Abstract
Introduction
The rheumatoid factor (RF) is present in numerous autoimmune disorders, although its role in many of them remains a subject of research. The study assesses the role of RF as an immunological and prognostic factor in the primary Sjögren’s syndrome (pSS).
Methods
Seventy-five pSS patients (mean age 50.03 ± 15.1), 65 (87%) females, and 10 (13%) males. WBC, CRP, RF, ESR, gammaglobulins, C4, C3 component of complement, cryoglobulins, ANA, anti-SS-A, and anti-SS-B antibodies were determined. The disease activity assessed with ESSDAI. Minor salivary gland biopsy (focus score and immunochemistry) was conducted. Results were analyzed with U Mann-Whitney (continuous variables) tests, correlations between quantitative variables assessed with the Spearman correlation coefficient with statistical significance set at p < 0.05. The approval of the Bioethics Committee was obtained.
Results
Two subgroups I-RF(+) (61%) and II-RF(−) (39%) were established, with lower WBC (p = 0.012) and higher ESR (p = 0.016), gammaglobulin concentration (p = 0.007) in group I. Conjunctivitis sicca was more severe in group I. There was positive correlation between RF and lnANA (rho = 0.496), anti-SS-A, anti-SS-B antibodies (rho = 0.448; rho = 0.397 respectively). There was higher disease activity ESSDAI in group I than in group II (Me, 3.0 vs 2.0; p < 0.003). RF correlated negatively with WBC (rho = − 0.374). RF did not correlate with serum concentrations of BAFF, APRIL, CRP, and C3, C4 and with CD19+, CD3+, CD4+, CD 21+, and CD35+.
Conclusions
RF should be considered as a prognostic, but not diagnostic, factor in patients with pSS, as it is associated with more severe disease course (sicca eye symptoms, ESSDAI) and parameters (production of gammaglobulins, ANA, anti SS-A, anti-SS-B autoantibodies) indicating increased B cell activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The rheumatoid factor (RF) was first discovered in 1922 by Kurt Myer, who described an antibody against the Fc portion of human immunoglobulin G. In 1940, Eric Waaler, a Norwegian doctor, first described the test, in which antibody directed against serum gammaglobulins promoted agglutination of sheep erythrocytes sensitized by subagglutinating doses of rabbit antibodies. The name “rheumatoid factor” came to use when Harry Malvin Rose found that RF was present in sera of patients with rheumatoid arthritis [1]. For more than 70 years, RF is known as a marker of numerous autoimmune diseases—yet, it may emerge in healthy subjects as well. The RF constitutes a class of IgM or IgA, rarely IgG antibodies which are directed against Fc portion of immunoglobulin G; as previously said it is “an antibody against antibody.” At the base of RF production lays the stimulation of the immune system by some triggering factors, such as bacterial liposaccharides and viruses’ antigens, as well as autoantigens and immune complexes. The RF is one of the cytokines playing vital role in the acquired immune response to microbial organisms taking part in such mechanisms as agglutination, phagocytosis, and clearance of immune-complexes [1, 2]. Therefore, basically, the production of RF may be considered a physiological phenomenon. As it was pointed out, the RF, with low affinity to the Fc fragment of IgG, is observed in healthy subject and, transiently, during some infections. Yet, the high affinity RF, produced by CD 5+ B cells, emerges as a result of a chronic stimulation of the immune system and therefore may increase autoimmune response in autoimmune diseases, e.g. RA or pSS. What is important, the high affinity RF acts as cryoglobulin and enhances the coagulation. It is well known that chronic virus infections, for which B-lymphocytes are target cells, such as hepatitis C infection, or Epstein-Barr virus, lead to RF production [3]. It was demonstrated that the chronic HCV infection, with IL 10 and IL 4, IL-12 serum levels elevated, leads to the protection of B cells CD 5+ from apoptosis, causing an increase of RF production [3]. The Table 1 shows the most common diseases in which RF is present and in the highest concentrations in the patients sera. The RF production may be induced both trough the T cell dependent as T cell-independent pathway. RF positive B cells may act as antigen-presenting cells and some authors suggests that RF-positive B cells are more efficient as APCs than others [4,5,6].
In the general population, the frequency of RF is estimated at 4.3% in Caucasians [7, 8]. Interestingly, Newkirk et al. in 1998 found, in some tribes North American Indians, RF-IgM positivity in 31% of diabetes patient and in 7% of healthy subject [9]. In western countries, RF seropositivity is linked to such factors as age and smoking. Primary Sjögren’s syndrome (pSS) is a chronic systemic autoimmune disease, in which stimulation of B cells with their hyperreactivity and autoantibodies production dominates. The underlying pathophysiological mechanisms in the pSS is the damage to the epithelial cells, the cells apoptosis and the release of antigens and RNA complexes. From the moment the epithelial cells are damaged, interferon gamma (IFN-γ) is secreted by cells such as macrophages or dendritic cells and the cells are stimulated to secrete a B cell-activating factor (BAFF), stimulating the maturation and differentiation of B cells and other cytokines that stimulate lymphocytes B such as proliferation-inducing ligand (APRIL) which has similar effect to BAFF [10, 11]. The continuous stimulation of B lymphocytes leads to the breaking of autotolerance and to autoantibodies production—particularly against ribonucleoproteins SS-A and SS-B. Despite the production of antibodies against ribonucleoproteins, pSS is one of the autoimmune diseases in which RF is present in sera of the majority of patients. It is estimated that about 60% of patients with pSS test is positive for RF [1]. Diaz–Lopez and colleagues [12] found that male patients with pSS presented higher concentrations of RF-IgA than female ones. In pSS, majority of patients have polyclonal RF, but in over 5% of them, B cells—due to their prolonged hyperactivity—switch to the monoclonal RF production and development of lymphoproliferative diseases [4, 12]. The aim of the presented study was to assess the role of RF as an immunological and prognostic factor in the primary Sjögren’s syndrome patients.
Material and methods
The study included 75 pSS patients (mean age 50.03 ± 15.1), 65 (87%) females and 10 (13%) males.
Laboratory tests were performed, including white blood count (WBC), erythrocyte sedimentation rate (ESR), serum levels of C-reactive protein (CRP), rheumatoid factor (using nephelometry method), C4, and C3 component of complement. Serum cytokines levels as B cell-activating factor (BAFF) and a proliferation-inducing ligand (APRIL) were evaluated using standard ELISA assays. Gammaglobulin fractions were analyzed with the serum protein electrophoresis. Antinuclear antibodies (ANA) were determined by indirect immunofluorescence (IF) on the cell line HEp-2 (Human Epithelial purpose; HEp-2000) and anti-SS-A and anti-SS-B antibodies were determined by the semi-quantitative method immunoblot (Anti-ENA Profile Plus, Euroimmun, Germany, DL 1590-1601-1 G). All patients were tested for the presence of hepatitis virus C (HCV) antibodies; patients with suspected infection were excluded from the analysis. The disease activity was assessed with EULAR Sjogren’s syndrome disease activity index (ESSDAI). Minor salivary gland biopsies (focus score and immunochemistry with the assessment of the presence of CD3+, CD 4+, CD 19+, CD 21+, and CD 35+ cells) were conducted. Eye examinations and evaluations of symptoms of eye dryness, as well as the effects of reductions in the aqueous phase of tears, were carried out in the course of diagnostics of pSS with a Schirmer test and Ocular Staining Score (OSS)—using lissamine green and fluorescein staining, with the quantitative assessment of changes. The normality of continuous variables distribution was verified using the Shapiro-Wilk test. Results were analyzed with U Mann-Whitney (continuous variables) test, correlations between quantitative variables assessed with the Spearman correlation coefficient with statistical significance set at p < 0.05. The statistical analysis was carried out with Statistica13. The approval of the Bioethics Committee of National Institute of Geriatrics, Rheumatology and Rehabilitation was obtained.
Results
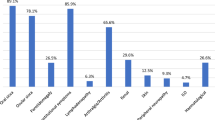
Patients were divided into two groups: group I—RF positive (+) (61%) and group II—RF negative (−) (39%). No differences were found between groups in terms of age and sex ratio. In group I, RF ranged from 20 to 1295 IU/ml (mean value 159.1 IU/ml). The lower WBC (p = 0.012), higher ESR (p = 0.016), and higher gammaglobulin concentration (p = 0.007) were also observed in group I. Conjunctivitis sicca (KS) evaluation by Schirmer’s test and Ocular Staining Score (OSS) was more severe in group I (Table 1).
There was positive correlation between RF and lnANA (rho = 0.496), anti-SS-A, anti-SS-B antibodies (rho = 0.448; rho = 0.397, respectively) which is presented on Figs. 1, 2, and 3.
There is a higher disease activity measured using ESSDAI in group I (p < 0.003; Fig. 4).
Rheumatoid factor did not correlate with the serum concentration of BAFF, APRIL, CRP, C3, and C4 or with the presence of CD19 +, CD3 +, CD4 +, CD 21+, and CD35+ cells in infiltrates in the biopsy of minor salivary glands.
The results are presented in Table 2.
Figure 5 presents the significant difference between the groups in the number of white blood cells, with the predominance of leukopenia in the group RF positive.
Discussion
The presence of RF in many rheumatic diseases creates problems in determining its significance. For many years, RF remained the main biomarker for the diagnosis of RA, but nowadays, the discovery of antibodies to cyclic citrullinated proteins (ACPA) has changed the diagnostic process in this disease. Although the rheumatoid factor is presently perceived as a prognostic marker for autoimmune rheumatic diseases, its presence can also be linked to many other serious and chronic diseases. As mentioned above, RF is common in patients with pSS. However, autoantibodies against ribonucleoproteins—anti SS-A/Ro and anti SS-B antibodies—with particular reference to anti SS-A antibodies, remain the main biomarkers of pSS. These autoantibodies, along with RF, may also be found in other than pSS autoimmune diseases. To make the matters more complicated, some of pSS patients are anti-SS-a anti SS-B negative. For this “seronegative” patients, in previously employed pSS classification criteria, the simultaneous presence of RF and ANA was a confirmation of immunological activity in pSS [13]. Obtained results confirm the previous studies about prevalence of RF in pSS patients group [1, 2]. The results also indicate correlations of RF presence with the pSS activity assessed by the ESSDAI questionnaire and the severity of dry eye symptoms (Schirmer’s test, OSS). Attention should be paid to the negative correlation of RF and leukopenia (rho = − 374), which may indicate an autoimmune character of leukopenia [14].
Similar observations, concerning the positive correlation of the RF presence with symptoms of dryness, hypergammaglobulinemia, presence of ANA antibodies in the higher titer, presence of anti-SS-A antibodies, anti-SS-B, accelerated SR, and leukopenia were presented by Witte et al. [15], who analyzed a group of 352 patients with systemic lupus erythematosus. The presence of RF in both patients with pSS and in other autoimmune diseases, as well as in infections, indicates the formation of a large number of other antibodies and the formation of antigen complexes with antibodies in these conditions. Increased activity of B lymphocytes and production of autoantibodies may also be associated with the autoimmune leukopenia, as was suggested by other researchers [14]. In the studied group of patients, the number of white blood cells negatively correlated with RF. The occurrence of leukopenia may therefore be interpreted as related to the higher activity of B cells (resulting in high levels of RF, gamma globulins, anti-SS-A antibodies). There was no RF correlation with BAFF and APRIL, which can confirm the fact, that although the RF is closely linked to the activity of B cells, its presence does not depend on the concentration of serum B cell-stimulating factors.
Nocturne et al. [16] studied a group of pSS patients with lymphoma. This group consisted mostly of individuals with mucosa-associated lymphoid tissue (MALT) lymphoma, but included patients with non-Hodgkin’s lymphoma (NHL) and diffuse large B cell lymphoma (DLBCL) as well. In the analyzed group, the RF presence proved to be a predictive factor for the lymphoma development. In their observations, authors showed that for each additional 10 IU of RF concentration, the risk of lymphoma development was increased by 5.7% (OR 1.057 [95% CI 1.026–1.100]). What seems to be particularly important, the researchers showed significant differences in the concentration of RF between the studied group (with pSS and lymphoma) and the control group, consisting of pSS patients without lymphoma (mean SD ± 568.4 ± 1.729 IU versus 31.26 ± 99.5 IU; p < 0.0001) [16].
In the research presented in our article, the study group included only two subjects with a diagnosed lymphoma. Small number of such individuals made a broader analysis of the association of RF with lymphoma impossible. Still, in the light of the cited observations by Nocturne et al., special attention should be paid to patients with RF, with regard to the increased risk of lymphoma development.
Similarly, Watanabe et al. presented RF as a prognostic factor of increase disease activity in antineutrophil cytoplasmic antibody associated vasculitis [17].
The significance of certain immunological markers, including rheumatoid factor, was presented by Spanish researchers. Their research was based on the evaluation of up to 1580 patients from the multicenter registry of Spanish pSS patients (GEAS-SS SEMI Registry). The authors showed that patients with severe systemic disease with organ involvement more frequently developed anemia and lymphopenia and presented low C3 and C4 component levels. Cryoglobulins and, what is important for the current analysis, rheumatoid factor were present in the sera of these patients [18].
Intriguing results were presented by Birnbaum et al. who, in the group pf pSS patients, sought confirmation of the presence of small fiber neuropathy (SFN) [19]. Their research has shown that, of the investigated group, 23 pSS patients had confirmed SFN, including 13 with pure form and with 10 mixed one, while 98 pSS patients had no SFN. Interestingly, patients with SFN were less likely to have RF and other autoantibodies, including anti SS-A and SS-B antibodies. In this group, there were also more males in comparison with the group without SFN. In SFN group, some patients (n = 10) had a mixed form of SFN. The patients of this subgroup were older and this subgroup was characterized by the older age of patients and higher percentage of subjects with anti-SS-autoantibodies presence—compared to the pure SFN subgroup. In both subgroups, the symptoms of SFN could precede the development of dryness—in the subgroup with pure SFN, this took place in 38.5% of cases and in the group with mixed SFN in 50% of patients. This phenomenon requires explanation and further research.
The presence in pSS of hyperreactivity of B cells and of the increase in the expression of their growth factors has drawn the attention of researchers and clinicians to the possibilities of the treatment of pSS through the inhibition of these phenomena. Until now, among the drugs aimed at depleting B lymphocytes, the highest efficacy in the treatment of pSS has been demonstrated for rituximab—anti-CD20 monoclonal antibody [20, 21].
There are certain studies confirming the RF usefulness in predicting the response to the immunosuppressive treatment on B-depleting therapy [22, 23]. On the other hand, Jones et al. presented the conflicting conclusion that the RF may inhibit the effector function of rituximab [24].
Conclusions
All presented and discussed results confirm the importance of RF presence assessment for clinical purposes, particularly for the disease activity evaluation, and suggest considering the RF as an independent risk factor of lymphoma development. In the light of the conducted research, the rheumatoid factor should be considered as a prognostic, but not a diagnostic, factor in patients with pSS.
The rheumatoid factor presence is associated with a more severe disease course (sicca eye symptoms, ESSDAI, lower WBC) and the production of gammaglobulins, ANA, anti SS-A, and anti-SS-B autoantibodies—indicating increased B cell activity.
References
Ingegnoli F, Castelli R, Gualtierotti R (2013) Rheumatoid factor: clinicla applications. Dis Markers 35(6):727–734
Haberman AM, William J, Euler C, Shlomchik MJ (2003) Rheumatoid factors in health and disease: structure, function, induction and regulation. Curr Dir Autoimmun 6:169–195
Orge E, Cefle A, Yazici A, Gürel-Polat N, Hulagu S (2010) The positivity of rheumatoid factor and anti-cyclic citrullinated peptide antibody in nonarthritic patients with chronic hepatitis C infection. Rheumatol Int 30(4):485–488. https://doi.org/10.1007/s00296-009-0997-1
Newkirk MM (2002) Rheumatoid factors: host resistance or autoimmunity? Clin Immunol 104:1–13
Cornec D, Saraux A, Pers JO, Jousse-Joulin S, Marhadour T, Roguedas-Contios AM, Genestet S, Renaudineau Y, Devauchelle-Pensec V (2014) Diagnostic accuracy of blood B-cell subset profiling and autoimmunity markers in primary Sjogren’s syndrome. Arthritis Res Ther 16:R15
Mizuochi T, Ito M, Takai K, Yamaguchi K (2009) Differential susceptibility of peripheral blood CD5+ and CD5- B cells to apoptosis in chronic hepatitis C patients. Biochem Biophys Res Commun 389(3):512–515. https://doi.org/10.1016/j.bbrc.2009.09.012
Nielsen SF, Bojeson SE, Schnohr P, Nordestaarg BG (2012) Elevated rheumatoid factor and long term risk of rheumatoid arthritis: a prospective cohort study. BMJ 345:e5244
Simard JF (2012) Rheumatoid factor positivity in the general population. Is unlikely to be discovered incidentally. BMJ 345:e5841
Newkirk MM, Lepage K, Niwa T, Rubin L (1998) Advanced glycation endproducts (AGE) on IgG, a target for circulating antibodies in North American Indians with Rheumatoid Arthritis (RA). Cell Molec Biol 44:1129–1138
Mavragani CP, Crow MK (2010) Activation of the type I interferon pathway in primary Sjögren’s syndrome. J Autoimmun 35:225–231
Youinou P, Pers JO (2011) Disturbance of cytokine networks in Sjögren’s syndrome. Arthritis Res Ther 13:227
Diaz-Lopez C, Geli C, Corominasetal H (2004) Are there clinical or serological differences between male and female patients with primary Sjögren’s syndrome? J Rheumatol 31(7):1352–1355
Shiboski SC, Shiboski CH, Criswell L et al (2012) American College of Rheumatology classification criteria for Sjögren’s syndrome: a data-driven, expert consensus approach in the Sjögren’s International Collaborative Clinical Alliance cohort. Arthritis Care Res (Hoboken) 64:475–487
Ramos-Casals M, Font J, Garcia-Carrasco M, , et al. Primary Sjogren syndrome: hematologic patterns of disease expression. (2002) Medicine (Baltimore) 81: 281–292
Witte T, Hartung K, Sachse C et al (2000) Rheumatoid factors in systemic lupus erythematosus: association with clinical and laboratory parameters. SLE study group. Rheumatol Int 19:107–111
Nocturne G, Virone A, Ng W-F, le Guern V, Hachulla E, Cornec D, Daien C, Vittecoq O, Bienvenu B, Marcelli C, Wendling D, Amoura Z, Dhote R, Lavigne C, Fior R, Gottenberg JE, Seror R, Mariette X (2016) Rheumatoid factor and disease activity are independent predictors of lymphoma in primary Sjögren’s syndrome. Arthritis Rheumatol 68:977–985
Watanabe S, Gono T, Nishina K, Sugitani N, Watanabe E, Yabe H, Terai C (2017) Rheumatoid factor is correlated with disease activity and inflammatory markers in antineutrophil cytoplasmic antibody- associated vasculitis. BMC Immunol 18:53
Flores-Chávez A, Kostov B, Solans R et al (2018) Severe, life-threatening phenotype of primary Sjögren’s syndrome: clinical characterisation and outcomes in 1580 patients (GEAS-SS Registry). Clin Exp Rheumatol 36 Suppl 112(3):121–129
Birnbaum J, Lalji A, Saed A, Baer AN (2018) Biopsy-proven small-fiber neuropathy in primary Sjögren’s syndrome: neuropathic pain characteristics, autoantibody findings, and histopathological features. Arthritis Care Res (Hoboken). https://doi.org/10.1002/acr.23762
Gottenberg JE, Cinquetti G, Larroche C et al (2013) Efficacy of rituximab in systemic manifestations of primary Sjogren’s syndrome: results in 78 patients of the Autoimmune and Rituximab registry. Ann Rheum Dis 72:1026–1031
Sada PR, Isenberg D, Ciurtin C (2015) Biologic treatment in Sjögren’s syndrome. Rheumatology (Oxford) 54:219–230
Maneiro RJ, Salgado E, Carmona L, Gomez-Reino JJ (2013) Rheumatoid factor as predictor of response to abatacept, rituximab and tocilizumab in rheumatoid arthritis: systematic review and meta-analysis. Semin Arthritis Rheum 43(1):9–17
Isaacs JD, Cohen SB, Emery P, Tak PP, Wang J, Lei G, Williams S, Lal P, Read SJ (2013) Effect of baseline rheumatoid factor and anticitrullinated peptide antibody serotype on rituximab clinical response: a meta-analysis. Ann Rheum Dis 72(3):329–336
Jones JD, Shyu I, Newkirk MM, Rigby WF (2013) A rheumatoid factor paradox: inhibition of rituximab effector function. Arthritis Res Ther 15(1):R20
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures were performed according to Helsinki Declaration. The approval of the Bioethics Committee of National Institute of Geriatrics, Rheumatology, and Rehabilitation was obtained.
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Maślińska, M., Mańczak, M. & Kwiatkowska, B. Usefulness of rheumatoid factor as an immunological and prognostic marker in PSS patients. Clin Rheumatol 38, 1301–1307 (2019). https://doi.org/10.1007/s10067-019-04438-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-019-04438-z