Abstract
Background
The association between pyoderma gangrenosum (PG) and rheumatoid arthritis (RA) was not investigated in the setting of controlled studies. The risk of PG among patients with RA is not established.
Objective
The study aims to evaluate the magnitude of the association between RA and the subsequent development of PG. Additionally, we aimed to characterize patients with RA-associated PG relative to other patients with PG.
Methods
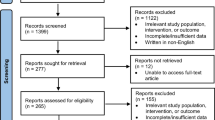
A population-based case-control study was conducted comparing PG patients (n = 302) with age-, sex-, and ethnicity-matched control subjects (n = 1497) with respect to the presence of RA. Logistic regression models were utilized for univariate and multivariate analyses.
Results
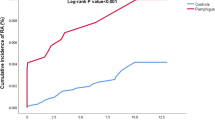
The prevalence of RA was greater in patients with PG than in control subjects (4.7% vs. 1.5%, respectively; P < 0.001). More than threefold increase in the odds of PG with RA (OR, 3.29; 95% CI, 1.66–6.50) was noted. This association retained its statistical significance following a sensitivity analysis excluding RA cases diagnosed up to 2 years prior to PG (OR, 2.72; 95% CI, 1.25–5.91) and after adjusting for confounding factors (adjusted OR, 2.80; 95% CI, 1.23–5.86). RA preceded the diagnosis of PG in the majority of patients by a mean (SD) latency of 9.2 (7.4) years. Patients with RA-associated PG were older relative to the remaining patients with PG (62.2 [15.0] vs. 53.4 [20.9] years, respectively; P = 0.006).
Conclusions
RA increases the odds of developing PG by more than threefold. Physicians managing patients with RA should be aware of this increased burden. Patients with RA may be advised to avoid additional precipitating factors of PG.
Key Points • The odds of developing PG are increased by more than threefold in patients with RA. • PG followed the diagnosis of RA in the majority of patients with these coexistent conditions by an average latency of 9.2 years. • Patients with RA-associated were older relative to other patients with PG at the onset of PG. |

Similar content being viewed by others
References
Braswell SF, Kostopoulos TC, Ortega-Loayza AG (2015) Pathophysiology of pyoderma gangrenosum (PG): an updated review. J Am Acad Dermatol 73:691–698. https://doi.org/10.1016/j.jaad.2015.06.021
Ortega-Loayza AG, Nugent WH, Lucero OM, Washington SL, Nunley JR, Walsh SW (2018) Dysregulation of inflammatory gene expression in lesional and nonlesional skin of patients with pyoderma gangrenosum. Br J Dermatol 178:e35–e36. https://doi.org/10.1111/bjd.15837
Wang EA, Steel A, Luxardi G, Mitra A, Patel F, Cheng MY, Wilken R, Kao J, de Ga K, Sultani H, Merleev AA, Marusina AI, Brassard A, Fung MA, Konia T, Shimoda M, Maverakis E (2018) Classic ulcerative pyoderma gangrenosum is a T cell-mediated disease targeting follicular adnexal structures: a hypothesis based on molecular and clinicopathologic studies. Front Immunol 8. https://doi.org/10.3389/fimmu.2017.01980
Kridin K, Cohen AD, Amber KT (2018) Underlying systemic diseases in pyoderma gangrenosum: a systematic review and meta-analysis. Am J Clin Dermatol 19:479–487. https://doi.org/10.1007/s40257-018-0356-7
Calabresi E, Petrelli F, Bonifacio AF et al (2018) One year in review 2018: pathogenesis of rheumatoid arthritis. Clin Exp Rheumatol
Lora V, Cerroni L, Cota C (2018) Skin manifestations of rheumatoid arthritis. G Ital di Dermatologia e Venereol. https://doi.org/10.23736/S0392-0488.18.05872-8
Sayah A, English JC (2005) Rheumatoid arthritis: a review of the cutaneous manifestations. J Am Acad Dermatol 53:191–209. https://doi.org/10.1016/j.jaad.2004.07.023
Cohen AD, Dreiher J, Regev-Rosenberg S et al (2010) The quality indigators program in Clalit Health Services: the first decade. Harefuah
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Chang K, Yang SM, Kim SH, Han K, Park S, Shin J (2014) Smoking and rheumatoid arthritis. Int J Mol Sci 15:22279–22295. https://doi.org/10.3390/ijms151222279
Manguso F, Sanges M, Staiano T, Gargiulo S, Nastro P, Gargano D, Somma P, Mansueto G, Peluso R, Scarpa R, D'Armiento FP, Astarita C, Ayala F, Renda A, Mazzacca G, D'Arienzo A (2004) Cigarette smoking and appendectomy are risk factors for extraintestinal manifestations in ulcerative colitis. Am J Gastroenterol 99:327–334
States V, O’Brien S, Rai JP et al (2020) Pyoderma gangrenosum in inflammatory bowel disease: a systematic review and meta-analysis. Dig Dis Sci. https://doi.org/10.1007/s10620-019-05999-4
Roberts H, Rai SN, Pan J, Rao JM, Keskey RC, Kanaan Z, Short EP, Mottern E, Galandiuk S (2014) Extraintestinal manifestations of inflammatory bowel disease and the influence of smoking. Digestion. 90:122–129. https://doi.org/10.1159/000363228
Karmiris K, Avgerinos A, Tavernaraki A, Zeglinas C, Karatzas P, Koukouratos T, Oikonomou KA, Kostas A, Zampeli E, Papadopoulos V, Theodoropoulou A, Viazis N, Polymeros D, Michopoulos S, Bamias G, Kapsoritakis A, Karamanolis DG, Mantzaris GJ, Tzathas C, Koutroubakis IE (2016) Prevalence and characteristics of extra-intestinal manifestations in a large cohort of Greek patients with inflammatory bowel disease. J Crohn's Colitis 10:429–436. https://doi.org/10.1093/ecco-jcc/jjv232
Marzano AV, Trevisan V, Lazzari R, Crosti C (2011) Pyoderma gangrenosum: study of 21 patients and proposal of a “clinicotherapeutic” classification. J Dermatol Treat 22:254–260. https://doi.org/10.3109/09546631003686069
Powell FC, Schroeter AL, Su WP, Perry HO (1985) Pyoderma gangrenosum: a review of 86 patients. Q J Med 55:173–186
Adisen E, Erduran F, Gurer MA (2016) Pyoderma gangrenosum: a report of 27 patients. Int J Low Extrem Wounds 15:148–154. https://doi.org/10.1177/1534734616639172
Vidal D, Puig L, Gilaberte M, Alomar A (2004) Review of 26 cases of classical pyoderma gangrenosum: clinical and therapeutic features. J Dermatolog Treat 15:146–152. https://doi.org/10.1080/09546630410031909
Suárez-Pérez JA, Herrera-Acosta E, López-Navarro N, Vilchez-Márquez F, Prieto JD, Bosch RJ, Herrera E (2012) Pyoderma gangrenosum: a report of 15 cases and review of the literature. Actas Dermosifiliogr 103:120–126. https://doi.org/10.1016/j.ad.2011.04.010
Pereira N, Brites MM, Goncalo M et al (2013) Pyoderma gangrenosum--a review of 24 cases observed over 10 years. Int J Dermatol 52:938–945. https://doi.org/10.1111/j.1365-4632.2011.05451.x
Ye MJ, Ye JM (2014) Pyoderma gangrenosum: a review of clinical features and outcomes of 23 cases requiring inpatient management. Dermatol Res Pract 2014:1–7. https://doi.org/10.1155/2014/461467
Saracino A, Kelly R, Liew D, Chong A (2011) Pyoderma gangrenosum requiring inpatient management: a report of 26 cases with follow up. Australas J Dermatol 52:218–221. https://doi.org/10.1111/j.1440-0960.2011.00750.x
Ashchyan HJ, Butler DC, Nelson CA, Noe MH, Tsiaras WG, Lockwood SJ, James WD, Micheletti RG, Rosenbach M, Mostaghimi A (2018) The association of age with clinical presentation and comorbidities of pyoderma gangrenosum. JAMA Dermatology 154:409–413. https://doi.org/10.1001/jamadermatol.2017.5978
Alatab S, Sepanlou SG, Ikuta K, Vahedi H, Bisignano C, Safiri S, Sadeghi A, Nixon MR, Abdoli A, Abolhassani H, Alipour V, Almadi MAH, Almasi-Hashiani A, Anushiravani A, Arabloo J, Atique S, Awasthi A, Badawi A, Baig AAA, Bhala N, Bijani A, Biondi A, Borzì AM, Burke KE, Carvalho F, Daryani A, Dubey M, Eftekhari A, Fernandes E, Fernandes JC, Fischer F, Haj-Mirzaian A, Haj-Mirzaian A, Hasanzadeh A, Hashemian M, Hay SI, Hoang CL, Househ M, Ilesanmi OS, Jafari Balalami N, James SL, Kengne AP, Malekzadeh MM, Merat S, Meretoja TJ, Mestrovic T, Mirrakhimov EM, Mirzaei H, Mohammad KA, Mokdad AH, Monasta L, Negoi I, Nguyen TH, Nguyen CT, Pourshams A, Poustchi H, Rabiee M, Rabiee N, Ramezanzadeh K, Rawaf DL, Rawaf S, Rezaei N, Robinson SR, Ronfani L, Saxena S, Sepehrimanesh M, Shaikh MA, Sharafi Z, Sharif M, Siabani S, Sima AR, Singh JA, Soheili A, Sotoudehmanesh R, Suleria HAR, Tesfay BE, Tran B, Tsoi D, Vacante M, Wondmieneh AB, Zarghi A, Zhang ZJ, Dirac M, Malekzadeh R, Naghavi M (2020) The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet Gastroenterol Hepatol 5:17–30. https://doi.org/10.1016/S2468-1253(19)30333-4
Wolf R, Ruocco V (1998) Nicotine for pyoderma gangrenosum. Arch Dermatol 134:1071–1072. https://doi.org/10.1001/archderm.134.9.1071
Patel GK, Rhodes JR, Evans B, Holt PJA (2004) Successful treatment of pyoderma gangrenosum with topical 0.5% nicotine cream. J Dermatol Treat. https://doi.org/10.1080/09546630310019364
Greenland S, Thomas DC (1982) On the need for the rare disease assumption in case-control studies. Am J Epidemiol 116:547–553. https://doi.org/10.1093/oxfordjournals.aje.a113439
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The ethical committee of Ben-Gurion University approved the current study in accordance with the declaration of Helsinki.
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kridin, K., Damiani, G. & Cohen, A.D. Rheumatoid arthritis and pyoderma gangrenosum: a population-based case-control study. Clin Rheumatol 40, 521–528 (2021). https://doi.org/10.1007/s10067-020-05253-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05253-7