Abstract
Introduction/objectives
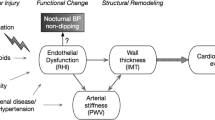
Hypertension management in lupus nephritis (LN) is guided by in-office blood pressure (BP); however, recent studies demonstrate that lupus patients frequently have nocturnal hypertension and reduced BP dipping. The aim of the study was to evaluate 24-h blood pressure in patients with active LN and after response to treatment.
Methods
Seventy active LN patients were evaluated during a LN flare by ambulatory blood pressure monitoring (ABPM). Later, 10 patients with complete response were re-evaluated after 12 months along with 20 matched controls. Overall, daytime and nightime BP, day-to-night dipping, BP load and variability, and the incidence of abnormal BP patterns were assessed. Blood pressure levels were correlated with clinical and histologic parameters and independent associations evaluated by linear regression.
Results
Overall systolic hypertension occurred in 25 (36%) patients and diastolic hypertension in 28 (40%). Nighttime systolic and diastolic hypertension occurred in 35 (50%) and 44 (63%) of patients, respectively. Nocturnal systolic day-to-night BP decrease was abnormal in 59 (84%) patients. Only 18 (26%) were diagnosed with HT by in-office evaluation while 29 (41%) had masked hypertension (MH)/masked uncontrolled hypertension (MUCH), and 3 (4%) had white coat hypertension. Patients with MH had lower eGFR, complement C3, hemoglobin, and higher systolic variability compared with patients with normal BP. Systolic and diastolic BP levels were associated with the years under corticosteroid treatment, activity biomarkers (proteinuria, complement C3), and the degree of interstitial inflammation in the kidney biopsy. A re-evaluation at 12 months showed that although 9 out of 10 patients had normal in-office BP and BP loads improved, still 5 patients remained with MH due to nocturnal hypertension, and 7 remained with abnormal day-to-night dipping. These numbers were higher than those of matched controls.
Conclusions
Due to the high frequency of nocturnal hypertension and abnormal day-to-night dipping, office BP measurements alone may not be sufficient to guide hypertension management in patients with LN.
Key Points • Nocturnal hypertension and abnormal BP patterns are frequent and not detectable by the standard in-office BP evaluation in LN patients. • BP abnormalities may not be fully corrected after a complete clinical response to treatment in lupus nephritis and are only detectable by ABPM. • The degree of interstitial inflammation in the kidney biopsy in LN patients is associated to BP levels. This supports the hypotheses underlining the role of interstitial inflammation in salt sensitivity and hypertension. |


Similar content being viewed by others
References
Fors Nieves CE, Izmirly PM (2016) Mortality in systemic lupus erythematosus: an updated review. Curr Rheumatol Rep 18:21
Mok CC, Kwok RCL, Yip PSF (2013) Effect of renal disease on the standardized mortality ratio and life expectancy of patients with systemic lupus erythematosus. Arthritis Rheum 65:2154–2160
Al-Herz A, Ensworth S, Shojania K, Esdaile JM (2003) Cardiovascular risk factor screening in systemic lupus erythematosus. J Rheumatol 30:493–496
Petri M (2000) Detection of coronary artery disease and the role of traditional risk factors in the Hopkins lupus cohort. Lupus 9:170–175
Sabio JM, Vargas-Hitos JA, Navarrete-Navarrete N, Mediavilla JD, Jiménez-Jáimez J, Díaz-Chamorro A, Jiménez-Alonso J, Grupo Lupus Virgen de las Nieves (2011) Prevalence of and factors associated with hypertension in young and old women with systemic lupus erythematosus. J Rheumatol 38:1026–1032
Tareeva IE, Shvetsov MI, Krasnova TN, Kutyrina IM, Nasonov EL, Kabaenkova GS, Fedorova EI, Shilov EM (1997) Arterial hypertension in lupus nephritis. Ter Arkh 69:13–17
Stojan G, Magder LS, Petri M (2019) Blood pressure variability and age-related blood pressure patterns in systemic lupus erythematosus. J Rheumatol. https://doi.org/10.3899/jrheum.181131
Bertsias GK, Tektonidou M, Amoura Z, Aringer M, Bajema I, Berden JH, Boletis J, Cervera R, Dörner T, Doria A, Ferrario F, Floege J, Houssiau FA, Ioannidis JP, Isenberg DA, Kallenberg CG, Lightstone L, Marks SD, Martini A, Moroni G, Neumann I, Praga M, Schneider M, Starra A, Tesar V, Vasconcelos C, van Vollenhoven R, Zakharova H, Haubitz M, Gordon C, Jayne D, Boumpas DT, European League Against Rheumatism and European Renal Association-European Dialysis and Transplant Association (2012) Joint European League Against Rheumatism and European Renal Association-European Dialysis and Transplant Association (EULAR/ERA-EDTA) recommendations for the management of adult and paediatric lupus nephritis. Ann Rheum Dis 71:1771–1782
KDIGO (2012) KDIGO Clinical Practice Guideline for Glomerulonephritis KDIGO Clinical Practice Guideline for Glomerulonephritis KDIGO Clinical Practice Guideline for Glomerulonephritis. Kidney Int Suppl 2:259–274
Pogue V, Rahman M, Lipkowitz M, Toto R, Miller E, Faulkner M, Rostand S, Hiremath L, Sika M, Kendrick C, Hu B, Greene T, Appel L, Phillips RA, African American Study of Kidney Disease and Hypertension Collaborative Research Group (2009) Disparate estimates of hypertension control from ambulatory and clinic blood pressure measurements in hypertensive kidney disease. Hypertension 53:20–27
Iimuro S, Imai E, Watanabe T, Nitta K, Akizawa T, Matsuo S, Makino H, Ohashi Y, Hishida A, Chronic Kidney Disease Japan Cohort Study Group (2013) Clinical correlates of ambulatory BP monitoring among patients with CKD. Clin J Am Soc Nephrol 8:721–730
Drawz PE, Alper AB, Anderson AH, Brecklin CS, Charleston J, Chen J, Deo R, Fischer MJ, He J, Hsu CY, Huan Y, Keane MG, Kusek JW, Makos GK, Miller ER 3rd, Soliman EZ, Steigerwalt SP, Taliercio JJ, Townsend RR, Weir MR, Wright JT Jr, Xie D, Rahman M, Chronic Renal Insufficiency Cohort Study Investigators (2016) Masked hypertension and elevated nighttime blood pressure in CKD: prevalence and association with target organ damage. Clin J Am Soc Nephrol 11:642–652
Bobrie G, Chatellier G, Genes N, Clerson P, Vaur L, Vaisse B, Menard J, Mallion J-M (2004) Cardiovascular prognosis of “masked hypertension” detected by blood pressure self-measurement in elderly treated hypertensive patients. JAMA 291:1342–1349
Agarwal R, Andersen MJ (2006) Prognostic importance of clinic and home blood pressure recordings in patients with chronic kidney disease. Kidney Int 69:406–411
Mancia G, Facchetti R, Bombelli M, Grassi G, Sega R (2006) Long-term risk of mortality associated with selective and combined elevation in office, home, and ambulatory blood pressure. Hypertension 47:846–853
Fagard RH, Cornelissen VA (2007) Incidence of cardiovascular events in white-coat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens 25:2193–2198
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma S, Gidding S, Jamerson KA, Jones DW, MacLaughlin E, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr (2018) 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. J Am Coll Cardiol 71:e127–e248
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I, Authors/Task Force Members (2018) 2018 ESC/ESH Guidelines for the management of arterial hypertension. J Hypertens 36:1953–2041
Parati G, Stergiou G, O’Brien E et al (2014) European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens 32:1359–1366
Canpolat N, Kasapcopur O, Caliskan S, Gokalp S, Bor M, Tasdemir M, Sever L, Arisoy N (2013) Ambulatory blood pressure and subclinical cardiovascular disease in patients with juvenile-onset systemic lupus erythematosus. Pediatr Nephrol 28:305–313
Campbell JF, Swartz SJ, Wenderfer SE (2015) Nocturnal hypertension and attenuated nocturnal blood pressure dipping is common in pediatric lupus. F1000Research 4:164
Sabio JM, Martinez-Bordonado J, Sánchez-Berná I, Vargas-Hitos JA, Mediavilla JD, Navarrete-Navarrete N, Zamora-Pasadas M, Ruíz ME, Jiménez-Alonso J (2015) Nighttime blood pressure patterns and subclinical atherosclerosis in women with systemic lupus erythematosus. J Rheumatol 42:2310–2317
Tan EM, Cohen AS, Fries JF, Masi AT, Mcshane DJ, Rothfield NF, Schaller JG, Talal N, Winchester RJ (1982) The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25:1271–1277
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725
Campos-Nonato I, Hernández-Barrera L, Pedroza-Tobías A, Medina C, Barquera S (2018) Hipertensión arterial en adultos mexicanos: prevalencia, diagnóstico y tipo de tratamiento. Ensanut MC 2016. Salud Publica Mex 60:233–243
Pickering TG (2005) Should we be evaluating blood pressure dipping status in clinical practice? J Clin Hypertens (Greenwich) 7:178–182
Marcovecchio ML, Dalton RN, Schwarze CP, Prevost AT, Neil HA, Acerini CL, Barrett T, Cooper JD, Edge J, Shield J, Widmer B, Todd JA, Dunger DB (2009) Ambulatory blood pressure measurements are related to albumin excretion and are predictive for risk of microalbuminuria in young people with type 1 diabetes. Diabetologia 52:1173–1181
Barenbrock M, Spieker C, Hausberg M, Rahn KH, Zidek W, Kisters K (1999) Studies on diurnal blood pressure variation in kidney diseases associated with excessive salt and water retention. J Hum Hypertens 13:269–273
Redon J, Plancha E, Swift PA, Pons S, Muñoz J, Martinez F (2010) Nocturnal blood pressure and progression to end-stage renal disease or death in nondiabetic chronic kidney disease stages 3 and 4. J Hypertens 28:602–607
Boggia J, Li Y, Thijs L, Hansen TW, Kikuya M, Björklund-Bodegård K, Richart T, Ohkubo T, Kuznetsova T, Torp-Pedersen C, Lind L, Ibsen H, Imai Y, Wang J, Sandoya E, O'Brien E, Staessen JA, International Database on Ambulatory blood pressure monitoring in relation to Cardiovascular Outcomes (IDACO) investigators (2007) Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet 370:1219–1229
Andoh D, Kobayashi M, Yasuda G, Hirawa N, Saka S, Yatsu K, Yamamoto Y, Umemura S (2009) Loss of nocturnal decline of blood pressure in non-diabetic patients with nephrotic syndrome in the early and middle stages of chronic kidney disease. Hypertens Res 32:364–368
Sarkar S, Sinha A, Lakshmy R, Agarwala A, Saxena A, Hari P, Bagga A (2017) Ambulatory blood pressure monitoring in frequently relapsing nephrotic syndrome. Indian J Pediatr 84:31–35
Kono K, Fujii H, Nakai K, Goto S, Watanabe S, Watanabe K, Nishi S (2016) Relationship between type of hypertension and renal arteriolosclerosis in chronic glomerular disease. Kidney Blood Press Res 41:374–383
Mathis KW, Venegas-Pont M, Masterson CW, Wasson KL, Ryan MJ (2011) Blood pressure in a hypertensive mouse model of SLE is not salt-sensitive. Am J Phys Regul Integr Comp Phys 301:R1281–R1285
Imai Y, Abe K, Sasaki S, Minami N, Munakata M, Nihei M, Sekino H, Yoshinaga K (1989) Exogenous glucocorticoid eliminates or reverses circadian blood pressure variations. J Hypertens 7:113–120
Maxwell SR, Moots RJ, Kendall MJ (1994) Corticosteroids: do they damage the cardiovascular system? Postgrad Med J 70:863–870
Franco M, Tapia E, Bautista R, Pacheco U, Santamaria J, Quiroz Y, Johnson RJ, Rodriguez-Iturbe B (2013) Impaired pressure natriuresis resulting in salt-sensitive hypertension is caused by tubulointerstitial immune cell infiltration in the kidney. Am J Phys Renal Phys 304:F982–F990
Rodríguez-Iturbe B, Quiroz Y, Nava M, Bonet L, Chávez M, Herrera-Acosta J, Johnson RJ, Pons HA (2002) Reduction of renal immune cell infiltration results in blood pressure control in genetically hypertensive rats. Am J Physiol Physiol 282:F191–F201
Jaffé D, Sutherland LE, Barker DM, Dahl LK (1970) Effects of chronic excess salt ingestion. Morphologic findings in kidneys of rats with differing genetic susceptibilities to hypertension. Arch Pathol 90:1–16
Mattson DL (2014) Infiltrating immune cells in the kidney in salt-sensitive hypertension and renal injury. Am J Phys Renal Phys 307:F499–F508
Rudofsky UH, Dilwith RL, Roths JB, Lawrence DA, Kelley VE, Magro AM (1984) Differences in the occurrence of hypertension among (NZB X NZW)F1, MRL-lpr, and BXSB mice with lupus nephritis. Am J Pathol 116:107–114
Franco M, Martínez F, Quiroz Y, Galicia O, Bautista R, Johnson RJ, Rodríguez-Iturbe B (2007) Renal angiotensin II concentration and interstitial infiltration of immune cells are correlated with blood pressure levels in salt-sensitive hypertension. Am J Physiol Integr Comp Physiol 293:R251–R256
De Miguel C, Lund H, Mattson DL (2011) High dietary protein exacerbates hypertension and renal damage in Dahl SS rats by increasing infiltrating immune cells in the kidney. Hypertension 57:269–274
Sommers SC, Relman AS, Smithwick RH (1958) Histologic studies of kidney biopsy specimens from patients with hypertension. Am J Pathol 34:685–715
Nakano M, Ueno M, Hasegawa H, Watanabe T, Kuroda T, Ito S, Arakawa M (1998) Renal haemodynamic characteristics in patients with lupus nephritis. Ann Rheum Dis 57:226–230
Malvar A, Pirruccio P, Alberton V, Lococo B, Recalde C, Fazini B, Nagaraja H, Indrakanti D, Rovin BH (2017) Histologic versus clinical remission in proliferative lupus nephritis. Nephrol Dial Transplant 32:1338–1344
Thomas G, Drawz PE (2018) BP measurement techniques. Clin J Am Soc Nephrol 13:1124–1131
Acknowledgments
We wish to thank Dr. Jaime Galindo-Uribe, Dr. Julia B. Ramírez-González, Dr. Reyna L. Pacheco-Domínguez, and Dr. Ricardo A. Osorio from Centro de Investigación en Políticas, Población y Salud, UNAM, for their collaboration with patient recruitment.
Funding
This work was supported by the Mexican Council of Science and Technology (CONACYT, Fondo Sectorial de Investigación en Salud y Seguridad Social—S0008-2016-01-272914 to Luis E. Morales-Buenrostro).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 34 kb)
Rights and permissions
About this article
Cite this article
Mejia-Vilet, J.M., López-Hernández, Y.J., Trujeque-Matos, M. et al. High frequency of nocturnal hypertension in lupus nephritis: should ABPM be implemented in usual practice?. Clin Rheumatol 39, 1147–1155 (2020). https://doi.org/10.1007/s10067-019-04830-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-019-04830-9