Abstract
Digital ulcers (DUs) comprise the main manifestation of vasculopathy and are a major cause of disability in patients with systemic sclerosis (SSc). A literature search in Web of Science, PubMed and Directory of Open Access Journals was performed in December 2022 to identify articles published in the last decade regarding the management of DUs. Prostacyclin analogues, endothelin antagonists and phosphodiesterase 5 inhibitors have shown promising results both as a stand-alone treatment and in combination for the treatment of existing and prevention of new DUs. Moreover, autologous fat grafting and botulinum toxin injections, although not readily available, can be of use in recalcitrant cases. Many investigational treatments with promising results could pave the way for a paradigm shift in the treatment of DUs in the future. Despite these recent advances, challenges remain. Better-designed trials are of paramount importance to optimise DU treatment in the years to come.
Key Points • DUs are a major cause of pain and reduced quality of life in patients with SSc. • Prostacyclin analogues and endothelin antagonists have shown promising results both as a stand-alone treatment and in combination for the treatment of existing and prevention of new DUs. • In the future, a combination of more powerful vasodilatory drugs, perhaps in conjunction with topical approaches, may improve outcomes. |
Similar content being viewed by others
Introduction
Systemic sclerosis (SSc), a prototype fibrotic disease, is characterised by an interplay between genetic predisposition and environmental triggers that leads to a dysregulated immune response, vasculopathy and eventually fibrosis. Among the various end-organ manifestations, digital ulcers (DUs) are one of the most common, affecting more than half of the patients at some stage during the course of disease, with the probability of developing digital ulcers reaching in some registries even 70% [1]. DUs are defined as well-demarcated areas of tissue loss of varying extent that can be denuded or covered by necrotic tissue [2]. From a pathophysiological perspective, fingertip DUs are thought to be a direct ischemic complication of the progressive vasculopathy, while those occurring over bony protuberances, mainly on the extensor aspect of the small joints of the hands, are most likely caused by recurrent microtrauma [3]. Albeit not the leading cause of morbidity and mortality in patients with SSc, DUs usually cause severe pain and disability due to functional impairment. DUs associate with a reduced quality of life and an increased economic burden, rendering their effective prevention and treatment a strategic target in SSc management [2].
The substantial progress of basic research in the last few years has led to a better understanding of the pathophysiology of SSc-related vasculopathy, identifying emerging therapeutic targets. In this narrative review, we highlight the most recent advances in the management of DUs in the past decade, including therapies currently in clinical trials or preclinical development. We also underline research priorities that could change the therapeutic landscape in the years to come.
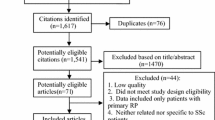
Methods
We performed an electronic search in Medline, Web of Science, Scopus and the Directory of Open Access Journals (DOAJ) from September 2012 to December 2022 using the following keywords: systemic sclerosis, digital ulcers and management in all combinations. We included cross-sectional studies, clinical trials, case series/reports and letters to the editor published in English language. Our search was focused only on articles related to the management of digital ulcers. A manual search was performed in the reference list of the included articles to extract relevant additional studies. Unpublished studies and gray literature were not considered.
Results
Pharmacological therapy
Prostacyclin analogues
Prostacyclin is a potent vasodilator with antithrombotic and antiproliferative properties that has been used in the treatment of refractory Raynaud’s phenomenon and SSc-associated DUs since the 1980s. The three prostacyclin analogues that are currently commercially available in Europe are iloprost, treprostinil and epoprostenol. Hypotension, headaches and flushing comprise some of their most encountered side effects and are mainly associated with the intravenous route of administration; however, a dose tapering to 0.5 ng/kg/min leads to a resolution of most adverse events in the majority of cases [4, 5]. BMI seems to be a major predictive factor of drug intolerance, as overweight patients tolerate lower iloprost infusion rates and have a 13-fold increased risk of developing adverse effects [6].
Iloprost is a synthetic analogue of prostacyclin that binds to prostacyclin and prostaglandin E2 receptors with equal affinity. Beside its antiplatelet, immunomodulating and cytoprotective properties, emerging data suggest a potential disease-modifying effect in patients with SSc [7]. Despite its short half-life, its clinical efficacy can extend for weeks after treatment cessation. This property may reflect its ability to inhibit CXCL10, a known, early contributor to SSc-associated vasculopathy, effectively preventing activation of endothelial cells and dermal fibroblasts in patients with SSc [8]. Moreover, iloprost stabilises endothelial adherence junctions preventing vascular dysfunction in SSc [9].
The PROSIT, an observational, multicentric study, retrospectively assessed an Italian cohort of 346 patients with SSc-related RP and/or DUs under long-term treatment with iloprost. For the management of active DUs, the authors employed and recommend a combination of iloprost plus calcium channel blockers (CCB) plus endothelin receptor antagonists. A reduction in the frequency and severity of DU lesions was reported by 74% of the participants using a validated Treatment Satisfaction Questionnaire for Medication. Most patients experienced relevant side effects such as hypotension, headache, flushing, vomiting and diarrhoea which were in only 14% of the cases prolonged. Some experts suggest the use of premedication like paracetamol or dopamine receptor antagonists to lower the rate of adverse events [10]. A similar retrospective real-world study found that 71% of patients with SSc receiving monthly iloprost infusions were free from DUs at the end of a decade-long follow-up period [11]. On the other hand, iloprost withdrawal was linked to worsening of RP and DUs recurrence [12]. Most patients on monthly iloprost infusions experience complete clinical resolution in the first year of treatment with the 10-year survival rate reaching in one cohort 55.6% [13]. In the absence of tools such as capillaroscopy, which require a certain level of experience and are operator dependent, simple clinical tests such as Allen’s test that can be performed easily at bedside can be employed as predictors of patient outcome; DUs in patients with a negative Allen’s test show expedited healing times [14]. Clinical improvement and a switch to easier, more cost-efficient ways of administration such as an elastomeric pump seem to be the main reasons of drug discontinuation [13]. Elastomeric pumps have been shown to be equally effective to the intravenous route, provide greater patient autonomy and are associated with fewer adverse events because of their continuous slow-release rate [15].
Despite the central role of iloprost in the management of DUs, its optimal infusion schedule has yet to be established. High-quality data from randomised trials are lacking, as all studies published to date assessed only short treatment regimens, no more than 5 days of daily treatment. In a recently published French observational retrospective study, a longer duration of iloprost treatment (more than 5 days, median 7.3 days) shortened DU healing times by half in comparison to shorter 3–5-day treatment courses (48 [7–392] vs. 91 [9–365] median days, range, respectively). At 3 months, more than half of the patients treated with the prolonged duration regimen experienced a complete resolution of the DUs in contrast to a mere 37% in the other cohort. The number of active DUs before treatment, concurrent treatment with endothelin antagonists, calcium channel blockers or other immunosuppressive agents, such as cyclophosphamide and methotrexate, did not affect healing times. Moreover, a statistical significance could not be observed in the number of DU-related complications between the two groups. The observed side effects were more common in patients receiving concomitantly calcium channel blockers [16]. Collectively, longer treatment courses could represent an efficacious, albeit costly alternative, especially in patients with more severe disease.
Treprostinil, a newer oral prostacyclin analogue, did not reach the prespecified primary endpoint of overall DU burden reduction after 20 weeks of treatment in a large, double-blind placebo-controlled trial (DISTOL-1). Nevertheless, a retrospective analysis of the medical charts of the patients after the termination of the trial as well as unpublished data from the extension study that succeeded it found evidence of a significantly increased total DU number following discontinuation of treprostinil and after adjusting for potential seasonal effects. Most of the observed side effects are dose-dependent, of mild or moderate intensity and include headache, diarrhoea and nausea. The failure to meet the primary endpoint in the randomised trial could be attributed to a heterogeneity of the initial patient cohort or inherent difficulties in performing high-quality DU studies such as the variable, experience-dependent definition of DU activity [17, 18]. Further study is warranted, when feasible taking into account specific biomarkers such as the subtype of SSc and the antibody status of the patients; patients with diffuse cutaneous SSc and no evidence of anticentromere antibodies may profit from treatment with treprostinil. Table 1 summarises all key data regarding prostacyclin analogues.
In addition to prostacyclin analogues, selexipag, an oral selective IP-prostacyclin receptor agonist, which is currently approved for the treatment of pulmonary hypertension, led to complete healing of the DUs in 6 patients with SSc, after first- and second-line agents failed to show efficacy. The observed effect was achieved after 3–6 months of treatment with 2.400–3.000 mg selexipag daily [19]. Despite these promising results, clinical trial data to support the routine use of selexipag in hard-to-treat DUs are lacking.
Endothelin antagonists
Endothelin-1 (ET-1), a potent vasoconstrictive and potentially inflammatory and fibrotic mediator, is considered a key orchestrator of the vascular changes and tissue remodelling in SSc. Although bosentan, ambrisentan and macitentan are currently used for the treatment of pulmonary arterial hypertension, only bosentan, a competitive antagonist targeting both ETA and ETB endothelin receptors, is currently licenced for the prevention of DU development.
Two randomised double-blind placebo-controlled trials provided rationale for its use in DU treatment. Most recently, in the RAPIDS-2 trial, 188 patients with SSc and at least one active DU were enrolled in a 20-week comparison of 125 mg bosentan twice daily versus placebo, after the patients were treated with half the dose of bosentan for 4 weeks at the initial phase of the study. A substantial reduction of 30% in the development of new DUs in patients with both diffuse and limited SSc was observed [20], although, in a subsequent study, no relationship could be established between this favourable outcome and the bosentan-induced increased digital blood flow [21]. A wide individual variability in the hand blood flow of patients with SSc could account for this lack of association. This beneficial effect was not extrapolated in the times to healing of the active DU, patient-reported overall hand pain scores or ulcer burden, as no differences were evident between the treatment and placebo group [20]. Even though the overall number of side effects did not differ significantly between the two groups, the increased incidence of elevated liver enzymes in subsects receiving treatment highlights the need for regular blood monitoring in patients on bosentan.
An Italian retrospective case-control study further corroborated a statistically significant lower occurrence of DUs in bosentan-treated patients with SSc [22], while the beneficial effects of bosentan were further reflected by an improvement of the self-reported visual analogue scale-digital ulcers score at a 12th-month follow-up visit, in another study [23]. In a subsequent prospective observational study in a Turkish cohort with SSc, 26.7% of the patients with diffuse cutaneous SSc developed new DUs under bosentan, while four patients suffered from critical digital ischemia requiring additional treatment with iloprost [24].
In other reports, bosentan was shown to be effective in the management of nondigital ulcers too, specifically those occurring on the basis of an impaired peripheral circulation [25, 26].
Moreover, mounting data provide evidence for the use of bosentan as an add-on treatment in patients with SSc already on iloprost. In a retrospective study of 34 patients with SSc and refractory digital ulcers despite 6 months of iloprost treatment, the addition of bosentan in the therapeutic regimen led to a significant decrease in the mean number of digital ulcers on the hands from 1.7 to 0.7 (p = 0.00003). A similar effect could not be observed in regard to the lower limbs. The degree of digital skin fibrosis seems to play a pivotal role in DU healing since only 18% of ulcers in patients with severe digital fibrosis healed in comparison with 80% in patients with mild disease [27]. Furthermore, in an Italian study of 30 patients with SSc, this synergistic effect was reflected by a statistically significant reduction of 80% in the incidence of new DUs [28], while a more recent retrospective study showed a 37.84% decrease in the prevalence of DUs with concurrent treatment [29]. An accompanying increase of capillaries acting as a surrogate marker for an improvement of the microvascular damage has also been reported under ET-1 antagonism and iloprost combination [28, 30]. Finally, bosentan seems to be a promising treatment for DUs presenting in the context of a paraneoplastic syndrome [31].
Macitentan is, like bosentan, a dual endothelin ETA/ETB receptor antagonist. Due to its slower receptor dissociation rate, macitentan possesses a theoretical potential to block ET-1 signalling more effectively than other ET-1 inhibitors [32]. In the phase III randomised, double-blind, placebo-controlled DUAL-1 and DUAL-2 trials, which involved approximately 70 centres worldwide each, the effectiveness of macitentan was evaluated in 226 and 216 patients, respectively, with SSc and active DUs. In each study, patients were either treated with 3 mg or 10 mg of macitentan or placebo once daily. Both trials could not achieve the primary endpoint of a reduction in the cumulative number of new DUs at week 16 of follow-up. Moreover, macitentan failed to improve hand function or reduce the overall hand pain related to DUs. These disappointing results led to a premature termination of DUAL-2, a decision based on patient safety concerns [33]. However, the findings of the DUAL trials should be interpreted critically. Better patient and clinician’s education as well as easier access to online information material on the prevention and management of SSc-associated DUs may be held accountable for the observed decrease in the number of new DUs in the control groups of both studies in comparison with the RAPID-2, thus rendering a possible beneficial effect of macitentan undetectable. Furthermore, the prior use of prostanoids and bosentan for the treatment of DUs might have posed a barrier regarding recruitment in the DUAL studies, excluding patients with severe DUs, who at least theoretically would be more likely to benefit from treatment. Despite some recent positive case reports [34, 35], macitentan is not yet a recommended treatment for DUs in the updated EULAR guidelines for the treatment of SSc.
Ambrisentan, a highly selective ETA inhibitor, has been shown to abate cellular proliferation and vasoconstriction while maintaining the vasodilatory effects of ETB-mediated signalling [32]. In a case series of six patients with SSc-related DUs receiving intravenous prostanoids, who were previously unsuccessfully treated with bosentan as an add-on therapy, ambrisentan administered at a dose of 5 mg/day resulted in the complete healing of all DUs in four patients at the end of the 24-week observation period. No new ulcers were detected while the number of RP attacks decreased significantly in all participants (Δ −3.10 p = 0.01) [36]. A larger, prospective open-label study found a similar reduction in the total number of DUs per patient (from 3.1 ± 2.1 to 1.3 ± 1.6, p = 0.004, weeks 0 and 24, respectively). However, ambrisentan did not prevent the development of new DUs over the study course [37]. A subsequent 12-week RCT found no improvement in the digital microvascular blood flow of patients treated with ambrisentan, indicating no measurable vasodilatory effect [38].
JAK inhibitors
Small molecules that inhibit the JAK signalling proteins are gaining traction in the past 5 years as treatment options in a wide range of rheumatic diseases. In SSc, Janus kinases are important transducers of pro-inflammatory and pro-fibrotic signals to key players of SSc pathogenesis, including fibroblasts and endothelial cells. In a case series, 3 out of 4 female patients with diffuse SSc and active DUs at baseline experienced a complete ulcer resolution at week 24 of treatment with baricitinib, while no new ulcers developed in any of the 10 patients treated. Furthermore, baricitinib led to a significant mean improvement of 49.23% in the Rodman skin score of the patients. The underlying pathophysiologic mechanisms that mediate this effect remain to be elucidated [39]. Tofacitinib was also used successfully in the treatment of DUs in an African American male patient with diffuse SSc [40]. Taken together, these data may pave a promising future for JAK inhibitors in SSc-associated DUs.
Topical treatment
Autologous fat grafting and mesenchymal cells transplantation
Accumulating evidence suggests that regional implantation of autologous adipose tissue-derived cell fractions could be a viable option for recalcitrant DUs. Adipose-derived stromal/stem cells (ASCs) exhibit an immunosuppressive capacity and angiogenic properties similar to those of mesenchymal stromal cells (MSCs) derived from bone marrow while they are easier to isolate and linked to reduced donor morbidity [41]. Based on the encouraging results of previous pilot studies [42, 43], an Italian group performed a monocentric RCT where autologous adipose tissue and placebo were injected at the base of the affected finger in 25 and 13 patients with active SSc-related DUs, respectively. Treatment with intravenous prostanoids and calcium-channel inhibitors, initiated before inclusion in the study, was continued in all patients enrolled. Complete DU healing was achieved in 92% of the patients treated with adipose tissue grafting after 8 weeks, while only one patient in the placebo arm experienced improvement of the DU (p < 0.0001). Moreover, no new ulcers had appeared in any of the patients treated with adipose tissue at a 3-month follow-up visit [44].
In a single-centre, open-label pilot study, autologous MSCs were injected in 40 patients with ischemic DUs due to either SSc or arteriosclerosis-associated peripheral artery disease (11 and 29 patients, respectively). Even though the visual analogue pain scores decreased significantly after treatment, 18.2% of the patients with SSc suffered from a recurrence of limb ischemia at the 2-year follow-up, while one patient required digital amputation [45].
Botulinum toxin injection
Several case series provide evidence for the use of botulinum toxin A (BTX-A) in the treatment of intractable DUs [46,47,48,49]. BTX-A, a selective acetylcholine release inhibitor, is thought to improve digital blood flow and inhibit vasoconstriction via vascular smooth muscle paralysis and blocking of noradrenaline release [47]. A recent study showed that a higher concentration and total dose of BTX-A when injected at the digital neurovascular bundle may lead to improved outcomes, such as vasospastic symptom control and ulcer healing with a favourable adverse effect profile [49]. In a subsequent single-blind RCT from the same group, BTX-B was shown to be effective in accelerating the healing of refractory to standard treatment DUs and preventing the development of new ones at 16 weeks of follow-up in patients with SSc [50]. Moreover, topical BTX treatment seems to be a cost-efficient, equally effective alternative to intravenous prostanoids that can be administered in the outpatient setting [51]. Collectively, more clinical data are needed to establish botulinum toxin injections as a standard treatment for DUs.
Sympathectomy
Although thoracic sympathectomy is nowadays an obsolete method owing to a high rate of adverse events, digital sympathectomy may represent a viable option for DUs refractory to standard care. A retrospective study of SSc-related DUs found a 92.3% post-sympathectomy improvement in pain, while all but two patients experienced DU healing [52].
Investigational treatments options
Riociguat
Riociguat, a first-in-class guanylate cyclase stimulator, is currently approved for the treatment of pulmonary arterial hypertension and chronic thromboembolic arterial hypertension. A randomised, double-blind, placebo-controlled trial did not find any difference of statistical significance in the net ulcer burden (primary endpoint) and other secondary outcome measures such as healing of all baseline DUs and healing of the cardinal DU between the 2 groups at week 16 of treatment [53]. However, a longer treatment duration might have been necessary for the treatment effect to be notable, as suggested by the positive trends in DU healing, documented in the open-label phase of the study.
Ozone
Ozone, a bactericidal gas with antioxidant properties and proven efficacy in the management of chronic wounds, was found in a randomised, blinded, controlled trial of 50 female patients with SSc-associated DUs to induce a significantly greater ulcer size reduction in comparison to calcium channel blockers (control group) at day 20 of treatment. The ulcer pain score and the number/duration of Raynaud’s phenomenon attacks were also decreased in the ozone treatment arm. The reported upregulation of growth factors such as VEGF and TGFβ in local ulcer tissue after ozone treatment may promote epithelialization and at least partially account for the observed effect [54]. A subsequent smaller study yielded similar results [55].
Hyperbaric oxygen therapy
Hyperbaric oxygen therapy (HBOT) utilises pure oxygen applied in a closed chamber at increased pressure, generally 2–3 atmospheres to induce hyperoxia and hyperoxemia. Its proven antimicrobial, angiogenic and immunomodulatory effects are used therapeutically in a wide array of diseases, including chronic ulcers [56]. In a recent report, the DUs in 2 out of 3 female patients with SSc healed completely, after 60 and 40 HBOT therapy sessions, respectively. No adverse events were documented during the treatment [57]. The therapeutic effects are thought to be mediated via an enhanced oxygen delivery in the DUs’ hypoxic environment and an upregulation of NO production, a potent vasodilator. Another case study provided similar results [58].
Extracorporeal shock wave therapy
Extracorporeal shock wave therapy (ESWT), a technique primarily used in lithotripsy, is recently shown to accelerate tissue regeneration and promote angiogenesis. In a phase 2 pilot study of 9 patients with SSc-related DUs, ESWT was effective in reducing DU size and number, although it did not prevent the development of new ones. Treatment was not associated with any side effects [59].
Low-level light therapy
Light treatment has been lately successfully employed in the treatment of recalcitrant skin ulcers. The therapeutic effect is thought to be achieved through a plethora of mechanisms, including stimulation of collagen deposition, an antibacterial effect and a local NO-dependent increase in tissue perfusion. In a feasibility study, a novel combination of infrared, red and violet light showed promising results as a safe, minimally invasive treatment in the management of DUs [60]. Currently, an ongoing, open-label, prospective randomised controlled trial (S.U.I.T.A.B.L.E) will assess the clinical effectiveness of a portable blue light device on DU healing after 16 consecutive weeks compared to standard treatment in patients suffering from SSc.
Rheopheresis (RheoP)
RheoP is a safe and effective therapeutic modality to treat microcirculatory disorders. It comprises a double filtration plasmapheresis system that selectively removes large plasma proteins, thus reducing the whole blood viscosity. RheoP was successful in treating recalcitrant DUs in a female patient with SSc. No new ulcers were reported during treatment and at a 3-month follow-up visit. Moreover, no major side effects were seen. To further investigate the potential benefit of Rheopheresis in Raynaud’s phenomenon and DUs, the Rheact, a randomised controlled feasibility study, is currently ongoing [61, 62] (Trial Identifier: NCT05204784).
G-CSF
Granulocyte colony-stimulating factor (G-CSF) is an immunoregulatory cytokine that exerts antimicrobial, angiogenetic and tissue regenerative effects. Daily treatment with filgrastim 300 μg, a G-CSF analogue, over three consecutive days resulted in a complete resolution of DUs in eight out of ten patients with SSc, while the mean time to DU healing was 1 and a half months [63].
Phosphodiesterase 5 inhibitors (PDEi5)
PDEi5 inhibit phosphodiesterase, an enzyme that catalyses the hydrolysis of cGMP in endothelial cells. The resulting increase in cGMP levels induces muscular smooth muscle relaxation and vasodilatation [64]. Because of these properties, they are recommended as a treatment for DUs in the updated EULAR guidelines for the management of SSc. Adverse events are not uncommon and include vasomotor reactions, myalgias, nasal stuffiness, visual abnormalities and allergic reactions [65].
Sildenafil, used primarily for the treatment of pulmonary hypertension in SSc at 20 mg three times daily orally, decreases the severity, frequency and duration of RP attacks. In a randomised, double-blind, placebo-controlled trial (SEDUCE trial), 83 patients with SSc were randomly assigned to either sildenafil 20 mg thrice daily or placebo. Sildenafil reduced the number of DUs per patient at weeks 8 and 12 (1.23 ± 1.61 vs. 1.79 ± 2.40, p = 0.04; 0.86 ± 1.62 vs 1.51 ± 2.68, p = 0.01, in the sildenafil and placebo group, respectively). Even though the primary endpoint evaluating the time to DU healing was not achieved because of a higher-than-expected healing ratio in the placebo group, sildenafil remains a useful treatment option for DUs in SSc [66].
Tadalafil, a phosphodiesterase 5 inhibitor, was recently found to be effective in reducing the RP-associated pain when used as an add-on topical therapy to standard care. Although a significant decrease in the number of DUs was not achieved, larger, randomised trials are needed to draw definitive conclusions [67].
Other treatments that were found to be effective in DU management include low-dose immune globulin and oral psoralen plus ultraviolet A therapy [68, 69]. The above investigational agents are summarised in Table 2.
Discussion
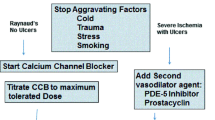
Even though DUs are not directly linked to the increased mortality seen in patients with SSc, they are very important from a clinical point of view since they associate with excruciating pain and significant functional impairment. The treatment of DUs remains challenging and suboptimal despite recent advances. In everyday clinical practice, the endothelin antagonist bosentan is commonly used for the prevention of new DUs. However, its high cost is a significant burden especially in countries with strict health care budget, but this issue may improve in the near future with the wider use of generics. There are only very limited data regarding the efficacy of other endothelin antagonists, and therefore, their use should be restricted to selected cases. On the other hand, prostacyclin analogues are certainly one of the most effective agents for the prevention and treatment of DUs, but again, their use has limitations such as very high cost, low availability and problematic route of administration. A combination of bosentan and iloprost appears promising for difficult-to-treat cases. Apart from these drugs, one should keep in mind that simple nonpharmacologic measures such as smoking cessation and avoiding exposure to cold are of outmost importance. All physicians should strongly encourage patients with SSc to apply these simple but critical lifestyle changes. Topical treatment in the form of autologous adipose grafting and botulinum toxin have shown promising yet preliminary results, and for the time being, they should be used with caution in selected cases in highly specialised centres.
In conclusion, during the last decade, we had some significant advances such as the approval of bosentan for the prevention of DUs, but still, we have a long way to go. There are several treatment options, but so far, efficacy has been modest. We definitely need more large-scale studies assessing combination treatments such as iloprost plus endothelin antagonists or endothelin antagonists plus PDE5i. In the future, a combination of more powerful vasodilatory drugs, perhaps in conjunction with topical approaches, may improve outcomes.
References
Hughes M, Allanore Y, Chung L et al (2020) Raynaud phenomenon and digital ulcers in systemic sclerosis. Nat Rev Rheumatol 16:208–221. https://doi.org/10.1038/s41584-020-0386-4
Morrisroe K, Stevens W, Sahhar J et al (2019) Digital ulcers in systemic sclerosis: their epidemiology, clinical characteristics, and associated clinical and economic burden. Arthritis Res Ther 21:1–12. https://doi.org/10.1186/s13075-019-2080-y
Hughes M, Herrick AL (2017) Digital ulcers in systemic sclerosis. Rheumatology 56:14–25. https://doi.org/10.1093/rheumatology/kew047
Hinze AM, Wigley FM (2018) Pharmacotherapy options in the management of Raynaud’s phenomenon. Curr Treatm Opt Rheumatol 4:235–254. https://doi.org/10.1007/s40674-018-0102-6
Bellando-Randone S, Bruni C, Lepri G et al (2018) The safety of iloprost in systemic sclerosis in a real-life experience. Clin Rheumatol 37:1249–1255. https://doi.org/10.1007/s10067-018-4043-0
Bixio R, Adami G, Bertoldo E et al (2022) Higher body mass index is associated with a lower iloprost infusion rate tolerance and higher iloprost-related adverse events in patients with systemic sclerosis. Ther Adv Musculoskelet Dis 14:1759720X2211371. https://doi.org/10.1177/1759720X221137125
Foti R, Visalli E, Amato G et al (2017) Long-term clinical stabilization of scleroderma patients treated with a chronic and intensive IV iloprost regimen. Rheumatol Int 37:245–249. https://doi.org/10.1007/s00296-016-3582-4
Colasanti T, Stefanantoni K, Fantini C et al (2022) The prostacyclin analogue iloprost modulates CXCL10 in systemic sclerosis. Int J Mol Sci 23:10150. https://doi.org/10.3390/ijms231710150
Tsou PS, Palisoc PJ, Flavahan NA, Khanna D (2021) Dissecting the cellular mechanism of prostacyclin analog iloprost in reversing vascular dysfunction in scleroderma. Arthritis and Rheumatology 73:520–529. https://doi.org/10.1002/art.41536
Negrini S, Magnani O, Matucci-Cerinic M et al (2019) Iloprost use and medical management of systemic sclerosis-related vasculopathy in Italian tertiary referral centers: results from the PROSIT study. Clin Exp Med 19:357–366. https://doi.org/10.1007/s10238-019-00553-y
Colaci M, Lumetti F, Giuggioli D, Guiducci S, Bellando-Randone S, Fiori G, Matucci-Cerinic M, Ferri C (2017) Long-term treatment of scleroderma-related digital ulcers with iloprost: a cohort study. Clin Exp Rheumatol 106(4):179–183 Epub 2017 Sep 18
de Lorenzis E, Natalello G, Verardi L et al (2022) Sudden winter iloprost withdrawal in scleroderma patients during COVID-19 pandemic. Microvasc Res 144:104404. https://doi.org/10.1016/j.mvr.2022.104404
Martins P, Dourado E, Fonseca JE, Romão V, Resende C (2022) The safety and persistence of intravenous iloprost in systemic sclerosis. ARP Rheumatol 1(2):122–128
Casigliani Rabl S, Della Rossa A, Pepe P et al (2012) Long-term cyclic intravenous iloprost in systemic sclerosis: clinical experience from a single center. Reumatismo 64:158–165. https://doi.org/10.4081/reumatismo.2012.158
Fartura Braga Temido MH, Gomes M, Parente F, Santos L (2019) Iloprost infusion through elastomeric pump in the treatment of Raynaud’s phenomenon and digital ulcers. J Scleroderma Relat Disord 4:NP1–NP4. https://doi.org/10.1177/2397198318765596
Jamart C, Levesque H, Thietart S et al (2022) Iloprost duration for digital ulcers in systemic sclerosis: French retrospective study at two centers and literature review. Front Med (Lausanne) 9:878970. https://doi.org/10.3389/fmed.2022.878970
Shah AA, Schiopu E, Chatterjee S et al (2016) The recurrence of digital ulcers in patients with systemic sclerosis after discontinuation of oral treprostinil. Journal of Rheumatology 43:1665–1671. https://doi.org/10.3899/jrheum.151437
Shah AA, Schiopu E, Hummers LK et al (2013) Open label study of escalating doses of oral treprostinil diethanolamine in patients with systemic sclerosis and digital ischemia: pharmacokinetics and correlation with digital perfusion. Arthritis Res Ther 15:R54. https://doi.org/10.1186/ar4216
del Papa N, Vitali C, Bilia S et al (2020) Selexipag may be effective in inducing digital ulcers healing in patients with systemic sclerosis. Clin Exp Rheumatol 38(Suppl 125):181–182
Matucci-Cerinic M, Denton CP, Furst DE et al (2011) Bosentan treatment of digital ulcers related to systemic sclerosis: results from the RAPIDS-2 randomised, double-blind, placebo-controlled trial. Ann Rheum Dis 70:32–38. https://doi.org/10.1136/ard.2010.130658
Meijs J, Voskuyl AE, Bloemsaat-Minekus JPJ, Vonk MC (2015) Blood flow in the hands of a predefined homogeneous systemic sclerosis population: the presence of digital ulcers and the improvement with bosentan. Rheumatology (United Kingdom) 54:262–269. https://doi.org/10.1093/rheumatology/keu300
Cozzi F, Pigatto E, Rizzo M et al (2013) Low occurrence of digital ulcers in scleroderma patients treated with bosentan for pulmonary arterial hypertension: a retrospective case-control study. Clin Rheumatol 32:679–683. https://doi.org/10.1007/s10067-013-2172-z
Rezus E, Burlui A, Gafton B et al (2019) A patient-centered approach to the burden of symptoms in patients with scleroderma treated with bosentan: a prospective single-center observational study. Exp Ther Med 19(3):1739–1746. https://doi.org/10.3892/etm.2019.8361
Küçükşahin O, Yildizgören MT, Gerede DM et al (2016) Bosentan for digital ulcers in patients with systemic sclerosis: single center experience. Arch Rheumatol 31:229–233. https://doi.org/10.5606/ArchRheumatol.2016.5811
Taniguchi T, Asano Y, Hatano M et al (2012) Effects of bosentan on nondigital ulcers in patients with systemic sclerosis. British Journal of Dermatology 166:417–421. https://doi.org/10.1111/j.1365-2133.2011.10581.x
Naert A, de Haes P (2013) Successful treatment with bosentan of lower extremity ulcers in a scleroderma patient. Case Rep Med 2013. https://doi.org/10.1155/2013/690591
de Cata A, Inglese M, Molinaro F et al (2016) Digital ulcers in scleroderma patients: a retrospective observational study. Int J Immunopathol Pharmacol 29:180–187. https://doi.org/10.1177/0394632015606846
Trombetta AC, Pizzorni C, Ruaro B et al (2016) Effects of longterm treatment with bosentan and iloprost on nailfold absolute capillary number, fingertip blood perfusion, and clinical status in systemic sclerosis. Journal of Rheumatology 43:2033–2041. https://doi.org/10.3899/jrheum.160592
Foti R, Amato G, Benenati A et al (2022) Intravenous iloprost in systemic sclerosis and its effect in cardiopulmonary function: a retrospective observational study. Eur Rev Med Pharmacol Sci 26:7967–7973 https://doi.org/10.26355/eurrev_202211_30149
Cutolo M, Ruaro B, Pizzorni C et al (2014) Longterm treatment with endothelin receptor antagonist bosentan and iloprost improves fingertip blood perfusion in systemic sclerosis. Journal of Rheumatology 41:881–886. https://doi.org/10.3899/jrheum.131284
Sharabi I, Tanay A, Zandman-Goddard G (2015) Digital ulcers, systemic sclerosis sine scleroderma and paraneoplastic phenomena responding to bosentan therapy. Isr Med Assoc J. 17(2):126–127
Enevoldsen FC, Sahana J, Wehland M et al (2020) Endothelin receptor antagonists: status quo and future perspectives for targeted therapy. J Clin Med 9:824. https://doi.org/10.3390/jcm9030824
Khanna D, Denton CP, Merkel PA et al (2016) Effect of macitentan on the development of new ischemic digital ulcers in patients with systemic sclerosis: Dual-1 and Dual-2 randomized clinical trials. JAMA 315:1975–1988. https://doi.org/10.1001/jama.2016.5258
Giner Serret E (2016) Swift and complete healing of digital ulcers after macitentan treatment. Case Rep Rheumatol 2016:1–4. https://doi.org/10.1155/2016/1718309
Gonçalves T, Santos L (2019) Macitentan in the treatment of severe digital ulcers. BMJ Case Rep 12:e228295. https://doi.org/10.1136/bcr-2018-228295
Parisi S, Peroni CL, Laganà A et al (2013) Efficacy of ambrisentan in the treatment of digital ulcers in patients with systemic sclerosis: a preliminary study. Rheumatology 52:1142–1144
Chung L, Ball K, Yaqub A et al (2014) Effect of the endothelin type A-selective endothelin receptor antagonist ambrisentan on digital ulcers in patients with systemic sclerosis: results of a prospective pilot study. J Am Acad Dermatol 71:400–401. https://doi.org/10.1016/j.jaad.2014.04.028
Bose N, Bena J, Chatterjee S (2015) Evaluation of the effect of ambrisentan on digital microvascular flow in patients with systemic sclerosis using laser Doppler perfusion imaging: a 12-week randomized double-blind placebo controlled trial. Arthritis Res Ther 17(1):44. https://doi.org/10.1186/s13075-015-0558-9
Hou Z, Su X, Han G et al (2022) JAK1/2 Inhibitor baricitinib improves skin fibrosis and digital ulcers in systemic sclerosis. Front Med (Lausanne) 9:859330. https://doi.org/10.3389/fmed.2022.859330
Deverapalli SC, Rosmarin D (2018) The use of JAK inhibitors in the treatment of progressive systemic sclerosis. Journal of the European Academy of Dermatology and Venereology 32:e328
Casteilla L (2011) Adipose-derived stromal cells: their identity and uses in clinical trials, an update. World J Stem Cells 3:25. https://doi.org/10.4252/wjsc.v3.i4.25
Papa N del, di Luca G, Sambataro D, et al (2015) Regional implantation of autologous adipose tissue-derived cells induces a prompt healing of long-lasting indolent digital ulcers in patients with systemic sclerosis. Cell Transplant 24:2297–2305. https://doi.org/10.3727/096368914X685636
Bene M del, Pozzi MR, Rovati L, et al (2014) Autologous fat grafting for scleroderma-induced digital ulcers an effective technique in patients with systemic sclerosis. Handchirurgie Mikrochirurgie Plastische Chirurgie 46:242–247. https://doi.org/10.1055/s-0034-1376970
del Papa N, di Luca G, Andracco R et al (2019) Regional grafting of autologous adipose tissue is effective in inducing prompt healing of indolent digital ulcers in patients with systemic sclerosis: results of a monocentric randomized controlled study. Arthritis Res Ther 21:7. https://doi.org/10.1186/s13075-018-1792-8
Takagi G, Miyamoto M, Tara S et al (2014) Therapeutic vascular angiogenesis for intractable macroangiopathy-related digital ulcer in patients with systemic sclerosis: a pilot study. Rheumatology (United Kingdom) 53:854–859. https://doi.org/10.1093/rheumatology/ket432
Souk JW, Kim HS (2019) Effects of botulinum toxin injection on systemic sclerosis-related digital ulcers. Korean Journal of Internal Medicine 34:1169–1170
Motegi SI, Yamada K, Toki S et al (2016) Beneficial effect of botulinum toxin A on Raynaud’s phenomenon in Japanese patients with systemic sclerosis: a prospective, case series study. Journal of Dermatology 43:56–62. https://doi.org/10.1111/1346-8138.13030
Motegi SI, Sekiguchi A, Saito S et al (2018) Successful treatment of Raynaud’s phenomenon and digital ulcers in systemic sclerosis patients with botulinum toxin B injection: assessment of peripheral vascular disorder by angiography and dermoscopic image of nail fold capillary. Journal of Dermatology 45:349–352. https://doi.org/10.1111/1346-8138.14140
Nagarajan M, McArthur P (2021) Targeted high concentration botulinum toxin A injections in patients with Raynaud’s phenomenon: a retrospective single-centre experience. Rheumatol Int 41:943–949. https://doi.org/10.1007/s00296-020-04606-4
Motegi SI, Uehara A, Yamada K et al (2017) Efficacy of botulinum toxin B injection for Raynaud’s phenomenon and digital ulcers in patients with systemic sclerosis. Acta Derm Venereol 97:843–850. https://doi.org/10.2340/00015555-2665
Shenavandeh S, Sepaskhah M, Dehghani S, Nazarinia MA (2022) A 4-week comparison of capillaroscopy changes, healing effect, and cost-effectiveness of botulinum toxin-A vs prostaglandin analog infusion in refractory digital ulcers in systemic sclerosis. Clin Rheumatol 41:95–104. https://doi.org/10.1007/s10067-021-05900-7
Momeni A, Sorice SC, Valenzuela A et al (2015) Surgical treatment of systemic sclerosis - is it justified to offer peripheral sympathectomy earlier in the disease process? Microsurgery 35:441–446. https://doi.org/10.1002/micr.22379
Nagaraja V, Spino C, Bush E et al (2019) A multicenter randomized, double-blind, placebo-controlled pilot study to assess the efficacy and safety of riociguat in systemic sclerosis-associated digital ulcers. Arthritis Res Ther 21:202. https://doi.org/10.1186/s13075-019-1979-7
Hassanien M, Rashad S, Mohamed N et al (2018) Non-invasive oxygen-ozone therapy in treating digital ulcers of patients with systemic sclerosis. Acta Reumatol Port 43:210–216
Kaymaz S, Karasu U, Alkan H et al (2022) Efficacy of local oxygen–ozone therapy for the treatment of digital ulcer refractory to medical therapy in systemic sclerosis: a randomized controlled study. Mod Rheumatol 32:1102–1107. https://doi.org/10.1093/mr/roab117
Ortega MA, Fraile-Martinez O, García-Montero C et al (2021) A general overview on the hyperbaric oxygen therapy: applications, mechanisms and translational opportunities. Medicina (Lithuania) 57:864
Mirasoglu B, Bagli BS, Aktas S (2017) Hyperbaric oxygen therapy for chronic ulcers in systemic sclerosis – case series. Int J Dermatol 56:636–640. https://doi.org/10.1111/ijd.13570
Gerodimos C, Stefanidou S, Kotsiou M, Melekos T, Mesimeris T (2013) Hyperbaric oxygen treatment of intractable ulcers in a systemic sclerosis patient. Aristotle University Medical Journal. Aristotle University Medical Journal 40:20–22
Saito S, Ishii T, Kamogawa Y et al (2015) Extracorporeal shock wave therapy for digital ulcers of systemic sclerosis: a phase 2 pilot study. Tohoku Journal of Experimental Medicine 238:39–47. https://doi.org/10.1620/tjem.238.39
Hughes M, Moore T, Manning J et al (2019) A feasibility study of a novel low-level light therapy for digital ulcers in systemic sclerosis. Journal of Dermatological Treatment 30:251–257. https://doi.org/10.1080/09546634.2018.1484875
Korsten P, Müller GA, Rademacher JG et al (2019) Rheopheresis for digital ulcers and Raynaud’s phenomenon in systemic sclerosis refractory to conventional treatments. Front Med (Lausanne) 6:208. https://doi.org/10.3389/fmed.2019.00208
Rademacher JG, Tampe B, Borisch A et al (2022) Study protocol: a randomized controlled prospective single-center feasibility study of Rheopheresis for Raynaud’s syndrome and digital ulcers in systemic sclerosis (RHEACT Study). Front Med 9:871744. https://doi.org/10.3389/fmed.2022.871744
Keret S, Slobodin G, Awisat A et al (2022) G- CSF treatment for refractory digital ulcers in systemic sclerosis. Joint Bone Spine 89:105348. https://doi.org/10.1016/j.jbspin.2022.105348
Hughes M, Bruni C, Ruaro B et al (2021) Digital ulcers in systemic sclerosis. Presse Med 50:104064. https://doi.org/10.1016/j.lpm.2021.104064
Kowal-Bielecka O, Fransen J, Avouac J et al (2017) Update of EULAR recommendations for the treatment of systemic sclerosis. Ann Rheum Dis 76:1327–1339. https://doi.org/10.1136/annrheumdis-2016-209909
Hachulla E, Hatron PY, Carpentier P et al (2016) Efficacy of sildenafil on ischaemic digital ulcer healing in systemic sclerosis: the placebo-controlled SEDUCE study. Ann Rheum Dis 75:1009–1015. https://doi.org/10.1136/annrheumdis-2014-207001
Fernández-Codina A, Kazem M, Pope JE (2020) Possible benefit of tadalafil cream for the treatment of Raynaud’s phenomenon and digital ulcers in systemic sclerosis. Clin Rheumatol 39:963–965
Perković D, Petrić M, Božić I et al (2021) Low dose intravenous immunoglobulin in addition to cyclophosphamide in systemic sclerosis: single centre experience. Wien Klin Wochenschr 133:1070–1075. https://doi.org/10.1007/s00508-020-01669-y
Inoue T, Yamaoka T, Murota H et al (2014) Effective oral psoralen plus ultraviolet a therapy for digital ulcers with revascularization in systemic sclerosis. Acta Derm Venereol 94:250–251
Funding
Open access funding provided by HEAL-Link Greece.
Author information
Authors and Affiliations
Contributions
IS performed the literature search. IS and DD jointly drafted the manuscript
Corresponding author
Ethics declarations
Competing interests
DD has received speaking fees and an honorarium for participation in an advisory board from ELPEN. All other authors have disclosed no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Part of the Topical Collection entitled ‘Cardiovascular Issues in Rheumatic Diseases’’
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sagonas, I., Daoussis, D. Treatment of digital ulcers in systemic sclerosis: recent developments and future perspectives. Clin Rheumatol 42, 2589–2599 (2023). https://doi.org/10.1007/s10067-023-06511-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-023-06511-0