (i.e., OPL) retina, more evident when considering the average of the 5 central regions than the central foveal circle alone.
Several reasons may account for such discrepancies with previous data [10]. First, our study is focused on PSP only and involves a larger number of patients (27 versus 12). Second, we compared retinal layer thicknesses between PSP and a group of healthy controls with similar age and sex distribution. But more importantly, our PSP and healthy controls showed comparable axial length, ensuring the reliability of retinal layers comparisons between groups. As a matter of fact, evidence demonstrates that axial length may influence the measurement of retinal and choroidal thickness [21, 22], and none of the previously published studies on this topic compared patients and controls according to these parameters. Finally, all our patients and healthy controls were Caucasian. On the contrary, Kim et al. included a group of healthy controls not matched for age, ethnicity, and axial length with FTD [10].
Our results were also supported by the ROC analysis, which demonstrated a fair diagnostic accuracy for both IRL, GCL, IPL, and OPL in discriminating between PSP and healthy controls (Fig. 2).
Using the immunoreactivity technique, previous studies showed tau protein accumulation in older individuals’ human retinal layers, such as RNFL, INL, IPL, and OPL [7, 8]. Considering that PSP is a neurodegenerative tauopathy and the RNFL, INL, and IPL layers are part of the IRL, we speculate that accumulation of tau protein in such retinal layers may cause the IRL, GCL, IPL, and OPL degeneration in PSP patients, with possible evolution in retinal thinning [6].
Similar to recent data [18], we failed to detect differences in retinal thickness between PSP phenotypes (PSP-RS vs vPSP) in any layer. Indeed, while IRL, GCL, IPL, and OPL proved able to differentiate PSP from healthy controls, none of the retinal thicknesses presented significant differences among MDS PSP subtypes (Table 3). The MDS PSP phenotypes were recently conceived based on an extensive review of the literature as well as the revision of the largest autopsy-confirmed case series reported so far [1]. In spite of being considered a window on brain changes, retinal thickness adds to the list of in vivo clinical and neuroimaging assessments not supporting the differentiation of the PSP phenotypes [2,3,4,5]. In such a scenario, there is a dearth of in vivo biomarkers supporting specific phenotypic attribution.
As for the correlation between retinal thickness and disease severity in PSP, we demonstrated a significant relationship between MoCA visuospatial subscore and IRL, INL, and the total retinal layer of the 5 central regions, which remained statistically significant after correcting for multiple comparisons. Retinal thickness has been associated with cognitive performances in tests requiring visual processing in other neurological conditions including multiple sclerosis [23]. Such association may have two possible explanations. First, greater retinal thinning may result in subclinical vision difficulties, which in turn affect the performance of cognitive testing requiring visual processing. Alternatively or complementary, greater retinal thinning may represent a marker of a more severe form of disease manifesting with poorer cognitive functions [23,24,25]. Since we missed to assess visual acuity and visual field, as well as perform neuroimaging studies in the present study, we cannot draw firm conclusions, and further studies are needed to clarify this aspect.
As for the relationship with motor scores, the correlation between PSP-rs bulbar, limb, and gait subscores with retinal layers lost significance after correction for multiple comparisons. Indeed, motor impairment in PSP is associated with a wide range of determinants possibly explaining the weaker relationship with retinal thickness.
In comparison with previous data [10,11,12,13], the strengths of the present study include a larger sample size of the PSP cohort, the comparison of PSP with a control group with similar age, sex and axial length, and the use of disease-specific clinical assessments (i.e., the PSP rating scale and the MoCA).
In conclusion, we demonstrated PSP patients disclose thinner IRL, GCL, IPL, and OPL compared to sex-matched healthy controls with similar age and axial length. Furthermore, we found a significant correlation between visuospatial abilities and retinal layers suggesting the existence of a mutual relationship between posterior cognitive function and retinal structure.
Change history
17 July 2022
Missing Open Access funding information has been added in the Funding Note.
Abbreviations
- MDS:
-
Movement Disorder Society
- MoCA:
-
Montreal Cognitive Assessment battery
- OCT:
-
Optical coherence tomography
- PSP:
-
Progressive supranuclear palsy
- PSP-rs:
-
Progressive supranuclear palsy rating scale
- PSP-RS:
-
Progressive supranuclear palsy with Richardson’s syndrome
- RNFL:
-
Retinal nerve fiber layer
- ROC:
-
Receiver operating characteristics
- vPSP:
-
The other variant syndromes of progressive supranuclear palsy
References
Hoglinger GH, Respondek G, Stamelou M et al (2017) Clinical diagnosis of progressive supranuclear palsy: the Movement Disorder Society criteria. Mov Disord 32:853–864
Picillo M, Tepedino MF, Abate F et al (2020) Midbrain MRI assessments in progressive supranuclear palsy subtypes. J Neurol Neurosurg Psychiatry 91(1):98–103
Picillo M, Erro R, Cuoco S, PSP Salerno Study Group et al (2018) MDS PSP criteria in real-life clinical setting: motor and cognitive characterization of subtypes. Mov Disord 33(8):1361–1365
Picillo M, Cuoco S, Tepedino MF et al (2019) Motor, cognitive and behavioral differences in MDS PSP phenotypes. J Neurol 266(7):1727–1735
Picillo M, Cuoco S, Carotenuto I et al (2019) Clinical use of SAND battery to evaluate language in patients with progressive supranuclear palsy. PLoS One 14(10):e0223621
Litvan I, Agid Y, Calne D et al (1996) Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome). Report of the NINDS-SPSP International Workshop. Neurology 47:1–9
Schon C, Hoffman NA, Ochs SM et al (2012) Long-term in vivo imaging of fibrillar tau in the retina of P301S transgenic mice. Plos One 7(12):e53547
Löffler KU, Edward DP, Tso MO (1995) Immunoreactivity against tau, amyloid precursor protein, and beta-amyloid in the human retina. Invest Ophthalmol Vis Sci 36:24–31
Leger F, Fernagut PO, Canron MH et al (2011) Protein aggregation in the aging retina. J Neuropathol Exp Neurol 70:63–68
Kim BJ, Irwin DJ, Song D et al (2017) Optical coherence tomography identifies outer retina thinning in frontotemporal degeneration. Neurology 89:1604–1611
Stemplewitz B, Kromer R, Vettorazzi E et al (2017) Retinal degeneration in progressive supranuclear palsy measured by optical coherence tomography and scanning laser polarimetry. Sci Rep 7:5357
Gulmez Sevim D, Unlu M, Gultekin M et al (2018) Evaluation of retinal changes in progressive supranuclear palsy and Parkinson disease. J Neuroophtalmol 38(2):151–155
Kim BJ, Grossman M, Song D et al (2019) Persistent and progressive outer retina thinning in frontotemporal degeneration. Front Neurosci 13:298
Golbe LI, Ohman-Strickland PA (2007) A clinical rating scale for progressive supranuclear palsy. Brain 130(Pt 6):1552–1565
Santangelo G, Cuoco S, Pellecchia MT, Erro R, Barone P, Picillo M (2018) Comparative cognitive and neuropsychiatric profiles between Parkinson’s disease, multiple system atrophy and progressive supranuclear palsy. J Neurol 265(11):2602–2613
Albrecht P, Müller AK, Südmeyer M et al (2012) Optical coherence tomography in parkinsonian syndromes. PLoS One 7(4):e34891
Schneider M, Müller HP, Lauda F et al (2014) Retinal single-layer analysis in parkinsonian syndromes: an optical coherence tomography study. J Neural Transm (Vienna) 121(1):41–47
Woo KA, Shin JY, Kim H et al (2021) Peripapillary retinal fiber layer thinning in patients with progressive supranuclear palsy. J Neurol. https://doi.org/10.1007/s00415-02110936-5.
Coppola G, Di Renzo A, Ziccardi L et al (2015) Optical coherence tomography in Alzheimer’s disease: a meta-analysis. Plos One 10:e0134750
Cheung CY, Chan VTT, Mok VC, Chen C, Wong TY (2019) Potential retinal biomarkers for dementia: what is new? Curr Opin Neurol 32:82–91
De Bernardo M, Salerno G, Gioia M et al (2021) Intraocular pressure and choroidal thickness postural changes in multiple system atrophy and Parkinson’s disease. Sci Rep 11(1):8936
De Bernardo M, Salerno G, Cornetta P, Rosa N (2018) Axial length shortening after cataract surgery: new approach to solve the question. Transl Vis Sci Technol 7(6):34
Jakimoski D, Benedict RHB, Weinstock-Guttman B et al (2021) Visual deficits and cognitive assessment of multiple sclerosis: confounder, correlate or both? J Neurol 268(7):2578–2588
Armstrong R, Kergoat H (2015) Oculovisual changes and clinical considerations affecting older patients with dementia. Ophthalmic Physiol Opt 35(4):352–376
Pietroboni AM, Dell’Arti L, Caprioli M et al (2019) The loss of macular ganglion cells begins from the early stages of disease and correlates with brain atrophy in multiple sclerosis patients. Mult Scler 25(1):31–38
Acknowledgements
This project was conducted with the support of the University of Salerno, FARB2019. We are grateful to the patients who took part in the present study.
Funding
Open access funding provided by Università degli Studi di Salerno within the CRUI-CARE Agreement. This project was conducted with the support of the University of Salerno, FARB2019.
Author information
Authors and Affiliations
Contributions
The statistical analysis was conducted by Marina Picillo, MD, PhD, University of Salerno, Italy.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
This study was approved by the local ethics committee, and all participants were included upon signature of the written informed consent form.
Conflict of interest
MP is supported by the Michael J Fox Foundation for Parkinson’s research; PB received consultancies as a member of the advisory board for Zambon, Lundbeck, UCB, Chiesi, Abbvie, and Acorda; RE received consultancies from Zambon and honoraria from TEVA.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Picillo, M., Salerno, G., Tepedino, M.F. et al. Retinal thinning in progressive supranuclear palsy: differences with healthy controls and correlation with clinical variables. Neurol Sci 43, 4803–4809 (2022). https://doi.org/10.1007/s10072-022-06061-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-06061-4