Abstract
Objectives
To evaluate the efficacy and safety of Janus kinase (JAK) inhibitors (Jakinibs) in the treatment of psoriasis and psoriatic arthritis (PsA).
Methods
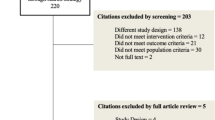
Databases including PubMed, Embase, Web of Science, and Cochrane Library were searched for randomized controlled trials on the efficacy and safety of Jakinibs in treating psoriasis and PsA from inception to July 2021. A systematic review and meta-analysis were performed to estimate pooled relative risk (RR) and 95% confidence interval (CI).
Results
Seventeen clinical trials (16 publications) comprising 6802 patients were included. All Jakinibs demonstrated significantly higher response rates compared with placebo (ACR20: RR 2.09, 95% CI 1.90–2.30; PASI75: RR 4.03, 95% CI 3.13–5.18). Within the subgroup analysis, the response rates defined by ACR20 were highest for filgotinib (RR 2.40, 95% CI 1.67–3.45), followed by upadacitinib, tofacitinib, and deucravacitinib. The proportion of patients achieving PASI75 response in the tofacitinib 10 mg twice daily group was significantly higher than that in the tofacitinib 5 mg group. Regarding safety, the incidence of adverse events (AEs) was significantly higher for Jakinibs compared with placebo (RR 1.17, 95% CI 1.11–1.23). Of note, a considerable increase in the risk of infections including upper respiratory tract and herpes zoster infection was observed among patients in the treatment group. For tofacitinib, upadacitinib, and filgotiniband, infection was the most prevalent AE. Moreover, AEs in the 10 mg tofacitinib group were higher than those in the 5 mg tofacitinib group.
Conclusion
Jakinibs are efficacious interventions for the treatment of psoriasis and PsA, but they are associated with an increased risk of AEs when compared with placebo. The long-term efficacy and safety data require further evaluation.
Key Points • This systematic review investigated and compared the efficacy and safety of different Jakinibs including the novel selective TYK2 inhibitors. • Jakinibs are efficacious interventions for the treatment of psoriasis and PsA. • A relatively higher dosing schedule of Jakinibs is associated with increased toxicity. |




Similar content being viewed by others
Data Availability
The data supporting the findings of this study are available within the article and its supplementary materials.
References
Michalek IM, Loring B, John SM (2017) A systematic review of worldwide epidemiology of psoriasis. J Eur Acad Dermatol Venereol 31(2):205–12. https://doi.org/10.1111/jdv.13854
Armstrong AW, Read C (2020) Pathophysiology, clinical presentation, and treatment of psoriasis: a review. JAMA 323(19):1945–1960. https://doi.org/10.1001/jama.2020.4006
Helmick CG, Lee-Han H, Hirsch SC, Baird TL, Bartlett CL (2014) Prevalence of psoriasis among adults in the U.S.: 2003–2006 and 2009–2010 National Health and Nutrition Examination Surveys. Am J Prev Med 47(1):37–45. https://doi.org/10.1016/j.amepre.2014.02.012
Ritchlin CT, Colbert RA, Gladman DD (2017) Psoriatic arthritis. N Engl J Med 376(10):957–970. https://doi.org/10.1056/NEJMra1505557
Griffiths CEM, Armstrong AW, Gudjonsson JE, Barker J (2021) Psoriasis. Lancet 397(10281):1301–1315. https://doi.org/10.1016/s0140-6736(20)32549-6
FitzGerald O, Ogdie A, Chandran V, Coates LC, Kavanaugh A, Tillett W et al (2021) Psoriatic arthritis. Nat Rev Dis Primers 7(1):59. https://doi.org/10.1038/s41572-021-00293-y
Van den Bosch F, Coates L (2018) Clinical management of psoriatic arthritis. Lancet 391(10136):2285–94. https://doi.org/10.1016/s0140-6736(18)30949-8
McLornan DP, Pope JE, Gotlib J, Harrison CN (2021) Current and future status of JAK inhibitors. Lancet 398(10302):803–816. https://doi.org/10.1016/s0140-6736(21)00438-4
Stark GR, Darnell JE Jr (2012) The JAK-STAT pathway at twenty. Immunity 36(4):503–514. https://doi.org/10.1016/j.immuni.2012.03.013
D’Urso DF, Chiricozzi A, Pirro F, Calabrese L, Caldarola G, Fossati B et al (2020) New JAK inhibitors for the treatment of psoriasis and psoriatic arthritis. G Ital Dermatol Venereol 155(4):411–20. https://doi.org/10.23736/s0392-0488.20.06658-4
Lé AM, Puig L, Torres T (2022) Deucravacitinib for the treatment of psoriatic disease. Am J Clin Dermatol 23(6):813–822. https://doi.org/10.1007/s40257-022-00720-0
Nogueira M, Puig L, Torres T (2020) JAK inhibitors for treatment of psoriasis: focus on selective TYK2 inhibitors. Drugs 80(4):341–352. https://doi.org/10.1007/s40265-020-01261-8
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj 372:n71. https://doi.org/10.1136/bmj.n71
Taylor W, Gladman D, Helliwell P, Marchesoni A, Mease P, Mielants H (2006) Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis Rheum 54(8):2665–2673. https://doi.org/10.1002/art.21972
Fredriksson T, Pettersson U (1978) Severe psoriasis–oral therapy with a new retinoid. Dermatologica 157(4):238–244. https://doi.org/10.1159/000250839
Felson DT, Anderson JJ, Boers M, Bombardier C, Furst D, Goldsmith C et al (1995) American College of Rheumatology. Preliminary definition of improvement in rheumatoid arthritis. Arthritis Rheum 38(6):727–35. https://doi.org/10.1002/art.1780380602
Felson DT, Anderson JJ, Lange ML, Wells G, LaValley MP (1998) Should improvement in rheumatoid arthritis clinical trials be defined as fifty percent or seventy percent improvement in core set measures, rather than twenty percent? Arthritis Rheum 41(9):1564–1570. https://doi.org/10.1002/1529-0131(199809)41:9%3c1564::Aid-art6%3e3.0.Co;2-m
Coates LC, Fransen J, Helliwell PS (2010) Defining minimal disease activity in psoriatic arthritis: a proposed objective target for treatment. Ann Rheum Dis 69(1):48–53. https://doi.org/10.1136/ard.2008.102053
Ashcroft DM, Wan Po AL, Williams HC, Griffiths CE (1999) Clinical measures of disease severity and outcome in psoriasis: a critical appraisal of their quality. Br J Dermatol 141(2):185–191. https://doi.org/10.1046/j.1365-2133.1999.02963.x
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Bmj 343:d5928. https://doi.org/10.1136/bmj.d5928
Clark HD, Wells GA, Huët C, McAlister FA, Salmi LR, Fergusson D et al (1999) Assessing the quality of randomized trials: reliability of the Jadad scale. Control Clin Trials 20(5):448–452. https://doi.org/10.1016/s0197-2456(99)00026-4
Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J et al (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64(4):401–6. https://doi.org/10.1016/j.jclinepi.2010.07.015
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Papp KA, Menter A, Strober B, Langley RG, Buonanno M, Wolk R et al (2012) Efficacy and safety of tofacitinib, an oral Janus kinase inhibitor, in the treatment of psoriasis: a phase 2b randomized placebo-controlled dose-ranging study. Br J Dermatol 167(3):668–77. https://doi.org/10.1111/j.1365-2133.2012.11168.x
Schmieder GJ, Draelos ZD, Pariser DM, Banfield C, Cox L, Hodge M et al (2018) Efficacy and safety of the Janus kinase 1 inhibitor PF-04965842 in patients with moderate-to-serve psoriasis: phase II, randomized, double-blind, placebo-controlled study. Br J Dermatol 179(1):54–62. https://doi.org/10.1111/bjd.16004
Papp KA, Menter MA, Abe M, Elewski B, Feldman SR, Gottlieb AB et al (2015) Tofacitinib, an oral Janus kinase inhibitor, for the treatment of chronic plaque psoriasis: results from two randomized, placebo-controlled, phase III trials. Br J Dermatol 173(4):949–961. https://doi.org/10.1111/bjd.14018
Papp K, Pariser D, Catlin M, Wierz G, Ball G, Akinlade B et al (2015) A phase 2a randomized, double-blind, placebo-controlled, sequential dose-escalation study to evaluate the efficacy and safety of ASP015K, a novel Janus kinase inhibitor, in patients with moderate-to-severe psoriasis. Br J Dermatol 173(3):767–76. https://doi.org/10.1111/bjd.13745
Ludbrook VJ, Hicks KJ, Hanrott KE, Patel JS, Binks MH, Wyres MR et al (2016) Investigation of selective JAK1 inhibitor GSK2586184 for the treatment of psoriasis in a randomized placebo-controlled phase IIa study. Br J Dermatol 174(5):985–995. https://doi.org/10.1111/bjd.14399
Papp KA, Menter MA, Raman M, Disch D, Schlichting DE, Gaich C et al (2016) A randomized phase 2b trial of baricitinib, an oral Janus kinase (JAK) 1/JAK2 inhibitor, in patients with moderate-to-severe psoriasis. Br J Dermatol 174(6):1266–76. https://doi.org/10.1111/bjd.14403
Jin T, Sun Z, Chen X, Wang Y, Li R, Ji S et al (2017) Serum human beta-defensin-2 is a possible biomarker for monitoring response to JAK inhibitor in psoriasis patients. Dermatology 233(2–3):164–9. https://doi.org/10.1159/000475809
Zhang J, Tsai T-F, Lee M-G, Zheng M, Wang G, Jin H et al (2017) The efficacy and safety of tofacitinib in Asian patients with moderate to severe chronic plaque psoriasis: a phase 3, randomized, double-blind, placebo-controlled study. J Dermatol Sci 88(1):36–45. https://doi.org/10.1016/j.jdermsci.2017.05.004
Bachelez H, van de Kerkhof PCM, Strohal R, Kubanov A, Valenzuela F, Lee J-H et al (2015) Tofacitinib versus etanercept or placebo in moderate-to-severe chronic plaque psoriasis: a phase 3 randomised non-inferiority trial. Lancet 386(9993):552–561. https://doi.org/10.1016/s0140-6736(14)62113-9
Papp K, Gordon K, Thaçi D, Morita A, Gooderham M, Foley P et al (2018) Phase 2 trial of selective tyrosine kinase 2 inhibition in psoriasis. N Engl J Med 379(14):1313–21. https://doi.org/10.1056/NEJMoa1806382
Mease P, Hall S, FitzGerald O, van der Heijde D, Merola JF, Avila-Zapata F et al (2017) Tofacitinib or adalimumab versus placebo for psoriatic arthritis. N Engl J Med 377(16):1537–50. https://doi.org/10.1056/NEJMoa1615975
Gladman D, Rigby W, Azevedo VF, Behrens F, Blanco R, Kaszuba A et al (2017) Tofacitinib for psoriatic arthritis in patients with an inadequate response to TNF inhibitors. N Engl J Med 377(16):1525–1536. https://doi.org/10.1056/NEJMoa1615977
Mease P, Coates LC, Helliwell PS, Stanislavchuk M, Rychlewska-Hanczewska A, Dudek A et al (2018) Efficacy and safety of filgotinib, a selective Janus kinase 1 inhibitor, in patients with active psoriatic arthritis (EQUATOR): results from a randomised, placebo-controlled, phase 2 trial. Lancet 392(10162):2367–77. https://doi.org/10.1016/s0140-6736(18)32483-8
McInnes IB, Anderson JK, Magrey M, Merola JF, Liu Y, Kishimoto M et al (2021) Trial of upadacitinib and adalimumab for psoriatic arthritis. N Engl J Med 384(13):1227–1239. https://doi.org/10.1056/NEJMoa2022516
Mease PJ, Lertratanakul A, Anderson JK, Papp K, Van den Bosch F, Tsuji S et al (2020) Upadacitinib for psoriatic arthritis refractory to biologics: SELECT-PsA 2. Ann Rheum Dis 80(3):312–20. https://doi.org/10.1136/annrheumdis-2020-218870
Mease PJ, Deodhar A, Van Der Heijde D, Behrens F, Kivitz A, Kim J et al (2021) Efficacy and safety of deucravacitinib, an oral, selective tyrosine kinase 2 inhibitor, in patients with active psoriatic arthritis: results from a phase 2, randomized, doubleblind, placebo-controlled trial. Ann Rheum Dis 80(SUPPL 1):314–315. https://doi.org/10.1136/annrheumdis-2021-eular.2603
Singh JA, Guyatt G, Ogdie A, Gladman DD, Deal C, Deodhar A et al (2019) Special article: 2018 American College of Rheumatology/National Psoriasis Foundation guideline for the treatment of psoriatic arthritis. Arthritis Rheumatol 71(1):5–32. https://doi.org/10.1002/art.40726
Coates LC, Kavanaugh A, Mease PJ, Soriano ER, Laura Acosta-Felquer M, Armstrong AW et al (2016) Group for research and assessment of psoriasis and psoriatic arthritis 2015 treatment recommendations for psoriatic arthritis. Arthritis Rheumatol 68(5):1060–71. https://doi.org/10.1002/art.39573
Campanaro F, Batticciotto A, Zaffaroni A, Cappelli A, Donadini MP, Squizzato A (2021) JAK inhibitors and psoriatic arthritis: a systematic review and meta-analysis. Autoimmun Rev 20(10):102902. https://doi.org/10.1016/j.autrev.2021.102902
Song GG, Choi SJ, Lee YH (2019) Comparison of the efficacy and safety of tofacitinib and upadacitinib in patients with active rheumatoid arthritis: a Bayesian network meta-analysis of randomized controlled trials. Int J Rheum Dis 22(8):1563–71. https://doi.org/10.1111/1756-185x.13616
Merola JF, Elewski B, Tatulych S, Lan S, Tallman A, Kaur M (2017) Efficacy of tofacitinib for the treatment of nail psoriasis: two 52-week, randomized, controlled phase 3 studies in patients with moderate-to-severe plaque psoriasis. J Am Acad Dermatol 77(1):79-87.e1. https://doi.org/10.1016/j.jaad.2017.01.053
Papp KA, Bissonnette R, Gooderham M, Feldman SR, Iversen L, Soung J et al (2016) Treatment of plaque psoriasis with an ointment formulation of the Janus kinase inhibitor, tofacitinib: a phase 2b randomized clinical trial. BMC Dermatol 16(1):15. https://doi.org/10.1186/s12895-016-0051-4
Ports WC, Khan S, Lan S, Lamba M, Bolduc C, Bissonnette R et al (2013) A randomized phase 2a efficacy and safety trial of the topical Janus kinase inhibitor tofacitinib in the treatment of chronic plaque psoriasis. Br J Dermatol 169(1):137–145. https://doi.org/10.1111/bjd.12266
Punwani N, Scherle P, Flores R, Shi J, Liang J, Yeleswaram S et al (2012) Preliminary clinical activity of a topical JAK1/2 inhibitor in the treatment of psoriasis. J Am Acad Dermatol 67(4):658–64. https://doi.org/10.1016/j.jaad.2011.12.018
Bechman K, Subesinghe S, Norton S, Atzeni F, Galli M, Cope AP et al (2019) A systematic review and meta-analysis of infection risk with small molecule JAK inhibitors in rheumatoid arthritis. Rheumatology (Oxford) 58(10):1755–1766. https://doi.org/10.1093/rheumatology/kez087
Horreau C, Pouplard C, Brenaut E, Barnetche T, Misery L, Cribier B et al (2013) Cardiovascular morbidity and mortality in psoriasis and psoriatic arthritis: a systematic literature review. J Eur Acad Dermatol Venereol 27(Suppl 3):12–29. https://doi.org/10.1111/jdv.12163
Xie W, Huang Y, Xiao S, Sun X, Fan Y, Zhang Z (2019) Impact of Janus kinase inhibitors on risk of cardiovascular events in patients with rheumatoid arthritis: systematic review and meta-analysis of randomised controlled trials. Ann Rheum Dis 78(8):1048–54. https://doi.org/10.1136/annrheumdis-2018-214846
Yates M, Mootoo A, Adas M, Bechman K, Rampes S, Patel V et al (2021) Venous thromboembolism risk with JAK inhibitors: a meta-analysis. Arthritis Rheumatol 73(5):779–88. https://doi.org/10.1002/art.41580
Dendrou CA, Cortes A, Shipman L, Evans HG, Attfield KE, Jostins L et al (2016) Resolving TYK2 locus genotype-to-phenotype differences in autoimmunity. Sci Transl Med 8(363):363ra149. https://doi.org/10.1126/scitranslmed.aag1974
Funding
This study was supported by the National Basic Research Program of China (973 Program) (No. 2014CB541801).
Author information
Authors and Affiliations
Contributions
FY, XL, and XZ conceived the study and designed the protocol. FY and CL performed the literature search. FY and CL selected the studies and extracted the relevant information. FY and YW synthesized the data. FY wrote the first draft of the paper. All authors critically revised successive drafts of the paper and approved the final version. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, F., Lu, C., Wang, Y. et al. Efficacy and safety of Janus kinase inhibitors in patients with psoriasis and psoriatic arthritis: a systematic review and meta-analysis. Clin Rheumatol 42, 1593–1605 (2023). https://doi.org/10.1007/s10067-023-06529-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-023-06529-4