Abstract
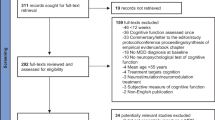
The assessment of cognition is an important part of major depressive disorder (MDD) evaluation and a crucial issue is the physicians’ perception of cognitive dysfunction in MDD that remains nowadays a little known matter. The present study aims at investigating the understanding of neurologists’ perception about cognitive dysfunction in MDD. An on-line survey addressed to 85 Italian neurologists in the period between May and June 2015 was performed. The questionnaire comprised three sections: the first section collecting information on neurologists’ socio-demographic profile, the second investigating cognitive symptoms relevance in relation with different aspects and the third one explicitly focusing on cognitive symptoms in MDD. Cognitive symptoms are considered most significant among DSM-5 symptoms to define the presence of a Major Depressive Episode in a MDD, to improve antidepressant therapy adherence, patients’ functionality and concurrent neurological condition, once resolved. Furthermore, an incongruity came to light from this survey: the neurologists considered cognitive symptoms a not relevant aspect to choose the antidepressant treatment in comparison with the other DSM-5 symptoms on one side, but they declared the opposite in the third part of the questionnaire focused on cognitive symptoms. Cognitive symptoms appeared to be a relevant aspect in MDD and neurologists have a clear understanding of this issue. Nevertheless, the discrepancy between neurologists’ perception on cognitive symptoms and the antidepressant treatment highlights the feeling of an unmet need that could be filled increasing the awareness of existing drugs with pro-cognitive effects.


Similar content being viewed by others
References
Veiel HOF (1997) A preliminary profile of neuropsychological deficits associated with major depression. J Clin Exp Neuropsychol 19:587–603
Elliot R (2003) Executive functions and their disorders. Br Med Bull 65:45–59
Landrø NI, Stiles TC, Sletvold H (2003) Neuropsychological function in nonpsychotic unipolar major depression. Neuropsychiatry Neuropsychol Behav Neurol 14:233–240
Sobin C, Sackeim HA (1997) Psychomotor symptoms of depression. Am J Psychiatry 154:4–17
Butters MA, Whyte EM, Nebes RD, Begley AE, Dew MA, Mulsant BH, Zmuda MD, Bhalla R, Meltzer CC, Pollock BG, Reynolds CF 3rd, Becker JT (2004) The nature and determinants of neuropsychological functioning in late-life depression. Arch Gen Psychiatry 61:587–595
Greer TL, Kurian BT, Trivedi MH (2010) Defining and measuring functional recovery from depression. CNS Drugs 24:267–284
Baune BT, Miller R, McAfoose J, Johnson M, Quirk F, Mitchell D (2010) The role of cognitive impairment in general functioning in major depression. Psychiatry Res 176:183–189
Jaeger J, Berns S, Uzelac S, Davis-Conway S (2006) Neurocognitive deficits and disability in major depressive disorder. Psychiatry Res 145:39–48
Greer TL, Sunderajan P, Grannemann BD, Kurian BT, Trivedi MH (2014) Does duloxetine improve cognitive function independently of its antidepressant effect in patients with major depressive disorder and subjective reports of cognitive dysfunction? Depress Res Treat 14:627863. doi:10.1155/2014/627863
Kennedy B, Lin Y, Schwab J (2012) Work, social, and family disabilities of subjects with anxiety and depression. South Med J 95:1424–1427
Srisurapanont M, Hong JP, Tian-Mei S, Hatim A, Liu CY, Udomratn P et al (2013) Clinical features of depression in Asia: results of a large prospective, cross-sectional study. Asia Pac Psychiatry 5:259–267
Tweed D (1993) Depression-related impairment: estimating concurrent and lingering effects. Psychol Med 23:373
Kennedy N, Paykel E (2004) Residual symptoms at remission from depression: impact on long-term outcome. J Affect Disord 80:135–144
Conradi H, Ormel J, de Jonge P (2011) Presence of individual (residual) symptoms during depressive episodes and periods of remission: a 3-year prospective study. Psychol Med 41:1165–1174
Saltiel PF, Silvershein D (2015) Major depressive disorder: mechanism-based prescribing for personalized medicine. Neuropsychiatr Dis Treat 11:875–888
Conradi HJ, Ormel J, de Jonge P (2012) Symptom profiles of DSM-IV-defined remission, recovery, relapse, and recurrence of depression: the role of the core symptoms. Depress Anxiety 29:638–645
McKnight PE, Kashdan TB (2009) The importance of functional impairment to mental health outcomes: a case for reassessing our goals in depression treatment research. Clin Psychol Rev 29:243–259
McClintock SM, Husain MM, Wisniewski SR, Nierenberg AA, Stewart JW, Trivedi MH, Cook I, Morris D, Warden D, Rush AJ (2011) Residual symptoms in depressed outpatients who respond by 50% but do not remit to antidepressant medication. J Clin Psychopharmacol 31:180–186
McIntyre RS, Cha DS, Soczynska JK, Woldeyohannes HO, Gallaugher LA, Kudlow P et al (2013) Cognitive deficits and functional outcomes in major depressive disorder: determinants, substrates, and treatment interventions. Depress Anxiety 30:515–527
World Health Organization and Alzheimer’s Disease International. Dementia: a public health priority (2012)
Kang H, Zhao F, You L, Giorgetta C, Sarkhel S, Prakash R (2014) Pseudo-dementia: a neuropsychological review. Ann Indian Acad Neurol 17:147–154
El Hammi E, Samp J, Rémuzat C, Auray JP, Lamure M, Aballéa S, Kooli A, Akhras K, Toumi M (2014) Difference of perceptions and evaluation of cognitive dysfunction in major depressive disorder patients across psychiatrists internationally. Ther Adv Psychopharmacol 4:22–29
Albert U, Brugnoli R, Caraci F, Dell’Osso B, Di Sciascio G, Tortorella A, Vampini C, Cataldo N, Pegoraro V (2015) Italian psychiatrists’ perception on cognitive symptoms in major depressive disorder. Int J Psychiatry Clin Pract 2:1–8
Baune BT, Renger L (2014) Pharmacological and non-pharmacological interventions to improve cognitive dysfunction and functional ability in clinical depression–a systematic review. Psychiatry Res 219:25–50
Dell’Osso B, Ketter TA (2013) Use of adjunctive stimulants in adult bipolar depression. Int J Neuropsychopharmacol 16:55–68
Dias VV, Balanzá-Martinez V, Soeiro-de-Souza MG, Moreno RA, Figueira ML, Machado-Vieira R, Vieta E (2012) Pharmacological approaches in bipolar disorders and the impact on cognition: a critical overview. Acta Psychiatr Scand 126:315–31
Katona CL, Katona CP (2014) New generation multi-modal antidepressants: focus on vortioxetine for major depressive disorder. Neuropsychiatr Dis Treat 10:349–354
McIntyre RS, Lophaven S, Olsen CK (2014) A randomized, double-blind, placebo-controlled study of vortioxetine on cognitive function in depressed adults. Int J Neuropsychopharmacol 17:1557–1567
Mahableshwarkar AR, Jacobsen PL, Serenko M, Chen Y, Trivedi MH (2015) A randomized, double-blind, placebo-controlled study of the efficacy and safety of 2 doses of vortioxetine in adults with major depressive disorder. J Clin Psychiatry 76:583–591
Cunningham CT, Quan H, Hemmelgarn B, Noseworthy T, Beck CA, Dixon E, Samuel S, Ghali WA, Sykes LL, Jetté N (2015) Exploring physician specialist response rates to web-based surveys. BMC Med Res Methodol 15:32
Acknowledgments
Claudio Ripellino and Nazarena Cataldo were responsible for survey design, data analyses and writing of the manuscript. Giuseppe Neri, Carlo Serrati and Paolo Zolo were responsible for clinical validation of the study and review of the manuscript. All authors read and approved the final manuscript. A courtesy review was also performed by Lundbeck S.p.A.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This survey was supported by an unrestricted grant from Lundbeck S.p.A., which was not responsible for the content of this survey, data analysis, data interpretation, medical writing or editorial assistance. Giuseppe Neri, Carlo Serrati and Paolo Zolo have received honoraria from IMS Health Information Solutions Italy srl and Claudio Ripellino and Nazarena Cataldo are employees of IMS Health Information Solutions Italy srl. The authors have indicated that they have no other conflict of interest with regard to the content of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Neri, G., Serrati, C., Zolo, P. et al. Italian neurologists’ perception on cognitive symptoms in major depressive disorder. Neurol Sci 37, 1437–1442 (2016). https://doi.org/10.1007/s10072-016-2601-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-016-2601-2