Abstract
Background
There is little robust data about the cardiovascular safety of hydroxychloroquine in patients with rheumatoid arthritis (RA), who often have cardiovascular comorbidities. We examined the association between use of hydroxychloroquine (HCQ) in patients with RA and major adverse cardiovascular events (MACE).
Methods
In a retrospective cohort of Medicare beneficiaries aged ≥ 65 years with RA, we identified patients who initiated HCQ (users) and who did not initiate HCQ (non-users) between January 2015-June 2017. Each HCQ user was matched to 2 non-users of HCQ using propensity score derived from patient baseline characteristics. The primary outcome was the occurrence of MACE, defined as acute admissions for stroke, myocardial infarction, or heart failure. Secondary outcomes included all-cause mortality and the composite of MACE and all-cause mortality. Cox proportional hazards model was used to compare outcomes between HCQ users to non-users.
Results
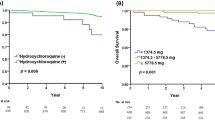
The study included 2380 RA patients with incident HCQ use and matched 4633 HCQ non-users over the study period. The mean follow-up duration was 1.67 and 1.63 years in HCQ non-users and users, respectively. In multivariable models, use of HCQ was not associated with the risk of MACE (hazard ratio 1.1; 95% CI: 0.832–1.33). However, use of HCQ was associated with a lower risk of all-cause mortality (HR: 0.54; 95% CI: 0.45–0.64) and the composite of all-cause mortality and MACE (HR 0.67; 95% CI: 0.58–0.78).
Conclusion
HCQ use was independently associated with a lower risk of mortality in older adults with RA but not with incidence of MACE events.
Key Points • Using an incident user design (to avoid the biases of a prevalent user design) and a population-based approach, we examined the effect of hydroxychloroquine (HCQ) on the risk of major cardiovascular events (MACE) in older patients with RA. • We did not find an association between HCQ use and incident MACE. We did, however, find a significant association with the composite outcome (MACE and all-cause mortality) driven by a significant reduction in all-cause mortality with HCQ use. |

Similar content being viewed by others
References
Johnson NB, Hayes LD, Brown K (2014) CDC National Health Report: leading causes of morbidity and mortality and associated behavioral risk and protective factors–United States, 2005–2013. MMWR Suppl 63:3–27
Gorina Y, Hoyert D, Lentzner H, Goulding M (2005) Trends in causes of death among older persons in the United States. Aging Trends (6):1–12. https://stacks.cdc.gov/view/cdc/6867
Salmon JE, Roman MJ (2008) Subclinical atherosclerosis in rheumatoid arthritis and systemic lupus erythematosus. Am J Med 121:S3–S8. https://doi.org/10.1016/j.amjmed.2008.06.010
Cavagna L, Boffini N, Cagnotto G et al (2012) Atherosclerosis and rheumatoid arthritis: more than a simple association. Mediators Inflamm 2012:147354. https://doi.org/10.1155/2012/147354
del Ricón ID, Williams K, Stern MP et al (2001) High incidence of cardiovascular events in a rheumatoid arthritis cohort not explained by traditional cardiac risk factors. Arthritis Rheum 44:2737–2745
van Halm VP, Peters MJL, Voskuyl AE et al (2009) Rheumatoid arthritis versus diabetes as a risk factor for cardiovascular disease: a cross-sectional study, the CARRE Investigation. Ann Rheum Dis 68:1395–1400. https://doi.org/10.1136/ard.2008.094151
Bili A, Sartorius JA, Kirchner HL (2011) Hydroxychloroquine use and decreased risk of diabetes in rheumatoid arthritis patients. J Clin Rheumatol 17:115–120
Qiao X, Zhou ZC, Niu R (2019) Hydroxychloroquine improves obesity-associated insulin resistance and hepatic steatosis by regulating lipid metabolism. Front Pharmacol 10. https://doi.org/10.3389/fphar.2019.00855
Morris SJ, Wasko MC, Antohe JL (2011) Hydroxychloroquine use associated with improvement in lipid profiles in rheumatoid arthritis patients. Arthritis Care Res 63:530–534
Achuthan S, Ahluwalia J, Shafiq N (2015) Hydroxychloroquine’s efficacy as an antiplatelet agent study in healthy volunteers: a proof of concept study. J Cardiovasc Pharmacol Ther 20:174–180
Kato E, Sawada T, Tahara K (2017) The age at onset of rheumatoid arthritis is increasing in Japan: a nationwide database study. Int J Rheum Dis 20:839–845
Kobak S, Bes C (2018) An autumn tale: geriatric rheumatoid arthritis. Ther Adv Musculoskelet Dis 10:3–11
Heart Disease and Stroke Statistics—2021 Update | Circulation. https://www.ahajournals.org/doi/10.1161/CIR.0000000000000950?cookieSet=1. Accessed 12 Dec 2022
Cannata F, Pinto G, Chiarito M et al (2023) Long-term prognostic impact of subclinical myocardial dysfunction in patients recovered from COVID-19. Echocardiography. https://doi.org/10.1111/echo.15575
Bonnesen K, Pedersen L, Ehrenstein V (2023) Impact of lifestyle and socioeconomic position on the association between non-steroidal anti-inflammatory drug use and major adverse cardiovascular events: a case-crossover study. Drug Saf. https://doi.org/10.1007/s40264-023-01298-0
Tsai W-C, Ou T-T, Yen J-H et al (2015) Long term frequent use of non-steroidal anti-inflammatory drugs might protect patients with ankylosing Spondylitis from cardiovascular diseases: a nationwide case control study. PLoS One 10:0126347. https://doi.org/10.1371/journal.pone.0126347
Wu M-Z, Chen Y, Au W-K, Chan D, Sit K-Y, Ho K-L, Ho L-M, Lam Y-M, Lau C-P, Chan T-M, Tse H-F, Yiu K-H (2018) Predictive value of acute kidney injury for major adverse cardiovascular events following Tricuspid annuloplasty: a comparison of three consensus criteria. J Cardiol 72(3):247–254. https://doi.org/10.1016/j.jjcc.2018.01.018
McCormick N, Bhole V, Lacaille D, Avina-Zubieta J (2015) Validity of diagnostic codes for acute stroke in administrative databases: a systematic review. PLoS One 10:135834. https://doi.org/10.1371/journal.pone.0135834
Metcalfe A, Neudam A, Forde S (2013) Case definitions for acute myocardial infarction in administrative databases and their impact on in-hospital mortality rates. Health Serv Res 48:290–318
Bates BA, Akhabue E, Nahass MM et al (2023) Validity of international classification of diseases (ICD)-10 diagnosis codes for identification of acute heart failure hospitalization and heart failure with reduced versus preserved ejection fraction in a national medicare sample. Circ Cardiovasc Qual Outcomes 16:009078. https://doi.org/10.1161/CIRCOUTCOMES.122.009078
Quan H, Sundararajan V, Halfon P et al (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43:1130–1139. https://doi.org/10.1097/01.mlr.0000182534.19832.83
Austin PC (2009) Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28:3083–3107. https://doi.org/10.1002/sim.3697
Yang L, Tao J, Tang X (2012) Prevalence and correlation of conventional and lupus-specific risk factors for cardiovascular disease in Chinese systemic lupus erythematosus patients. J Eur Acad Dermatol Venereol 26:95–101
Halm VP, Nurmohamed MT, Twisk JWR et al (2006) Disease-modifying antirheumatic drugs are associated with a reduced risk for cardiovascular disease in patients with rheumatoid arthritis: a case control study. Arthritis Res Ther 8:R151. https://doi.org/10.1186/ar2045
Sharma TS, Wasko MC, Tang X (2016) Hydroxychloroquine use is associated with decreased incident cardiovascular events in rheumatoid arthritis patients. J Am Heart Assoc 5(1):e002867. https://doi.org/10.1161/JAHA.115.002867
Roman MJ, Shanker BA, Davis A (2003) Prevalence and correlates of accelerated atherosclerosis in systemic lupus erythematosus. N Engl J Med 349:2399–2406. https://doi.org/10.1056/NEJMoa035471
Pons-Estel GJ, Gonzalez LA, Zhang J (2009) Predictors of cardiovascular damage in patients with systemic lupus erythematosus: data from LUMINA (LXVIII), a multiethnic US cohort. Rheumatology (Oxford) 48:817–22
Nikpour M, Urowitz MB, Ibanez D et al (2011) Importance of cumulative exposure to elevated cholesterol and blood pressure in development of atherosclerotic coronary artery disease in systemic lupus erythematosus: a prospective proof-of-concept cohort study. Arthritis Res Ther 13:R156
Magder LS, Petri M (2012) Incidence of and risk factors for adverse cardiovascular events among patients with systemic lupus erythematosus. Am J Epidemiol 176:708–719
Li C, Wang XR, Ji HJ (2017) Cardiovascular disease in rheumatoid arthritis: medications and risk factors in China. Clin Rheumatol 36:1023–1029
De Leeuw K, Freire B, Smit AJ et al (2006) Traditional and non-traditional risk factors contribute to the development of accelerated atherosclerosis in patients with systemic lupus erythematosus. Lupus 15:675–682
Hsu CY, Lin YS, Su YJ (2017) Effect of long-term hydroxychloroquine on vascular events in patients with systemic lupus erythematosus: a database prospective cohort study. Rheumatology (Oxford) 56:2212–2221
Gustafsson J, Gunnarsson I, Börjesson O (2009) Predictors of the first cardiovascular event in patients with systemic lupus erythematosus - a prospective cohort study. Arthritis Res Ther 11:R186
Fasano S, Margiotta DP, Navarini L (2017) Primary prevention of cardiovascular disease in patients with systemic lupus erythematosus: case series and literature review. Lupus 26:1463–1472
Liu D, Li X, Zhang Y (2018) Chloroquine and hydroxychloroquine are associated with reduced cardiovascular risk: a systematic review and meta-analysis. Drug Des Devel Ther 12:1685–1695
Rempenault C, Combe B, Barnetche T et al (2018) Metabolic and cardiovascular benefits of hydroxychloroquine in patients with rheumatoid arthritis: a systematic review and meta-analysis. Ann Rheum Dis 77:98–103. https://doi.org/10.1136/annrheumdis-2017-211836
Jorge A, Lu N, Choi H et al (2021) Hydroxychloroquine use and cardiovascular events among patients with systemic lupus erythematosus and rheumatoid arthritis. Arthritis Care Res (Hoboken). https://doi.org/10.1002/acr.24850
D’Andrea E, Desai RJ, He M et al (2022) Cardiovascular risks of hydroxychloroquine vs methotrexate in patients with rheumatoid arthritis. J Am Coll Cardiol 80:36–46. https://doi.org/10.1016/j.jacc.2022.04.039
Soeltoft K, Hallas J, Wasko MCM et al (2018) OP0191 All-cause mortality and cardiovascular death in hydroxychloroquine users in rheumatoid arthritis patients - a population based danish cohort study. Ann Rheum Dis 77:144–145
Faselis C, Zeng-Treitler Q, Cheng Y Cardiovascular safety of hydroxychloroquine in US veterans with rheumatoid arthritis. Arthritis &
Alarcon GS, McGwin G, Bertoli AM (2007) Effect of hydroxychloroquine on the survival of patients with systemic lupus erythematosus: data from LUMINA, a multiethnic US cohort (LUMINA L. Ann Rheum Dis 66:1168–1172
Shinjo SK, Bonfa E, Wojdyla D (2010) Antimalarial treatment may have a time-dependent effect on lupus survival: data from a multinational Latin American inception cohort. Arthritis Rheum 62:855–862
Jorge A, McCormick N, Lu N (2021) Hydroxychloroquine and mortality among patients with systemic lupus erythematosus in the general population. Arthritis Care Res 73:1219–1223
Kaiser R, Cleveland CM, Criswell LA (2009) Risk and protective factors for thrombosis in systemic lupus erythematosus: results from a large, multi-ethnic cohort. Ann Rheum Dis 68:238–241
Acknowledgements
This work has been previously presented as an oral presentation at the Annual American College of Rheumatology meeting in 2019.
Funding
This study was funded by the Innovative Project Award (19IPLOI34760622) of the American Heart Association to Dr Singh.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Namrata Singh and Mary Vaughan-Sarrazin are co-senior authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Iyer, P., Gao, Y., Jalal, D. et al. Hydroxychloroquine use is associated with reduced mortality risk in older adults with rheumatoid arthritis. Clin Rheumatol 43, 87–94 (2024). https://doi.org/10.1007/s10067-023-06714-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-023-06714-5