Abstract
Introduction
To describe clinical characteristics of patients in Japan with coronavirus disease 19 (COVID-19) and pre-existing rheumatic disease and examine the possible risk factors associated with severe COVID-19.
Methods
Adults with rheumatic disease and a COVID-19 diagnosis who were registered in the COVID-19 Global Rheumatology Alliance (C19-GRA) physician-reported registry from Japan between 15 May 2020 and 12 May 2021 were included. Multivariable logistic regression models were used to assess factors associated with severe COVID-19 progression, defined as death or requiring oxygen inhalation.
Results
In total, 222 patients were included in the study. Rheumatoid arthritis (48.2%), gout (14.4%), and systemic lupus erythematosus (8.1%) were the most common types of rheumatic disease, 55.1% of patients were in remission and 66.2% had comorbid disease. Most patients were hospitalised (86.9%) for COVID-19, 43.3% received oxygen, and 9.0% died. Older age (≥ 65 years), corticosteroid use, comorbid diabetes, and lung diseases are associated with higher risk for severe COVID-19 progression (odds ratio (OR) 3.52 [95% confidence interval (CI) 1.69–7.33], OR 2.68 [95% CI 1.23–5.83], OR 3.56 [95% CI 1.42–8.88], and OR 2.59 [95% CI 1.10–6.09], respectively).
Conclusions
This study described clinical characteristics of COVID-19 patients with rheumatic diseases in Japan. Several possible risk factors for severe COVID-19 progression were suggested.
Key points |
|---|
• Clinical characteristics of 222 adult patients in Japan with coronavirus disease 19 (COVID-19) and pre-existing rheumatic diseases were described. |
• Most patients were hospitalised (86.9%) for COVID-19 in Japan, 43.3% received oxygen, and 9.0% died. |
• The COVID-19 characteristics of patients with rheumatic diseases did not show any obvious different pattern from those of the general population in Japan. |
• In this study, older age (≥ 65 years), corticosteroid use, comorbid diabetes, and lung diseases are associated with higher risk for severe COVID-19 progression. |
Similar content being viewed by others
Introduction
Severe acute respiratory syndrome-associated coronavirus 2 (SARS-CoV-2) has spread rapidly since December 2019, resulting in the coronavirus disease 19 (COVID-19) global pandemic with significant morbidity and mortality [1]. Patients with chronic health conditions such rheumatic diseases, where they may be receiving immunosuppressive therapy, may be more vulnerable to infection and developing a more severe form of COVID-19. However, the current evidence is not clear, and the European Alliance of Associations for Rheumatology (EULAR) has advised that there is no evidence to support that patients with rheumatic musculoskeletal diseases have a higher risk of contracting SARS-CoV-2 or that they have a worse prognosis with COVID-19 [2,3,4,5]. On the other hand, it has been reported that SARS-CoV-2 infection leads to a hypersensitive response of the immune system in the later stage of COVID-19, which might lead to death or a severe outcome. Besides corticosteroids, antirheumatics such as IL-6 inhibitors and Janus kinase (JAK) inhibitors are recommended as treatment options for severe COVID-19 [6, 7].
In March 2020, the COVID-19 Global Rheumatology Alliance (C19-GRA) was formed to rapidly collect and disseminate information about the course of COVID-19 in patients with rheumatic disease and those being administered immunosuppressive medications [8,9,10]. Initial findings from the C19-GRA registry using data mainly from the USA and Europe highlighted several factors that were associated with an increased risk of hospitalisation, including older age, presence of comorbidities, and higher glucocorticoid dosage (≥ 10 mg/day of prednisolone equivalent) [11,12,13].
In Japan, the number of COVID-19 cases and deaths per population has been relatively low compared with Western countries [14], despite the fact that Japan has one of the most aged populations [15] and a high population density. The reasons for this are unclear, and information specific to the rheumatology population in Japan is currently unknown. Given the current absence of information regarding the course of COVID-19 in patients with rheumatic diseases in Japan, we conducted this study to describe the clinical characteristics of rheumatic disease patients with a diagnosis of COVID-19 in Japan and examine the possible risk factors associated with progression to severe COVID-19, defined as death or requiring oxygen inhalation.
Methods
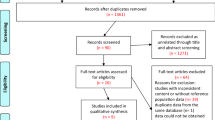
Study design and patients: This was a retrospective, multicentre, observational study that used data from the C19-GRA physician-reported registry. In total, 79 hospitals and 19 clinics in Japan joined this study as a grass-root movement, and upon experiencing COVID-19 cases with underlying rheumatic diseases, they consequently registered all cases into this registry. A COVID-19 diagnosis was based on either polymerase chain reaction testing, antibody status, metagenomic testing, computed tomography scans, laboratory assays, or symptoms only [16].
The C19-GRA physician-reported registry was launched on 24 March 2020 and has been reported previously [8,9,10, 17]. In brief, registry data was collected voluntarily through a survey available to clinicians on the registry website (https://rheum-covid.org/). No patient identifiers, such as name or date of birth, were collected, and only de-identified information was captured by the survey. The data collected on case report forms included patient demographics, rheumatic disease phenotypes, physician-reported disease activities, comorbidities, usage of immunosuppressants and other drug therapies, COVID-19 phenotypes, treatments, and outcomes [8,9,10, 17].
A total of 222 adults who were residing in Japan registered in the C19-GRA physician-reported registry between 15 May 2020 and 12 May 2021 (diagnosed with COVID-19 between 1 January 2020 and 31 December 2020) were included in this study. Due to limited number of death cases, the primary outcome of interest was progression to severe COVID-19. Using the WHO severity definition, a low oxygen saturation (< 90% on room air) or severe respiratory distress [18], severe COVID-19 was defined as oxygen inhalation or death in this study. Oxygen status nor survival was not known for 13 cases, and these were excluded from the outcome analysis.
Ethical approval: The C19-GRA physician-reported registry was approved by the University of California, San Francisco Institutional Review Board as exempt research based on qualification as quality improvement/surveillance research, and not ‘human subjects research’. This observational study of data for patients from Japan in the C19-GRA physician-reported registry was approved by the Ethics Committee of Toho University Omori medical centre (M20137 20,041 20,018).
Data analysis: Frequency (number and percentage [%]) was calculated for categorical variables, and summary statistics (median and interquartile range [IQR] or mean and standard deviation (SD)) were calculated for continuous data. The background factors of patients who progressed to severe COVID-19 versus those who did not were compared and P values were calculated using the Wilcoxon rank-sum test (for continuous variables) or chi-squared test (for categorical variables). Data were considered statistically significant for P values < 0.05. The odds ratios (OR) for both progression to severe disease and death as an outcome were analysed using a univariate logistic regression model and were reported alongside the corresponding 95% confidence intervals (CIs). For the multivariable logistic regression model for which progression to severe disease was an outcome, covariates included in the model were age, sex, and background factors with significant differences in the univariate analysis (with regards to complications, each were included separately), and risk factors identified in former studies [13, 19, 20]. For the multivariable logistic regression model for which death was an outcome, sex, age, and rheumatic disease classification or type of therapeutic agent for rheumatic diseases were included as variables. STATA version 16 (StataCorp LLC, College Station, TX, USA) was used for all analyses.
Results
Patients
A total of 222 adult patients in Japan with rheumatic disease and COVID-19 that was diagnosed between 1 January 2020 and 31 December 2020 were registered in the C19-GRA physician-reported registry between 15 May 2020 and 12 May 2021. Baseline demographic and clinical characteristics of these 222 patients are summarised in Table 1. The mean (SD) patient age was 63 (62.7 ± 14.6) years, 44.6% (99/222) were male, and 98.7% (219/222) were East Asian. Majority of cases (80.2% [166/207]) were from Kanto region. Of the 189 patients with available data on smoking history, 44.4% (84/189) were current or ex-smokers. The most common types of rheumatic disease in this population were rheumatoid arthritis (48.2% [107/222]), gout (14.4% [32/222]), and systemic lupus erythematosus (8.1% [18/222]). Most patients were reported to be in remission (55.1% [114/207]), although a low, moderate, or high level of disease activity was reported in 35.8% (74/207), 6.8% (14/207), and 2.4% (5/207) of patients, respectively (Table 1). The majority of patients had a comorbid disease (66.2% [147/222]). Key comorbidities included hypertension (32.9% [73/222]), diabetes mellitus (22.5% [50/222]), and a spectrum of lung diseases (23.0% [51/222]), including COPD/asthma (11.7% [26/222]) and intestinal lung disease (10.8% [24/222]) (Table 1).
Treatments for underlying rheumatic diseases
At the time of COVID-19 diagnosis, the treatments that patients were receiving for rheumatic disease included corticosteroids (45.5% [100/220]), conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) (44.1% [98/222]), biologic disease-modifying antirheumatic drugs (bDMARDs) (15.3% [34/222]), and JAK inhibitors (1.4% [3/222]) (Table 2). Most patients who were receiving bDMARDs or JAK inhibitors discontinued treatment after the onset of COVID-19 (81.8% [27/33], 100% [3/3], respectively) (Table 2).
COVID-19 characteristics and outcomes
Regarding the infection acquisition, 47.3% (105/222) of patients had a community-acquired infection of route unknown, 48.2% (107/222) of patients reported it was from a close contact, either at home or in the workplace, and 7.7% (17/222) of patients reported as healthcare-associated infection (Table 3). The most common diagnosis method was by polymerase chain reaction (91.9% [204/222]). CT was used for 18.9% [42/222] of patients. The common disease symptoms were fever (88.2% [165/187]) and cough (49.7% [93/187]). Most of the patients did not have complications (82.4% [183/222]), but 8.6% (19/222) of patients developed ARDS. The common treatment administered for COVID-19 was either corticosteroids (33.8% [75/222]), favipiravir (27.0% [60/222]), or remdesivir (23.4% [52/222]) (Table 3). Although most patients (83.8% [181/216]) recovered from COVID-19, 86.9% (186/214) of patients were hospitalised and 43.3% (90/208) required oxygen therapy. Death occurred in 9.0% (20/222) of patients. Overall, 96 patients had progression to severe COVID-19 (Table 3).
COVID-19 outcomes, mortality, the proportion of patients who progressed to severe disease (required oxygen inhalation or died), and the proportion of patients who progressed critical disease (required ventilation or extracorporeal membrane oxygenation, or died) by age groups are shown in Online supplementary Table 1. All these proportions increased with ages from 60s to older than 80 years old; mortality was 8.3% (4/48), 11.5% (6/52), 28.6% (8/28); the proportion of patients who progressed to severe disease was 52.3% (23/48), 59.2% (29/52), and 64.3% (18/28); the proportion who progressed to critical disease was 15.9% (7/48), 16.3% (8/52), 35.7% (10/28) in 60–69, 70–79, ≥ 80 years old, respectively.
Factors associated with progression to severe COVID-19
Comparison of clinical characteristics of 96 patients who progressed to severe COVID-19 (defined as requiring oxygen administration or death) versus 113 patients who did not using univariate analysis is shown in Table 4. Patients who progressed to severe disease were older and had more comorbidities. Especially, hypertension, diabetes mellitus, lung diseases (including COPD/asthma and intestinal lung disease) were more common among the patients who progressed to severe disease. A higher percentage of patients who progressed to severe disease were administered corticosteroids (56.3% [54/96]) than those who did not (38.7% [43/111]).
When adjusting for baseline factors, a multivariable analysis showed that older age (≥ 65 years) (OR 3.52 [95% CI 1.69–7.33], corticosteroid use (OR 2.68 [95% CI 1.23–5.83]), comorbid diabetes (OR 3.56 [95% CI 1.42–8.88]), and lung diseases (OR 2.59 [95% CI 1.10–6.09]) remained independently associated with a greater risk of progression to severe disease (all P < 0.05; Table 5). Neither underlying rheumatic disease categories, disease activities of rheumatic diseases, nor other medications than corticosteroids for rheumatic diseases showed statistically significant association in this model.
Factors associated with COVID-19-related death
Clinical characteristics of 20 deceased patients were compared to 202 not deceased patients by univariate analysis (Table 6). Patients who died were older (mean ± SD 75.0 ± 13.4 years old) than those survived (61.5 ± 14.2 years old). More patients who died used corticosteroids (70.0% [14/20]) than those who did not (43.0% [86/200]). Higher percentage of patients who died had at least one comorbidity (90.0% [18/20]) than those who did not (63.9% [129/202]). Comorbid chronic kidney dysfunction and hepatic disease were more common among the deceased patients (20.0% [4/20] and 15.0% [3/20]) than the survived patients (4.0% [8/202] and 3.0% [6/202]) (all P < 0.05).
When adjusting by sex and age using the presence of underlying rheumatic disease or medications for rheumatic disease, a multivariable analysis showed that only older age (≥ 65 years) remained associated with an increased risk of death (P < 0.05; Online Supplementary Tables 2 and 3).
Discussion
This multicentre, observational study using data from the C19-GRA physician-reported registry of adults with rheumatic diseases and COVID-19 enabled description of the clinical characteristics and management of affected patients in Japan. The COVID-19 characteristics including route of infection, common symptoms, and complications of patients with rheumatic diseases in Japan did not show any obvious different pattern from those of the general populations in Japan and China [21,22,23]. Treatment pattern for COVID-19 might be different in Japan from western countries. In the USA, hydroxychloroquine and chloroquine were prescribed for COVID-19 frequently under the emergency use authorization because of the potential benefits [24, 25]. In Japan, instead of hydroxychloroquine and chloroquine, it was expected that favipiravir would have an antiviral effect against SARS-CoV-2 [26], and so, favipiravir was frequently administered for COVID-19 in 2020 [21] although it had not been approved for use in patients with COVID-19. In this study, antimalarials such as hydroxychloroquine were administered for only 2.3% (5/222) and 27.0% (60/222) patients were administered favipiravir. In Japan, remdesivir was approved for the treatment of COVID-19 on 7 May 2020 [27], however, because of insufficient drug stocks, it was not widely used at the time. In this study, 23.4% (52/222) were treated with remdesivir.
Regarding COVID-19 outcomes, this analysis showed that both the mortality and severe disease progression were worse with increasing age, which is compatible to the published data from the overall population (i.e., those with and without rheumatic diseases) [21, 22, 28]. While differences in the databases do not allow direct comparison between studies, COVID-19 mortality and proportion of patients who progressed to severe COVID-19 among hospitalized patients in this study were numerically higher than those reported from the general population by the Ministry of Health, Labour, and Welfare (MHLW) in Japan up to 6 January 2021, both overall and in each age group [28]. The MHLW reported mortality 0.0%, 0.0%, 0.1%, 0.3%, 1.4%, 12.3%, and 1.4% and severe COVID-19 (treated in an intensive care unit or required ventilation or extracorporeal membrane oxygenation) progression 0.0%, 0.0%, 0.5%, 1.4%, 3.0%, 4.1%, 2.0%, and 1.2% in 20–29, 30–39, 40–49, 50–59, 60–69, 70–79, ≥ 80 years old, and overall, respectively. Online supplementary Table 1 shows the most comparable data in our study to the MHLW data, given that we utilised the same age group stratification, a similar definition of progression to severe disease, and close data cut-off date. This numerical difference between the population in our study and the general population accords with a published report of COVID-19 outcome data from immunosuppressed inpatients in Japan, including those with connective tissue diseases and those being treated with immunosuppressive agents, in which a higher proportion of deaths in patients with connective tissue diseases (16.5%) versus non-immunosuppressed patients (3.2%) was found [29]. However, this study did not adjust for other risk factors, including age or sex. A cross-sectional investigation using IORRA cohort in Japan reported that 46 self-reported COVID-19 cases with RA were relatively younger, with lower disease activity and better physical function, compared to 2915 non-COVID-19 with RA cases. Because none of the COVID-19 cases presented pneumonia nor required hospitalization, characteristics of severe COVID-19 cases with RA were not assessed in this report [30].
At the closest cut-off point to our analysis, 6300 cases with underlying rheumatic diseases were registered in the total population of the C19-GRA physician-reported registry globally [31]. Among those, the proportion of elderly people (> 65 years old) was 21.5% (1355/6300), which is lower than our study population which itself was almost half occupied by 65 years and older (46.9% [104/222]). The three most common rheumatic diseases in the global population were rheumatoid arthritis (41.1% [2586/6300]), systemic lupus erythematosus (17.7% [1117/6300]), and psoriatic arthritis (8.3% [522/6300]), in cases registered from Japan, the three most common were rheumatoid arthritis (48.2% [107/222]), gout (14.4% [32/222]), and systemic lupus erythematosus (8.1% [18/222]) (Table 1). The percentage of gout was much lower in the total C19-GRA physician-reported registry population (2.6% [165/6300]). Given a known side effect of favipiravir, a common treatment option for COVID-19 in Japan, is hyperuricemia [32], clinicians tend to specifically check for a history of gout in COVID-19 patients, which may have been a possible explanation for the elevated proportion of patients with gout in this analysis.
While corticosteroids were used by a somewhat higher proportion of patients in the cases from Japan versus the total population usage, biologic DMARD and JAK inhibitor administration at the onset of COVID-19 was lower in Japan than the overall (corticosteroids 45.5% [100/220] versus 33.2% [2094/6300]; biologic DMARDs 15.3% [34/222] versus 31.4% [1977/6300]; JAK inhibitors 1.4% [3/222] versus 4.6% [290/6300]). There was a somewhat higher proportion of patients with comorbidities in cases from Japan versus the total population (66.2% versus 50.9% [3207/6300]), while the common comorbid conditions were similar, hypertension (32.9% [73/222] versus 35.1% [2209/6300]), comorbid lung diseases (23.0% [51/222] versus 15.6% [984/6300]), and diabetes mellitus (22.5% [50/222] versus 14.5% [916/6300]) [31].
Among the cases included in the total C19-GRA physician-reported registry population, most recovered (86.2% [5431/6300]), 31.1% (1959/6300) were hospitalised, 28.5% (1795/6300) required oxygen inhalation, 5.1% (324/6300) required a ventilator or ECMO, and 5.8% (362/6300) died [31]. The proportion of cases that resulted in death, hospitalisation, and oxygen or ventilator usage were numerically higher in patients from Japan than the global data; however, these results should be interpreted with caution because of the baseline characteristic difference as mentioned above. Additionally, there is a potential selection bias of patients entered into the C19-GRA physician-reported registry. Moreover, the way that patient information was collected differed from country to country. In Japan, all patients who tested positive for SARS-CoV-2 infection were isolated per the Infectious Disease Control Law and those with underlying conditions, including rheumatic diseases, were recommended for hospitalisation. In 2020, hospital bed capacity allowed them to be hospitalized. Further, polymerase chain reaction testing was reserved for patients with symptoms of COVID-19 or who were in close contact with others experiencing COVID-19 symptoms [33], likely leading to less detection of asymptomatic cases. These differences make direct comparison between countries difficult even from within the same registry.
On the other hand, a meta-analysis of 31 reports of COVID-19 in patients with rheumatic diseases found that COVID-19-related hospitalisation rates were similar in Asia, Europe, and North America (60% [95% CI 41–77%], 62% [51–73%], and 50% [37–64%], respectively) though the fatality rate after hospitalisation was higher in Europe (19% [15–24%]) than in Asia (11% [2–23%]) and North America (12% [6–19%]) [34]. They reported that the rates of oxygen support, intensive care unit (ICU) admission, and death were 33% (95% CI 21–47%), 9% (5–15%), and 7% (3–11%), respectively, in overall, which were similar figures to our findings.
In this study, older age (≥ 65 years), corticosteroid use, and comorbid diabetes and lung diseases were suggested as possible risk factors for severe COVID-19 outcomes in patients with rheumatic disease, which were reported as association with COVID-19-related hospitalization or death in previous report of C19-GRA cases [11,12,13], other cohort studies [35,36,37], and a meta-analysis in patients with rheumatic diseases [38]. Other than these factors we suggested, previous C19-GRA reports suggested that comorbid hypertension/cardiovascular disease and chronic renal insufficiency were associated with higher odds of hospitalisation [11] and male sex and higher disease activity were associated with higher odds of death [13]. In our study, although in the multivariable model male sex and comorbid hypertension did not show a statistically strong association, in univariate analysis, they showed statistically strong association to severe COVID-19. Association of disease activity with severe disease in our study was not clear because the number of cases whose physician reported having higher than moderate disease activity was limited.
Previous reports suggested association of biologic DMARDs with severe COVID-19 outcome [11, 12, 36, 38,39,40],; however, the relationship of biologic DMARDs or JAK inhibitor usage with COVID-19 outcomes is not clear currently. A report from the first 600 cases from the C19-GRA physician-reported registry suggested that the use of tumour necrosis factor (TNF) inhibitors may reduce the probability of hospitalisation [11]. A later analysis that included 2869 cases from the C19-GRA suggested that JAK inhibitors or rituximab treatment resulted in worse COVID-19 outcomes compared with patients treated with TNF inhibitors, there were no associations between treatment with abatacept or IL-6 inhibitors and COVID-19 severity [12]. This association of JAK inhibitor treatment and worse COVID-19 outcomes was consistent with a New York University cohort study [39], though another cohort study conducted in the USA reported that rituximab users had a higher risk of hospitalisation compared with patients treated with TNF inhibitors and found no significant difference between those treated with JAK inhibitors and TNF inhibitors [40]. These inconsistent results may be explained by differences in confounding factors assessed in analyses or the timing of drug usage during COVID-19. In this analysis, patients receiving biologic DMARDs or JAK inhibitors had lower point estimate for adjusted odds of severe disease progression compared to patients without DMARDs or immunosuppressant,; however, there was no statistical significance (adjusted OR 0.58 [95% CI 0.18–1.84] (Table 5). Although analysis of outcomes according to individual drug classes would be ideal, this was not possible in our study because of limited numbers of patients for such individual drugs. Future studies with larger samples would be more informative.
This current study has several limitations, including a relatively small number of patients and mortality events and a potential for reporting bias of more severe cases. This study is voluntary, and there was a biased distribution with data mainly from tertiary care centres near Tokyo in the Kanto region, which results that our data is not well representative of the whole rheumatology population in Japan and thus limits the generalisability of the results. Additionally, a comparison between our study data from Japan with those from other countries was limited due to selection bias related to different data collection methods, health policy and systems. Finally, this study was based on preliminary data that was collected in 2020, before new variants of COVID-19 (e.g., alpha, delta or omicron) became prevalent, and before COVID-19 vaccines became available in Japan. However, this study allows us to fill the current information gap of the clinical characteristics of COVID-19 among patients with rheumatic diseases in Japan.
In conclusion, this retrospective, multicentre, observational study using data from the C19-GRA physician-reported registry has shown the clinical characteristics of patients with underlying rheumatic disease and diagnosed COVID-19 in Japan. Older age (≥ 65 years), corticosteroid use and comorbid diabetes and lung diseases are suggested as possible risk factors for severe COVID-19 disease progression.
References
Fauci AS, Lane HC, Redfield RR (2020) Covid-19—navigating the uncharted. N Engl J Med 382(13):1268–1269. https://doi.org/10.1056/NEJMe2002387
Furst DE (2010) The risk of infections with biologic therapies for rheumatoid arthritis. Semin Arthritis Rheum 39(5):327–346. https://doi.org/10.1016/j.semarthrit.2008.10.002
D’Silva KM, Wallace ZS (2021) COVID-19 and rheumatoid arthritis. Curr Opin Rheumatol 33(3):255–261. https://doi.org/10.1097/BOR.0000000000000786
Liu Y, Sawalha AH, Lu Q (2021) COVID-19 and autoimmune diseases. Curr Opin Rheumatol 33(2):155–162. https://doi.org/10.1097/BOR.0000000000000776
Landewé RBM, Kroon FPB, Alunno A et al (2022) EULAR recommendations for the management and vaccination of people with rheumatic and musculoskeletal diseases in the context of SARS-CoV-2: the November 2021 update. Annals of the rheumatic diseases, annrheumdis-2021–222006. Advance online publication. https://doi.org/10.1136/annrheumdis-2021-222006
Nissen CB, Sciascia S, de Andrade D et al (2021) The role of antirheumatics in patients with COVID-19. The Lancet Rheumatology 3(6):e447–e459. https://doi.org/10.1016/S2665-9913(21)00062-X
National Institutes of Health (2022) COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. https://www.covid19treatmentguidelines.nih.gov/. Accessed 9 July 2022.
Robinson PC, Yazdany J (2020) The COVID-19 Global Rheumatology Alliance: collecting data in a pandemic. Nat Rev Rheumatol 16(6):293–294. https://doi.org/10.1038/s41584-020-0418-0
Gianfrancesco MA, Hyrich KL, Gossec L et al (2020) Rheumatic disease and COVID-19: initial data from the COVID-19 global rheumatology alliance provider registries. The Lancet Rheumatol 2(5):e250–e253. https://doi.org/10.1016/S2665-9913(20)30095-3
Liew JW, Bhana S, Costello W et al (2021) The COVID-19 Global Rheumatology Alliance: evaluating the rapid design and implementation of an international registry against best practice. Rheumatology (Oxford) 60(1):353–358. https://doi.org/10.1093/rheumatology/keaa483
Gianfrancesco M, Hyrich KL, Al-Adely S et al (2020) Characteristics associated with hospitalisation for COVID-19 in people with rheumatic disease: data from the COVID-19 Global Rheumatology Alliance physician-reported registry. Ann Rheum Dis 79(7):859–866. https://doi.org/10.1136/annrheumdis-2020-217871
Sparks JA, Wallace ZS, Seet AM et al (2021) Associations of baseline use of biologic or targeted synthetic DMARDs with COVID-19 severity in rheumatoid arthritis: results from the COVID-19 Global Rheumatology Alliance physician registry. Ann Rheum Dis 80(9):1137–1146. https://doi.org/10.1136/annrheumdis-2021-220418
Strangfeld A, Schäfer M, Gianfrancesco MA et al (2021) Factors associated with COVID-19-related death in people with rheumatic diseases: results from the COVID-19 Global Rheumatology Alliance physician-reported registry. Ann Rheum Dis 80(7):930–942. https://doi.org/10.1136/annrheumdis-2020-219498
Ritchie H, Mathieu E, Rodés-Guirao L et al (2022) Coronavirus pandemic (COVID-19). https://ourworldindata.org/coronavirus. Accessed 1 March 2022.
Statistics Bureau of Japan, Statistics Handbook of Japan, Ministry of Internal Affairs and Communications, Japan, 2021 (2021) https://www.stat.go.jp/english/data/handbook/pdf/2021all.pdf#page=1. Accessed 1 March 2022.
COVID-19 Global Rheumatology Alliance. Rheumatology COVID-19 Provider-Entered Registry (2020) https://rheum-covid.org/downloads/translations/English_rheum-covid-provider-registry.pdf. Accessed 1 March 2022.
Wallace ZS, Bhana S, Hausmann JS et al (2020) The rheumatology community responds to the COVID-19 pandemic: the establishment of the COVID-19 global rheumatology alliance. Rheumatology (Oxford) 59(6):1204–1206. https://doi.org/10.1093/rheumatology/keaa191
World Health Organization (2022) Clinical management of COVID-19: Living guideline, 23 June 2022. file://vmg-vdi-ad04/redirect(RDS)/b21200wt/Downloads/WHO-2019-nCoV-Clinical-2022.1-eng.pdf Accessed 10 July 2022.
Landewé RB, Machado PM, Kroon F et al (2020) EULAR provisional recommendations for the management of rheumatic and musculoskeletal diseases in the context of SARS-CoV-2. Ann Rheum Dis 79(7):851–858. https://doi.org/10.1136/annrheumdis-2020-217877
Mikuls TR, Johnson SR, Fraenkel L et al (2020) American College of rheumatology guidance for the management of rheumatic disease in adult patients during the COVID-19 pandemic: version 2. Arthritis & rheumatology 72(9):e1–e12. https://doi.org/10.1002/art.41437
Matsunaga N, Hayakawa K, Terada M et al (2021) Clinical epidemiology of hospitalized patients with coronavirus disease 2019 (COVID-19) in Japan: report of the COVID-19 registry Japan. Clin infectious diseases: an official publ Infectious Diseases Soc America 73(11):e3677–e3689. https://doi.org/10.1093/cid/ciaa1470
Chen N, Zhou M, Dong X et al (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395(10223):507–513. https://doi.org/10.1016/S0140-6736(20)30211-7
Guan WJ, Ni ZY, Hu Y et al (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382(18):1708–1720. https://doi.org/10.1056/NEJMoa2002032
Bull-Otterson L, Gray EB, Budnitz DS et al (2020) Hydroxychloroquine and chloroquine prescribing patterns by provider specialty following initial reports of potential benefit for COVID-19 Treatment — United States, January–June 2020. MMWR Morb Mortal Wkly Rep 69:1210–1215. https://doi.org/10.15585/mmwr.mm6935a4
Food and Drug Administration (2020) Revocation of the EUA Letter June 15, https://www.fda.gov/media/138945/download Accessed 29 April 2022
Wang M, Cao R, Zhang L et al (2020) Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res 30(3):269–271. https://doi.org/10.1038/s41422-020-0282-0
Pharmaceuticals and Medical Devices Agency (2020) Special approval for emergency of remdesivir for COVID-19. https://www.pmda.go.jp/english/int-activities/0004.pdf Accessed 1 May 2022.
Ministry of Health, Labour and Welfare (2021) Domestic outbreak trends of new coronavirus infections (in Japanese). 2021. https://www.mhlw.go.jp/content/10906000/000716059.pdf. Accessed 1 March 2022.
Nomoto H, Suzuki S, Asai Y et al (2022) Clinical characteristics and prognosis of immunosuppressed inpatients with COVID-19 in Japan. J infection chemotherapy: official J Japan Soc Chemotherapy 28(2):224–231. https://doi.org/10.1016/j.jiac.2021.10.021
Tanaka E, Inoue E, Abe M et al (2022) Changes in treatment adherence and behaviour during the COVID-19 pandemic in Japanese patients with rheumatoid arthritis: results from cross-sectional study in the IORRA cohort. Modern rheumatology, roab120. Advance online publication. https://doi.org/10.1093/mr/roab120
COVID-19 Global Rheumatology Alliance (2020) https://rheum-covid.org/. Accessed 1 March 2022.
Mishima E, Anzai N, Miyazaki M et al (2020) Uric acid elevation by favipiravir, an antiviral drug. Tohoku J Exp Med 251(2):87–90. https://doi.org/10.1620/tjem.251.87
Sawano T, Kotera Y, Ozaki A et al (2020) Underestimation of COVID-19 cases in Japan: an analysis of RT-PCR testing for COVID-19 among 47 prefectures in Japan. QJM: monthly J Assoc Physicians 113(8):551–555. https://doi.org/10.1093/qjmed/hcaa209
Xu C, Yi Z, Cai R et al (2021) Clinical outcomes of COVID-19 in patients with rheumatic diseases: a systematic review and meta-analysis of global data. Autoimmun Rev 20(4):102778. https://doi.org/10.1016/j.autrev.2021.102778
Shin YH, Shin JI, Moon SY et al (2021) Autoimmune inflammatory rheumatic diseases and COVID-19 outcomes in South Korea: a nationwide cohort study. Lancet Rheumatol 3(10):e698–e706. https://doi.org/10.1016/S2665-9913(21)00151-X
Ayala Gutiérrez MDM, Rubio-Rivas M, Romero Gómez C et al (2021) Autoimmune diseases and COVID-19 as risk factors for poor outcomes: data on 13,940 hospitalized patients from the Spanish Nationwide SEMI-COVID-19 Registry. J Clin Med 10(9):1844. https://doi.org/10.3390/jcm10091844
Freites Nuñez DD, Leon L, Mucientes A et al (2020) Risk factors for hospital admissions related to COVID-19 in patients with autoimmune inflammatory rheumatic diseases. Ann Rheum Dis 79(11):1393–1399. https://doi.org/10.1136/annrheumdis-2020-217984
Wang Q, Liu J, Shao R et al (2021) Risk and clinical outcomes of COVID-19 in patients with rheumatic diseases compared with the general population: a systematic review and meta-analysis. Rheumatol Int 41(5):851–861. https://doi.org/10.1007/s00296-021-04803-9
Haberman RH, Castillo R, Chen A et al (2020) COVID-19 in patients with inflammatory arthritis: a prospective study on the effects of comorbidities and disease-modifying antirheumatic drugs on clinical outcomes. Arthritis & rheumatol (Hoboken, N.J.) 72(12):1981–1989. https://doi.org/10.1002/art.41456
Raiker R, DeYoung C, Pakhchanian H et al (2021) Outcomes of COVID-19 in patients with rheumatoid arthritis: a multicenter research network study in the United States. Semin Arthritis Rheum 51(5):1057–1066. https://doi.org/10.1016/j.semarthrit.2021.08.010
Acknowledgements
We wish to thank the participants of the study (listed on Online Supplementary File). We thank Sarah Bubeck, PhD, and Nila Bhana, MSc (Hons) of Edanz for providing medical writing support.
Author information
Authors and Affiliations
Contributions
MK conceived the idea of the study and developed the statistical analysis plan and conducted statistical analyses. TN supervised the conduct of this study. MK, MS, HK, SM, SO, and TN contributed to data collection. MK, JA, and TS contributed to the results interpretation. MK drafted the original manuscript. All authors reviewed the manuscript and revised it critically on intellectual content. All authors gave final approval of the manuscript to be published.
Corresponding author
Ethics declarations
Conflict of interest
MK and JA both are employed by Pharmaceuticals and Medical Devices Agency. The views expressed in this article are those of the authors and do not necessarily reflect the official views of Pharmaceuticals and Medical Devices Agency. TS has received research grants and/or honoraria from Abbvie Japan Co., Ltd., AsahiKASEI Co., Ltd., Astellas Pharma Inc., Ayumi Pharmaceutical, Bristol Myers Squibb K.K., Chugai Pharmaceutical Co., Ltd., Daiichi Sankyo., Eli Lilly Japan K.K., Mitsubishi-Tanabe Pharma Co., Ono Pharmaceutical, Pfizer Japan Inc., Takeda Pharmaceutical Co. Ltd., and UCB Japan Co. Ltd. Tokyo Medical and Dental University received unrestricted research grants for Department of Lifetime Clinical Immunology from AbbVie GK, Asahikasei Pharmaceutical Co., AYUMI Pharmaceutical Corporation, Chugai Pharmaceutical Co., Ltd., CSL Behring K.K., Japan Blood Products Organization, Nippon Kayaku Co., Ltd. and UCB Japan Co. Ltd. SM received consultant fees/speakers fees from Asahikasei Pharma Corp., Ono Pharmaceutical Co., Ltd., Eisai Co., Ltd., and Astellas Pharma Inc. TN received grant/research support from Chugai Pharmaceutical Co., Eisai Co., Ltd., Teijin Pharma Ltd., Eli Lilly Japan K.K., Bristol-Myers K.K., Ono Pharmaceutical Co., Ltd., Asahikasei Pharma Corp., Mitsubishi-Tanabe Pharma Co., Ayumi Pharmaceutical Corporation, Shionogi & Co., Ltd., Sanofi K.K., Nippon Kayaku Co., Ltd., AbbVie GK, Nippon Boehringer Ingelheim Co., Ltd., and Taisho Pharmaceutical Co., Ltd., and consultant fees/speakers fees from UCB Japan Co., Ltd., Eisai Co., Ltd., Chugai Pharmaceutical Co., Astellas Pharma Inc., Janssen Pharmaceutical K.K., Pfizer Japan Inc., Asahikasei Pharma Corp., Eli Lilly Japan K.K., Takeda Pharmaceutical Co., Nippon Boehringer Ingelheim Co., Ltd., AbbVie GK., Taisho Pharmaceutical Co., Ltd., Ono Pharmaceutical Co., Ltd., Mochida Pharmaceutical Co., Ltd., GlaxoSmithKline plc., Kyowa Kirin Co., Ltd., and Mylan N.V. All other co-authors have nothing to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kihara, M., Sugihara, T., Asano, J. et al. Clinical characteristics of COVID-19 patients with underlying rheumatic diseases in Japan: data from a multicenter observational study using the COVID-19 Global Rheumatology Alliance physician-reported registry. Clin Rheumatol 41, 3661–3673 (2022). https://doi.org/10.1007/s10067-022-06305-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-022-06305-w