Abstract
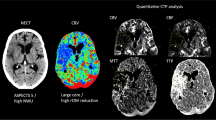
We investigated the practical clinical utility of the CT perfusion (CTP) cerebral blood volume (CBV) parameter for differentiating salvageable from non-salvageable tissue in acute ischemic stroke (AIS). Fifty-five patients with AIS were imaged within 6 h from onset using CTP. Admission CBV defect (CBVD) volume was outlined using previously established gray and white matter CBV thresholds for infarct core. Admission cerebral blood flow (CBF) hypoperfusion and CBF/CBV mismatch were visually evaluated. Truncation of the ischemic time–density curve (ITDC) and hypervolemia status at admission, recanalization at 24-h CT angiography, hemorrhagic transformation (HT) at 24 h and/or 7-day non-contrast CT (NCCT), final infarct volume as indicated by 3-month NCCT defect (NCCTD) and 3-month modified Rankin Score were determined. Patients with recanalization and no truncation had the highest correlation (R = 0.81) and regression slope (0.80) between CBVD and NCCTD. Regression slopes were close to zero for patients with admission hypervolemia with/without recanalization. Hypervolemia underestimated (p = 0.02), while recanalization and ITDC truncation overestimated (p = 0.03) the NCCTD. Among patients with confirmed recanalization at 24 h, 38 % patients had an admission CBF/CBV mismatch within normal appearing areas on respective NCCT. 83 % of these patients developed infarction in admission hypervolemic CBF/CBV mismatch tissue. A reduction in CBV is a valuable predictor of infarct core when the acquisition of ITDC data is complete and hypervolemia is absent within the tissue destined to infarct. Raised or normal CBV is not always indicative of salvageable tissue, contrary to the current definition of penumbra.
Similar content being viewed by others
References
Donnan GA, Fisher M, Macleod M, Davis SM (2008) Stroke. Lancet 371:1612–1623
Wahlgren N, Ahmed N, Dávalos A, Hacke W, Millán M, Muir K, Roine RO, Toni D, Lees KR, SITS investigators (2008) Thrombolysis with alteplase 3-4.5 h after acute ischaemic stroke (SITS-ISTR): an observational study. Lancet 372:1303–1309
Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, Larrue V, Lees KR, Medeghri Z, Machnig T, Schneider D, von Kummer R, Wahlgren N, Toni D, Investigators ECASS (2008) Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 359:1317–1329
Schumacher HC, Bateman BT, Boden-Albala B, Berman MF, Mohr JP, Sacco RL, Pile-Spellman J (2007) Use of thrombolysis in acute ischemic stroke: analysis of the nationwide inpatient sample 1999 to 2004. Ann Emerg Med 50:99–107
Bivard A, Parsons M (2012) ASPECTaSaurus (a dinosaur)? Int J Stroke 7:564
Wardlaw J, Dorman P, Lewis S, Sandercock PA (1999) Can stroke physicians and neuroradiologists identify signs of early cerebral infarction on CT? J Neurol Neurosurg Psychiatry 67:651–653
Puetz V, Dzialowski I, Hill MD, Demchuk AM (2009) The Alberta Stroke Program Early CT Score in clinical practice: what have we learned? Int J Stroke 4:354–364
Turk AS, Nyberg EM, Chaudry MI, Turner RD, Magarik JA, Nicholas JS, Holmstedt CA, Chalela JA, Hays A, Lazaridis C, Chimowitz MI, Turan TN, Adams RJ, Jauch EC (2013) Utilization of CT perfusion patient selection for mechanical thrombectomy irrespective of time: a comparison of functional outcomes and complications. J Neurointerv Surg 5:518–522
Turk A, Magarik JA, Chaudry I, Turner RD, Nicholas J, Holmstedt CA, Chalela J, Hays A, Lazaridis C, Jauch E, Chimowitz M, Turan T, Adams R (2012) CT perfusion-guided patient selection for endovascular treatment of acute ischemic stroke is safe and effective. J Neurointerv Surg 4:261–265
Kamalian S, Kamalian S, Konstas AA, Maas MB, Payabvash S, Pomerantz SR, Schaefer PW, Furie KL, González RG, Lev MH (2012) CT perfusion mean transit time maps optimally distinguish benign oligemia from true “at-risk” ischemic penumbra, but thresholds vary by postprocessing technique. Am J Neuroradiol 33:545–549
García-Bermejo P, Calleja AI, Pérez-Fernández S, Cortijo E, del Monte JM, García-Porrero M, Fe Muñoz M, Fernández-Herranz R, Arenillas JF (2012) Perfusion computed tomography-guided intravenous thrombolysis for acute ischemic stroke beyond 4.5 hours: a case-control study. Cerebrovasc Dis 34:31–37
Kamalian S, Kamalian S, Maas MB, Goldmacher GV, Payabvash S, Akbar A, Schaefer PW, Furie KL, Gonzalez RG, Lev MH (2011) CT cerebral blood flow maps optimally correlate with admission diffusion-weighted imaging in acute stroke but thresholds vary by postprocessing platform. Stroke 42:1923–1928
Campbell BC, Christensen S, Levi CR, Desmond PM, Donnan GA, Davis SM, Parsons MW (2011) Cerebral blood flow is the optimal CT perfusion parameter for assessing infarct core. Stroke 42:3435–3440
Murphy BD, Fox AJ, Lee DH, Sahlas DJ, Black SE, Hogan MJ, Coutts SB, Demchuk AM, Goyal M, Aviv RI, Symons S, Gulka IB, Beletsky V, Pelz D, Chan RK, Lee TY (2008) White matter thresholds for ischemic penumbra and infarct core in patients with acute stroke: CT perfusion study. Radiology 247:818–825
Hatazawa J, Shimosegawa E, Toyoshima H, Ardekani BA, Suzuki A, Okudera T, Miura Y (1999) Cerebral blood volume in acute brain infarction: a combined study with dynamic susceptibility contrast MRI and 99mTc-HMPAO-SPECT. Stroke 30:800–806
Murphy BD, Fox AJ, Lee DH, Sahlas DJ, Black SE, Hogan MJ, Coutts SB, Demchuk AM, Goyal M, Aviv RI, Symons S, Gulka IB, Beletsky V, Pelz D, Hachinski V, Chan R, Lee TY (2006) Identification of penumbra and infarct in acute ischemic stroke using computed tomography perfusion-derived blood flow and blood volume measurements. Stroke 37:1771–1777
Deipolyi AR, Wu O, Macklin EA, Schaefer PW, Schwamm LH, Gilberto Gonzalez R, Copen WA (2012) Reliability of cerebral blood volume maps as a substitute for diffusion-weighted imaging in acute ischemic stroke. J Magn Reson Imaging 36:1083–1087
Labeyrie MA, Turc G, Hess A, Hervo P, Mas JL, Meder JF, Baron JC, Touzé E, Oppenheim C (2012) Diffusion lesion reversal after thrombolysis: a MR correlate of early neurological improvement. Stroke 43:2986–2991
d’Esterre CD, Fainardi E, Aviv RI, Lee TY (2012) Improving acute stroke management with computed tomography perfusion: a review of imaging basics and applications. Transl Stroke Res 3:205–220
d’Esterre CD, Aviv RI, Lee TY (2012) The evolution of the cerebral blood volume abnormality in patients with ischemic stroke: a CT perfusion study. Acta Radiol 53:461–467
TIMI Study Group (1985) The Thrombolysis in Myocardial Infarction (TIMI) trial. Phase I findings. N Engl J Med 312:932–936
Larrue V, von Kummer RR, Müller A, Bluhmki E (2001) Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator: a secondary analysis of the European-Australasian Acute Stroke Study (ECASS II). Stroke 32:438–441
Bland JM, Altman DG (1999) Measuring agreement in method comparison studies. Stat Methods Med Res 8:135–160
Konstas AA, Goldmakher GV, Lee TY, Lev MH (2009) Theoretic basis and technical implementations of CT perfusion in acute ischemic stroke, part 1: theoretic basis. Am J Neuroradiol 30:662–668
Dani KA, Thomas RG, Chappell FM, Shuler K, MacLeod MJ, Muir KW, Wardlaw JM, Translational Medicine Research Collaboration Multicentre Acute Stroke Imaging Study (2011) Computed tomography and magnetic resonance perfusion imaging in ischemic stroke: definitions and thresholds. Ann Neurol 70:384–401
Bivard A, Spratt N, Levi C, Parsons M (2011) Perfusion computer tomography: imaging and clinical validation in acute ischaemic stroke. Brain 134:3408–3416
Cortijo E, Calleja AI, García-Bermejo P, Mulero P, Pérez-Fernández S, Reyes J, Muñoz MF, Martínez-Galdámez M, Arenillas JF (2014) Relative cerebral blood volume as a marker of durable tissue-at-risk viability in hyperacute ischemic stroke. Stroke 45:113–118
Marchal G, Furlan M, Beaudouin V, Rioux P, Hauttement JL, Serrati C, de la Sayette V, Le Doze F, Viader F, Derlon JM, Baron JC (1996) Early spontaneous hyperperfusion after stroke. A marker of favourable tissue outcome? Brain 119:409–419
Acknowledgments
This work has been supported by Italian National Health System- Research Program entitled “Nuove conoscenze e problematiche assistenziali nell’ictus cerebrale: un Programma Strategico di Ricerca e Sviluppo” ex art. 12-12bis/D.Lgs n. 502/92, PG/2007/0293184. The authors would also like to thank the Canadian Stroke Network and European Stroke Network, Canadian Institutes of Health Research, Ontario Research Fund and GE Healthcare for partial support of this study.
Conflict of interest
Ting-Yim Lee licenses CT Perfusion software to and receives funding from GE Healthcare.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
d’Esterre, C.D., Roversi, G., Padroni, M. et al. CT perfusion cerebral blood volume does not always predict infarct core in acute ischemic stroke. Neurol Sci 36, 1777–1783 (2015). https://doi.org/10.1007/s10072-015-2244-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-015-2244-8