Abstract
Objectives
To evaluate specificity, level, and avidity of antineutrophil cytoplasmic antibodies (ANCA) in systemic lupus erythematosus (SLE). There are no studies of ANCA avidity in SLE.
Methods
Level (ELISA) and avidity (ELISA) of myeloperoxidase (MPO-), proteinase 3 (PR3-), lactoferrin (LF-), cathepsin G, elastase (EL-), and bactericidal/permeability increasing protein (BPI)-ANCA in 142 SLE patients were studied. SLE activity was measured by SLEDAI-2 K. 25/40 ANCA-positive patients were immunoserologically followed (12 ± 2 months).
Results
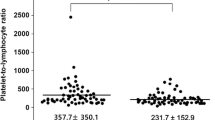
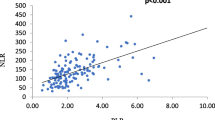
40/142 (28.2%) SLE patients were ANCA-positive: LF- (21/40), MPO- (19/40), EL- (6/40), PR3- (3/40), and BPI-ANCA (1/40). Only LF-ANCA were associated with renal manifestations (p < 0.05), and positive predictive value for renal involvement in ANCA-positive SLE was 76.2%. LF-ANCA-positive patients had higher SLEDAI-2 K (p < 0.05) and more frequently had anti-dsDNA (p < 0.05), low C3 (p < 0.001), and low C4 (p < 0.05) than LF-ANCA-negative patients. LF-ANCA level was in a positive correlation with SLEDAI-2 K, anti-dsDNA, and anti-C1q (p < 0.01) and in a negative correlation with C3 and C4 (p < 0.05). LF-ANCA avidity was higher than MPO-, EL-, PR3-, and BPI-ANCA avidity (p < 0.01). In LF-ANCA-positive patients, renal manifestations were associated with higher LF-ANCA level (p < 0.01) and avidity (p < 0.05). Based on LF-ANCA level and avidity, the receiver operating characteristic curves for discriminating patients with and without renal involvement had areas under the curves of 0.988 (95% CI: 0.949–1.00) and 0.813 (95% CI: 0.607–1.00), respectively. After the follow-up period, number of LF-ANCA-positive patients decreased (p < 0.01).
Conclusions
In contrast to other ANCAs, only LF-ANCA level correlated with activity and standard serological SLE markers. LF-ANCA level and avidity might be biomarkers of renal involvement in SLE. LF-ANCA are promising serological marker in SLE.
Key Points • LF- and MPO-ANCA were most frequently found, while EL-, PR3-, and BPI-ANCA were rarely detected in SLE. • In contrast to other ANCAs, only LF-ANCA were associated with renal involvement, and their level correlated with the activity and standard serological markers of SLE. • LF-ANCA avidity was higher than other ANCAs’ avidity; LF-ANCA level and avidity might be useful biomarkers of renal manifestations in SLE. • Detection of ANCA specificity, level, and avidity may help in the diagnosis of particular clinical SLE phenotypes. |

Similar content being viewed by others
References
Tsokos GC (2020) Autoimmunity and organ damage in systemic lupus erythematosus. Nat Immunol 21(6):605–614. https://doi.org/10.1038/s41590-020-0677-6
Sangaletti S, Tripodo C, Chiodoni C, Guarnotta C, Cappetti B, Casalini P, Piconese S, Parenza M, Guiducci C, Vitali C, Colombo MP (2012) Neutrophil extracellular traps mediate transfer of cytoplasmic neutrophil antigens to myeloid dendritic cells toward ANCA induction and associated autoimmunity. Blood 120(15):3007–3018. https://doi.org/10.1182/blood-2012-03-416156
Garcia-Romo GS, Caielli S, Vega B, Connolly J, Allantaz F, Xu Z, Punaro M, Baisch J, Guiducci C, Coffman RL, Barrat FJ, Banchereau J, Pascual V (2011) Netting neutrophils are major inducers of type I IFN production in pediatric systemic lupus erythematosus. Sci Transl Med 3(73):73ra20. https://doi.org/10.1126/scitranslmed.3001201
Nakazawa D, Tomaru U, Suzuki A, Masuda S, Hasegawa R, Kobayashi T, Nishio S, Kasahara M, Ishizu A (2012) Abnormal conformation and impaired degradation of propylthiouracil-induced neutrophil extracellular traps: implications of disordered neutrophil extracellular traps in a rat model of myeloperoxidase antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum 64(11):3779–3787. https://doi.org/10.1002/art.34619
Podolska MJ, Biermann MH, Maueröder C, Hahn J, Herrmann M (2015) Inflammatory etiopathogenesis of systemic lupus erythematosus: an update. J Inflamm Res 8:161–171. https://doi.org/10.2147/jir.s70325
Okubo K, Kamiya M, Urano Y, Nishi H, Herter JM, Mayadas T, Hirohama D, Suzuki K, Kawakami H, Tanaka M, Kurosawa M, Kagaya S, Hishikawa K, Nangaku M, Fujita T, Hayashi M, Hirahashi J (2016) Lactoferrin suppresses neutrophil extracellular traps release in inflammation. EBioMedicine 10:204–215. https://doi.org/10.1016/j.ebiom.2016.07.012
Schauer C, Janko C, Munoz LE, Zhao Y, Kienhöfer D, Frey B, Lell M, Manger B, Rech J, Naschberger E, Holmdahl R, Krenn V, Harrer T, Jeremic I, Bilyy R, Schett G, Hoffmann M, Herrmann M (2014) Aggregated neutrophil extracellular traps limit inflammation by degrading cytokines and chemokines. Nat Med 20(5):511–517. https://doi.org/10.1038/nm.3547
Pan HF, Fang XH, Wu GC, Li WX, Zhao XF, Li XP, Xu JH, Ye DQ (2008) Anti-neutrophil cytoplasmic antibodies in new-onset systemic lupus erythematosus and lupus nephritis. Inflammation 31(4):260–265. https://doi.org/10.1007/s10753-008-9073-3
Wang Y, Huang X, Cai J, Xie L, Wang W, Tang S, Yin S, Gao X, Zhang J, Zhao J, Huang Y, Li Y, Zhang Y, Zhang J (2016) Clinicopathologic characteristics and outcomes of lupus nephritis with antineutrophil cytoplasmic antibody: a retrospective study. Medicine 95(4):e2580. https://doi.org/10.1097/md.0000000000002580
Galeazzi M, Morozzi G, Sebastiani GD, Bellisai F, Marcolongo R, Cervera R, De Ramòn Garrido E, Fernandez-Nebro A, Houssiau F, Jedryka-Goral A, Mathieu A, Papasteriades C, Piette JC, Scorza R, Smolen J (1998) Anti-neutrophil cytoplasmic antibodies in European patients with systemic lupus erythematosus: prevalence, clinical associations and correlation with other autoantibodies. European Concerted Action on the Immunogenetics of SLE. Clin Exp Rheumatol. 16(5):541–546
Čučnik S, Kveder T, Artenjak A, Ulcova Gallova Z, Swadzba J, Musial J, Iwaniec T, Stojanovich L, Alessandri C, Valesini G, Avčin T, Cohen Tervaert JW, Rozman B, Božič B (2012) Avidity of anti-β2-glycoprotein I antibodies in patients with antiphospholipid syndrome. Lupus 21(7):764–765. https://doi.org/10.1177/0961203312440057
Andrejevic S, Jeremic I, Sefik-Bukilica M, Nikolic M, Stojimirovic B, Bonaci-Nikolic B (2013) Immunoserological parameters in SLE: high-avidity anti-dsDNA detected by ELISA are the most closely associated with the disease activity. Clin Rheumatol 32(11):1619–1626. https://doi.org/10.1007/s10067-013-2330-3
Lee SS, Lawton JW, Chan CE, Li CS, Kwan TH, Chau KF (1992) Antilactoferrin antibody in systemic lupus erythematosus. Br J Rheumatol 31(10):669–673. https://doi.org/10.1093/rheumatology/31.10.669
Caccavo D, Rigon A, Picardi A, Galluzzo S, Vadacca M, Ferri GM, Amoroso A, Afeltra A (2005) Anti-lactoferrin antibodies in systemic lupus erythematosus: isotypes and clinical correlates. Clin Rheumatol 24(4):381–387. https://doi.org/10.1007/s10067-004-1040-2
Chikazawa H, Nishiya K, Matsumori A (2000) Hashimoto K (2000) Immunoglobulin isotypes of anti-myeloperoxidase and anti-lactoferrin antibodies in patients with collagen diseases. J Clin Immunol 4:279–286. https://doi.org/10.1023/a:1006667703202
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40(9):1725. https://doi.org/10.1002/art.1780400928
Petri M, Buyon J, Kim M (1999) Classification and definition of major flares in SLE clinical trials. Lupus 8(8):685–691. https://doi.org/10.1191/096120399680411281
Gladman DD, Ibañez D, Urowitz MB (2002) Systemic lupus erythematosus disease activity index 2000. J Rheumatol 29(2):288–291
Romero-Díaz J, Vargas-Vóracková F, Kimura-Hayama E, Cortázar-Benítez LF, Gijón-Mitre R, Criales S, Cabiedes-Contreras J, Iñiguez-Rodríguez Mdel R, Lara-García EA, Núñez-Alvarez C, Llorente L, Aguilar-Salinas C, Sánchez-Guerrero J (2012) Systemic lupus erythematosus risk factors for coronary artery calcifications. Rheumatology (Oxford) 51(1):110–119. https://doi.org/10.1093/rheumatology/ker307
Kemna MJ, Schlumberger W, van Paassen P, Dähnrich C, Damoiseaux JG, Cohen Tervaert JW (2016) The avidity of PR3-ANCA in patients with granulomatosis with polyangiitis during follow-up. Clin Exp Immunol 185(2):141–147. https://doi.org/10.1111/cei.12796
Bosch X, Guilabert A, Font J (2006) Antineutrophil cytoplasmic antibodies. Lancet (London, England) 368(9533):404–418. https://doi.org/10.1016/s0140-6736(06)69114-9
Gajic-Veljic M, Bonaci-Nikolic B, Lekic B, Skiljevic D, Ciric J, Zoric S, Stojimirovic B, Nikolic M (2015) Importance of low serum DNase I activity and polyspecific anti-neutrophil cytoplasmic antibodies in propylthiouracil-induced lupus-like syndrome. Rheumatology (Oxford) 54(11):2061–2070. https://doi.org/10.1093/rheumatology/kev243
Kyriakidi KS, Tsianos VE, Karvounis E, Christodoulou DK, Katsanos KH, Tsianos EV (2016) Neutrophil anti-neutrophil cytoplasmic autoantibody proteins: bactericidal increasing protein lactoferrin cathepsin and elastase as serological markers of inflammatory bowel and other diseases. Ann Gastroenterol 29(3):258–267. https://doi.org/10.20524/aog.2016.0028
Dobric S, Popovic D, Nikolic M, Andrejevic S, Spuran M, Bonaci-Nikolic B (2011) Anti-neutrophil cytoplasmic antibodies (ANCA) specific for one or several antigens: useful markers for subtypes of ulcerative colitis and associated primary sclerosing cholangitis. Clin Chem Lab Med 50(3):503–509. https://doi.org/10.1515/CCLM.2011.797
Schnabel A, Csernok E, Isenberg DA, Mrowka C, Gross WL (1995) Antineutrophil cytoplasmic antibodies in systemic lupus erythematosus Prevalence specificities and clinical significance. Arthritis Rheum 38(5):633–637. https://doi.org/10.1002/art.1780380509
Nishiya K, Chikazawa H, Nishimura S, Hisakawa N, Hashimoto K (1997) Anti-neutrophil cytoplasmic antibody in patients with systemic lupus erythematosus is unrelated to clinical features. Clin Rheumatol 16(1):70–75. https://doi.org/10.1007/bf02238766
Spronk PE, Bootsma H, Horst G, Huitema MG, Limburg PC, Tervaert JW, Kallenberg CG (1996) Antineutrophil cytoplasmic antibodies in systemic lupus erythematosus. Br J Rheumatol 35(7):625–631. https://doi.org/10.1093/rheumatology/35.7.625
Zhao MH, Liu N, Zhang YK, Wang HY (1998) Antineutrophil cytoplasmic autoantibodies (ANCA) and their target antigens in Chinese patients with lupus nephritis. Nephrol Dial Transplant 13(11):2821–2824. https://doi.org/10.1093/ndt/13.11.2821
Molnár K, Kovács L, Kiss M, Husz S, Dobozy A, Pokorny G (2002) Antineutrophil cytoplasmic antibodies in patients with systemic lupus erythematosus. Clin Exp Dermatol 27(1):59–61. https://doi.org/10.1046/j.0307-6938.2001.00964.x
Sinico RA, Pozzi C, Radice A, Tincani A, Li Vecchi M, Rota S, Comotti C, Ferrario F, D’Amico G (1993) Clinical significance of antineutrophil cytoplasmic autoantibodies with specificity for lactoferrin in renal diseases. Am J Kidney Dis 22(2):253–260. https://doi.org/10.1016/s0272-6386(12)70314-1
Pradhan VD, Badakere SS, Bichile LS, Almeida AF (2004) Anti-neutrophil cytoplasmic antibodies (ANCA) in systemic lupus erythematosus: prevalence, clinical associations and correlation with other autoantibodies. J Assoc Physicians India 52:533–537
Su F, Xiao W, Yang P, Chen Q, Sun X, Li T (2017) Anti-neutrophil cytoplasmic antibodies in new-onset systemic lupus erythematosus. An Bras Dermatol 92(4):466–469. https://doi.org/10.1590/abd1806-4841.20175476
Yu YW, Liu ZR, Xie D, Chen SX, Li HY (2006) Clinical significance of antineutrophil cytoplasmic antibodies in patients with lupus nephritis. Nan Fang Yi Ke Da Xue Xue Bao 26(6):833–836
Jarrot PA, Chiche L, Hervier B, Daniel L, Vuiblet V, Bardin N, Bertin D, Terrier B, Amoura Z, Andrés E, Rondeau E, Hamidou M, Pennaforte JL, Halfon P, Daugas E, Dussol B, Puéchal X, Kaplanski G, Jourde-Chiche N (2016) Systemic lupus erythematosus and antineutrophil cytoplasmic antibody-associated vasculitis overlap syndrome in patients with biopsy-proven glomerulonephritis. Medicine (Baltimore) 95(22):e3748. https://doi.org/10.1097/MD.0000000000003748
Flores-Mendoza G, Sansón SP, Rodríguez-Castro S, Crispín JC, Rosetti F (2018) Mechanisms of tissue injury in lupus nephritis. Trends Mol Med 24(4):364–378. https://doi.org/10.1016/j.molmed.2018.02.003
Fu HL, Hsu TC, Chang CC, Tsay GJ (2001) Antigenic specificity of anti-neutrophil cytoplasmic antibody. J Formos Med Assoc 100(1):35–39
Manolova I, Dancheva M, Halacheva K (2001) Antineutrophil cytoplasmic antibodies in patients with systemic lupus erythematosus: prevalence, antigen specificity, and clinical associations. Rheumatol Int 20(5):197–204. https://doi.org/10.1007/s002960100108
Turner-Stokes T, Wilson HR, Morreale M, Nunes A, Cairns T, Cook HT, Pusey CD, Tarzi RM, Lightstone L (2017) Positive antineutrophil cytoplasmic antibody serology in patients with lupus nephritis is associated with distinct histopathologic features on renal biopsy. Kidney Int 92(5):1223–1231. https://doi.org/10.1016/j.kint.2017.04.029
Chin HJ, Ahn C, Lim CS, Chung HK, Lee JG, Song YW, Lee HS, Han JS, Kim S, Lee JS (2000) Clinical implications of antineutrophil cytoplasmic antibody test in lupus nephritis. Am J Nephrol 20(1):57–63. https://doi.org/10.1159/000013557
Zeng Y, Lin Y, Wang X, Zhang Y, Peng F, Wang J, Jiang L, Liang S, Xiao Y (2020) Assessment of a high-avidity IgG ANAs for the diagnosis and activity prediction of systemic lupus erythematosus. Clin Rheumatol 39(9):2619–2629. https://doi.org/10.1007/s10067-020-05040-4
Yoshida M, Sasaki M, Nakabayashi I, Akashi M, Tomiyasu T, Yoshikawa N, Kojima T, Ohno N, Yamada M (2009) Two types of myeloperoxidase-antineutrophil cytoplasmic autoantibodies with a high affinity and a low affinity in small vessel vasculitis. Clin Exp Rheumatol 27(Suppl 52):S28–S32
Pyo JY, Jung SM, Song JJ, Park YB, Lee SW (2019) ANCA positivity at the time of renal biopsy is associated with chronicity index of lupus nephritis. Rheumatol Int 39(5):879–884. https://doi.org/10.1007/s00296-019-04263-2
Audrain MA, Gourbil A, Muller JY, Esnault LM (1996) Anti-lactoferrin autoantibodies: relation between epitopes and iron-binding domain. J Autoimmun 9(4):569–574. https://doi.org/10.1006/jaut.1996.0076
Funding
This study was supported by the Ministry of Education and Science of the Republic of Serbia, Grant No. 175065 (M Nikolic, B Bonaci-Nikolic, and M Gajic-Veljic). The Ministry of Education and Science of the Republic of Serbia had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
MGV, BL, and BBN contributed to the design and implementation of the research, to the analysis of the results, and to the writing of the manuscript. MN was involved in planning and supervised the work. BS interpreted renal function tests. BL and JL performed the statistical analyses and participated in the interpretation of the results. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mirjana Gajic-Veljic and Branislav Lekic contributed equally to this work.
Rights and permissions
About this article
Cite this article
Gajic-Veljic, M., Lekic, B., Nikolic, M. et al. Level and avidity of antineutrophil cytoplasmic antibodies specific to lactoferrin are useful biomarkers in systemic lupus erythematosus. Clin Rheumatol 41, 709–720 (2022). https://doi.org/10.1007/s10067-021-05926-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-021-05926-x