Abstract
Introduction/objectives
Patients with rheumatoid arthritis (RA) are at increased risk for congestive heart failure (CHF) and left ventricular diastolic dysfunction (LVDD), as compared to the general population. High disease activity is to be associated with higher incidence of cardiovascular disease (CVD), CHF, and mortality in RA patients. LVDD is not anticipated in RA patients without CVD symptoms and may be underdiagnosed especially in those with low disease activity.
Method
The study group consisted of 70 RA patients (54 women, 16 men) with no CVD and 33 healthy controls, of comparable age. All RA patients had low disease activity (DAS28 ≤ 3.2) from 2 to 7 years. Laboratory and imaging assessments included metabolic, RA-related, and cardiovascular parameters. Echocardiographic and Doppler studies were conducted in patients and controls with assessment of ejection fraction (EF) and diastolic dysfunction (assessed as E/A ratio).
Results
The mean E/A ratio did not differ significantly between RA patients and healthy controls (1.08 (0.28) vs 0.99 (0.21), NS); comparable numbers of patients and controls had abnormal E/A (< 1.0) (26 (37.1%) vs 10 (30.3%), NS). Patients with decreased E/A were significantly older and had higher disease duration, activity, and presence of bone erosions than their RA counterparts with normal E/A. The mean EF was not significantly different in patients and controls.
Conclusions
The prevalence of DD as expressed by E/A ratio in RA patients with continued low disease activity was not different from that of controls. Higher disease duration and severity may predispose to DD occurrence in patients with preserved EF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a chronic, autoimmune disease, characterized by progressive, symmetric arthritis of peripheral, synovial joints, leading to irreversible joint destruction. Patients with RA have an increased risk of cardiovascular disease (CVD) including 2-fold increased risk of congestive heart failure (CHF) as compared to the general population [1, 2]. In patients with RA, CHF is less likely to be preceded by CVD, and in those with CHF, the ejection fraction (EF) is more likely to be preserved (EF ≥ 50%) [2, 3].
The higher prevalence of left ventricular (LV) diastolic dysfunction (LVDD) has been reported in RA patients compared with non-RA subjects [1,2,3,4,5,6] or no significant difference was observed between RA patients and controls [7]. Almost equal number of studies provides evidence for and against the role of disease activity and duration as predictors of LVDD [1]. Furthermore, almost all studies investigated patients with high or differentiated disease activity.
In the general population, LVDD is an independent predictor of mortality and incident CHF [1]. However, routine screening for LVDD is rarely performed in RA patients, especially in those without clinical symptoms [2].
The purpose of this study was to assess LVDD in patients with continued low activity RA and without a history of CHF, and to compare with non-RA healthy controls.
Materials and methods
The study was performed on outpatients with RA, treated in the Regional Outpatient Clinic in Rzeszów, Poland, as described previously [8]. All patients fulfilled the American College of Rheumatology (ACR)/European League Against Rheumatism (EULAR) classification criteria for RA [9]. The protocol of the study has been approved by the Ethics Committee of the Medical University of Lublin, with the approval number KE-0254/92/2013, and the study has been performed in accordance with the 1964 Declaration of Helsinki and its later amendments. The informed consent was obtained from each patient, after an adequate explanation of the design of the research.
The study group consisted of 70 RA patients, 54 women and 16 men, of comparable age, who had continued low disease activity (4.2 (1.2) years, from 2 to 7 years) and no clinically evident CVD (e.g., ischemic heart diseases (IHD), CHF, hypertension), as well as other diseases which increase CV risk (diabetes, chronic kidney disease (CKD)). The control group consisted of 33 healthy volunteers, 18 women and 15 men, of comparable age.
Demographic and clinical information was obtained through structured interview, review of medical records, self-report questionnaires, physical examination, and laboratory tests. Assessment of the CV system was performed using the following methods: electrocardiogram (ECG), echocardiography, and high-resolution B-mode ultrasonography, as described previously [8].
RA-related data collection
Disease activity of RA was assessed using the Disease Activity Score (DAS) based on evaluation of 28 joints (DAS28) [10]. The cut point for low disease activity is DAS28 ≤ 3.2.
An erosive form of RA was diagnosed in those patients who presented erosions on joint surfaces of bones in radiograms of hands and/or feet. Radiographs of hands and feet were taken up to 6 months before study entry and assessed according to the Sharp/van der Heijde score (SHS) by a trained radiologist [11].
Laboratory tests
Blood was collected after overnight fasting. All the tests were performed in the Medical Laboratory Diagnostics of the Regional Outpatient Clinic, according to standardized laboratory methods, as described previously [8].
The standard assessment included complete blood cell count, erythrocyte sedimentation rate (ESR), serum concentration of C-reactive protein (CRP), creatinine, glucose, total cholesterol (TC), high-density lipoprotein (HDL) cholesterol (HDL-C), low-density lipoprotein (LDL) cholesterol (LDL-C), and triglycerides (TG). Renal function was estimated by assessing serum creatinine concentration and creatinine-based estimated glomerular filtration rate (eGFR) calculated using the Modification of Diet in Renal Disease (MDRD) formula [12]. The atherogenic index (AI) was calculated as ratio of TC and HDL-C concentrations with the normal value in women < 4.0 and in men < 4.5.
Blood samples were also taken to assess RA serological markers: IgM rheumatoid factor (RF-IgM) and anti-cyclic citrullinated peptide (anti-CCP) antibodies, using enzyme-linked immunosorbent assays (ELISA). RF-IgM was determined using Johnson&Johnson ELISA, with the normal upper limit 12 units (IU)/ml. Anti-CCP antibodies were determined using the EUROIMMUN ELISA, with the normal upper limit 5 units (RU)/ml. Serum samples were also stored at − 80 °C for further assessment of amino-terminal pro-brain natriuretic peptide (NT-proBNP).
CV parameters
Traditional and nontraditional CV risk factors were assessed in every patient. Information concerning CVD, diabetes, and CKD was taken from medical records.
During physical examination, blood pressure (BP) was assessed in a sitting position.
Height and weight were measured barefoot wearing light clothes. Body mass index (BMI) was calculated as the ratio of weight and squared height.
The 10-year risk of fatal CVD using the Systemic Coronary Risk Evaluation (SCORE) model was estimated in every patient. According to the EULAR recommendations, the result was multiplied by 1.5 (mSCORE) [13].
Measurement of NT-proBNP serum concentration was performed using electrochemiluminescence immunoassay (ECLIA), Cobas assay (Elecsys pro-BNP II test). The recommended normal range is up to 125 pg/ml in patients < 75 years of age and up to 450 pg/ml in older patients.
Electrocardiogram
Electrocardiogram (ECG) was performed in RA patients and controls. Resting 12-lead ECGs (25 mm/s paper speed and 10 mm/mV amplitude) were recorded using a three-channel direct writing machine (ASPEL-Mr Gold). ECGs were reviewed by an independent cardiologist. For each ECG, data on the following parameters were recorded: heart rate, QRS interval, QT interval, heart rate-corrected QT (QTc) calculated using Bazett’s formula.
Echocardiographic examination
Echocardiographic examination was performed in RA patients and controls. All the assessments were performed by an independent cardiologist, not knowing the patients’ information, using a commercially available system (Philips HD15XE). Subjects were examined in the left lateral recumbent position using standard parasternal views and apical views. Left ventricular (LV) end-systolic (LVESD) and end-diastolic (LVEDD) dimensions, LV wall thickness, and left atrial (LA) diameter were measured by two-dimensional-guided M-mode echocardiography. LV function was assessed by ejection fraction (EF). Early (E) and late (A) diastolic mitral inflow velocities were measured by standard and tissue Doppler imaging (TDI) and E/A ratio calculated. The result of E/A ratio ≥ 1.0 is defined as normal and < 1.0 is equivalent for DD.
Carotid intima-media thickness measurement
An assessment of the carotid intima-media thickness (cIMT) was performed in RA patients and controls. cIMT was measured using high-resolution B-mode ultrasound (Philips HD15XE). In every subject, IMT was assessed bilaterally in the three regions: common carotid artery (CCA), carotid bulb (BULB), and internal carotid artery (ICA). The average of the maximum IMT from all six carotid segments (defined as mean cIMT) was used in the analyses. The mean cIMT value < 0.6 mm is considered as normal, ≥ 0.9 mm as abnormal. The presence of carotid plaques is a marker of advanced atherosclerosis. Plaques were defined as a distinct protrusion, greater than 1.5 mm into the vessel lumen [14].
Statistical analysis
Results were expressed as mean (standard deviation, SD) or number (%) and range of values (minimum and maximum). Variables were tested for normality by the Kolmogorov-Smirnov test. Differences between RA patients and controls as well as between the specific groups of RA patients were tested using Kruskal-Wallis H test, Mann-Whitney U test as well as Student’s t test and chi2 test, for non-normally and normally distributed parameters, respectively. For all tests, p values < 0.05 were considered significant.
Results
Demographic and disease-related variables in RA patients
The clinical characteristic of patients with RA is presented in Table 1.
The disease activity was low (DAS28 ≤ 3.2) in all RA patients. Most patients had an erosive form of RA and over ¾ of them were seropositive (RF-IgM and/or ACPA).
At the time of examination, conventional synthetic disease-modifying anti-rheumatic drugs (csDMARDs) were used in all patients and included methotrexate (MTX) in 52 (74.3%) patients (dose 10–25 mg/week, in monotherapy or combination); leflunomide (LEF), 11 (15.7%); hydroxychloroquine (HCQ), 5 (7.2%); sulfasalazine (SS), 1 (1.4%); and cyclosporine A (CsA), 1 (1.4%). Therapy with low-dose glucocorticoid (GC) (prednisone ≤ 5 mg/day) was used in 16 patients (Table 1).
There were no patients treated with biological DMARDs (bDMARDs).
Patients with RA included in the study had no history of IHD, CHF, hypertension, diabetes, and CKD. In large majority, they were non-smokers, with normal AI and BMI values. The mean NT-proBNP concentration remained within the referenced ranges. According to the mSCORE system, the mean 10-year risk of CV death was moderate, in spite of no CVD history (Table 1). Traditional CV risk factors were found in some patients: BMI > 30 kg/m2 in 9 (12.9%), increased atherogenic index in 19 (27.1%), increased cIMT (≥ 0.6 mm) in 60 (85.7%), and according to mSCORE system, high/very high 10-year risk of CV death in 23 (32.9%).
Characteristics of the control group
The control group consisted of 33 healthy subjects: 18 women (54.5%) and 15 men (45.5%) with the mean (SD) age of 53.6 (8.3) years (range 27–75). Control subjects had no traditional CV risk factors.
Comparison of patients and controls
The mean E/A ratio did not differ significantly between RA patients with low disease activity and healthy controls (1.08 (0.28) vs 0.99 (0.21), NS). The numbers of patients and controls with abnormal E/A (< 1.0) were not statistically different (26 (37.1%) vs 10 (30.3%), NS); however, patients with RA were more likely to have abnormal E/A ratio than in non-RA subjects (OR = 1.4; 95% CI 0.6 to 3.3, NS).
The mean EF did not differ significantly in patients and controls (59.8 (1.6) vs 60.2 (0.9)%, NS). The mean age was not significantly different in patients and controls (53.9 (13.1) vs 53.6 (8.3) years, NS).
Comparison of groups of patients with normal and decreased E/A ratio
The decreased E/A ratio (< 1) was found in 26 (37.1%) patients with low RA activity and with no clinically evident CVD. The comparison of patients with normal and decreased E/A ratio is presented in Table 2. Statistically significant differences observed between the two groups of patients included metabolic parameters, CV parameters, and RA-related variables associated with the disease course.
Patients with decreased E/A were significantly older, had significantly lower eGFR, and had significantly higher TG, glucose, and BMI values. Furthermore, the mSCORE was 2.5-fold higher in these patients (Table 2). Significant differences of CV parameters included lower EF and higher values of QTc, cIMT, NT-proBNP, SBP, and DBP. Almost 90% of patients with decreased E/A had atherosclerotic plaques (Table 2).
Considering the course of RA, patients with decreased E/A were characterized by significantly higher disease duration, ESR value, disease activity (DAS28, RF-IgM titers), and presence of bone erosions (Table 2).
The mean E/A was significantly lower in patients with atherosclerotic plaques vs with no plaques (0.99 (0.22) vs 1.24 (0.3), p < 0.001) as well as in patients with bone destructions (erosions) in comparison with no erosion (1.02 (0.29) vs 1.6 (0.25), p = 0.03).
The presence of atherosclerotic plaques and abnormal BMI (≥ 25 kg/m2) was significantly associated with abnormal E/A value (respectively OR = 9.2; 95% CI 2.3 to 36.1, p = 0.001; OR = 6.0; 95% CI 2.0 to 17.7, p < 0.001).
The presence of bone erosions was associated with 3.9-fold increased occurrence of abnormal E/A ratio (OR = 3.9; 95% CI 1.3 to 11.5, p = 0.01). The disease activity was also significantly associated with DD and the higher DAS28 and the higher risk: 3-fold increase in patients with DAS28 ≥ 2.8 (OR = 3.0; 95% CI 1.6 to 5.6, p = 0.0004) and 3.3-fold increase in patients with DAS28 ≥ 3.0 (OR = 3.3; 95% CI 1.8 to 6.1, p < 0.0001).
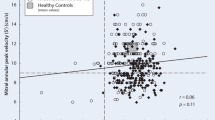
Correlations between E/A ratio and metabolic CV parameters
Negative correlations were found between E/A ratio and the following parameters: patients’ age and disease duration, values of CV and metabolic parameters (cIMT, SBP, DBP, BMI, TC, LDL-C, TG, AI, mSCORE), and RA parameters (DAS28, ESR, RF-IgM). In the multiple linear regression analysis, significant negative associations were confirmed for E/A ratio with age (b = − 0.008, p = 0.04) and TG concentration (b = − 0.002, p = 0.04).
Discussion
Our study showed that the mean E/A ratio was not significantly different between RA patients with low disease activity and healthy controls. However, decreased E/A was found in over 1/3 of patients with RA and there were no clinically evident CVD and preserved EF. It is noteworthy that the feature of diastolic heart dysfunction suggesting increased CV risk was found in the group of RA patients, in spite of continued low disease activity (DAS28 ≤ 3.2) and no history of CVD.
The decreased E/A ratio was associated with an erosive form of RA, higher disease duration and activity, and higher values of ESR and RF-IgM. It seems that patients with higher inflammatory and/or immunological parameters have greater risk of DD, even in the group with low RA activity. Patients with decreased E/A ratio were also significantly older and had unfavorable CV and metabolic parameters in comparison with their RA counterparts with normal E/A. The significant correlation was found between DD expressed as E/A ratio with patients’ age and TG level.
It seems that as RA progresses, the prevalence of DD increases as measured by E/A ratio. A decreased E/A ratio may be the first sign of impaired diastolic function that occurs even in RA patients with continued low disease activity.
Similar results were reported in the study done by Muizz et al.; however, they included patients with various disease activities (from low to high) [7]. The prevalence of DD in the RA group was not different from that in controls (47.2% vs 50.9%). They also found higher ESR level in patients with DD compared with the normal diastolic function group [7]. Arslan et al. reported that in patients with active RA, E/A ratio was significantly lower than that in controls [15]. In another study, RA patients with new onset of CHF had a higher ESR level at diagnosis up to 6 months after diagnosis [16]. In contrary, other studies showed significantly higher prevalence of DD in RA patients than in controls (23–43% vs 6–26%); however, RA activity was heterogeneous and mostly high [1, 3,4,5,6, 17], or the disease activity was not assessed [3].
According to the literature, there are studies providing evidence for and against the role of disease duration and activity as predictors of DD [1]. The duration of RA disease was strongly associated with DD in some studies [3, 4, 15, 17]. This may reflect a chronic subclinical myocardial process leading to impairment of myocardial function [3]. However, some other studies did not suggest such a link [1].
The beneficial effect of low disease activity has been suggested in RA and low disease activity to be sufficient to achieve a protective effect against CVD in RA patients [18]. The RA activity was reported to have implications on DD occurrence. The value of DAS28 ≥ 2.6 was an independent risk factor of DD, as well as systemic inflammation (ESR > 16 mm/h, CRP > 10 mg/l) [4]. The significant association of DD with IL-6 level was noted, which suggests the impact of immune dysregulation on myocardial abnormalities in RA [3].
In another study, Sharma et al. concluded that severity of the disease was strongly associated with LVDD which was supported by significantly higher DAS28 in patients with DD and an association of DD with severity of radiological damage (Steinbrocker stage) and with functional class of RA [17]. It was also found that E/A ratio had a significant correlation with age and anti-citrullinated peptide antibodies (ACPA) [17]. In another study, the correlation was observed between anti-CCP antibodies and prolongation of isovolumetric relaxation time (IVRT) as one of the parameters of LVDD [5].
Patients with RA are greatly exposed to the development of cardiac abnormalities and CV events. This condition could be attributable to several mechanisms, including high disease activity associated with high serum levels of pro-inflammatory cytokines, high titers of antibodies (RF-IgM, ACPA) [5], and presence of extra-articular symptoms and bone erosions [8]. It has been suggested that patients with RA develop some maladaptive changes in the cardiac phenotype, which are closely associated with poor outcomes. These changes progress for a long time as an asymptomatic mode, but can be detected by echocardiography [15]. It has been presented that a significant reversal of subclinical CV dysfunction accompanied by a reduction in myocardial inflammation might occur following anti-TNF therapy [19]. It has also been reported that cessation of anti-TNF therapy in patients with well-controlled established RA resulted in reduced vasodilator function but only in those patients who developed disease flare detected with the increased DAS28 value [20].
Patients with RA should be analyzed in primary prevention due to high risk of CV death, despite no clinically evident symptoms of CVD. The prevalence of DD with preserved EF has been previously associated with a marked increase in mortality in the general population [3]. The isolated DD may affect an excess mortality in RA patients. It seems that tight control of RA activity is crucial to eliminate systemic effects of inflammation. However, even in those RA patients, who have no history of CVD, well-controlled course of RA as a result of effective treatment, and continued low disease activity, careful monitoring is obligatory due to increased CV risk in comparison with non-RA subjects.
Our study has some potential limitations. First is the relatively small number of patients included into the study; higher number of patients could enable better statistical evaluation. Second, only one parameter of diastolic dysfunction was examined in the study; however, we wanted to present the parameter which is quite easy to perform in everyday clinical practice. Third, additional parameters of disease activity could enable more accurate estimation.
Our study has also several strengths. First, to our best knowledge, it is the first study performed in the group of RA patients with low disease activity. Second, this is a homogeneous study population with continued low disease activity and simultaneously no history of CVD or other diseases which increase CV risk. Third, all the patients were observed for a long time in everyday clinical practice. They came from community population and were not selected from hospitals or academic centers. Fourth, we used a homogenous therapy because all the patients were treated only with conventional synthetic DMARDs and among them MTX was used in ¾ of the patients. There were no patients treated with biological DMARDs. Fifth, all assessments performed are available on an outpatient basis.
Conclusion
The mean E/A ratio was comparable in RA patients with low disease activity and healthy controls. The decreased E/A ratio in RA patients was associated with higher age and disease duration, more severe course of RA (bone erosions), and with unfavorable CV and metabolic parameters. Decreased E/A ratio may be the first sign of impaired diastolic function that occurs even in RA patients with continued low disease activity. Asymptomatic DD may be diagnosed in RA patients by echocardiography and may be helpful in reducing CV mortality by introducing appropriate treatment at an early stage.
References
Aslam F, Bandeali SJ, Khan NA, Alam M (2013) Diastolic dysfunction in rheumatoid arthritis: a meta-analysis and systematic review. Arthritis Care Res (Hoboken) 65:534–543
Crowson CS, Myasoedova E, Davis JM 3rd, Roger VL, Karon BL, Borgeson D, Rodeheffer RJ, Therneau TM, Gabriel SE (2011) Use of B-type natriuretic peptide as a screening tool for left ventricular diastolic dysfunction in rheumatoid arthritis patients without clinical cardiovascular disease. Arthritis Care Res (Hoboken) 63:729–734
Liang KP, Myasoedova E, Crowson CS, Davis JM, Roger VL, Karon BL, Borgeson DD, Therneau TM, Rodeheffer RJ, Gabriel SE (2010) Increased prevalence of diastolic dysfunction in rheumatoid arthritis. Ann Rheum Dis 69:1665–1670
Schau T, Gottwald M, Arbach O, Seifert M, Schöpp M, Neuß M, Butter C, Zänker M (2015) Increased prevalence of diastolic heart failure in patients with rheumatoid arthritis correlates with active disease, but not with treatment type. J Rheumatol 42:2029–2037
Marasovic-Krstulovic D, Martinovic-Kaliterna D, Fabijanic D, Morovic-Vergles J (2011) Are the anti-cyclic citrullinated peptide antibodies independent predictors of myocardial involvement in patients with active rheumatoid arthritis? Rheumatology (Oxford) 50:1505–1512
Wislowska M, Jaszczyk B, Kochmanski M, Sypula S, Sztechman M (2008) Diastolic heart function in RA patients. Rheumatol Int 28:513–519
Abdul Muizz AM, Mohd Shahrir MS, Sazliyana S, Oteh M, Shamsul AS, Hussein H (2011) A cross-sectional study of diastolic dysfunction in rheumatoid arthritis and its association with disease activity. Int J Rheum Dis 14:18–30
Biskup M, Biskup W, Majdan M, Targońska-Stępniak B (2018) Cardiovascular changes in rheumatoid arthritis patients with low disease activity. Rheumatol Int 38:1207–1215
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO III, Birnbaum NS, Burmester GR, Bykerk VP, Cohen MD, Combe B, Costenbader KH, Dougados M, Emery P, Ferraccioli G, Hazes JMW, Hobbs K, Huizinga TWJ, Kavanaugh A, Kay J, Kvien TK, Laing T, Mease P, Ménard HA, Moreland LW, Naden RL, Pincus T, Smolen JS, Stanislawska-Biernat E, Symmons D, Tak PP, Upchurch KS, Vencovský J, Wolfe F, Hawker G (2010) 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 62:2569–2581
Prevoo ML, van ‘t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL (1995) Modified disease activity scores that include twenty-eight-joint counts: development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 38:44–48
van der Heijde D (2000) How to read radiographs according to the Sharp/van der Heijde method. J Rheumatol 27:261–263
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130:461–470
Peters MJL, Symmons DPM, McCarey D, Dijkmans BAC, Nicola P, Kvien TK, McInnes IB, Haentzschel H, Gonzalez-Gay MA, Provan S, Semb A, Sidiropoulos P, Kitas G, Smulders YM, Soubrier M, Szekanecz Z, Sattar N, Nurmohamed MT (2010) EULAR evidence-based recommendations for cardiovascular risk management in patients with rheumatoid arthritis and other forms of inflammatory arthritis. Ann Rheum Dis 69:325–331
Veller MG, Fisher CM, Nicolaides AN, Renton S, Geroulakos G, Stafford NJ, Sarker A, Szendro G, Belcaro G (1993) Measurement of the ultrasonic intima-media complex thickness in normal subjects. J Vasc Surg 17:719–725
Arslan S, Bozkurt E, Sari RA, Erol MK (2006) Diastolic function abnormalities in active rheumatoid arthritis evaluation by conventional Doppler and tissue Doppler: relation with duration of disease. Clin Rheumatol 25:294–299
Maradit-Kremers H, Nicola PJ, Crowson CS, Ballman KV, Jacobsen SJ, Roger VL, Gabriel SE (2007) Raised erythrocyte sedimentation rate signals heart failure in patients with rheumatoid arthritis. Ann Rheum Dis 66:76–80
Sharma A, Kaushik R, Kaushik RM, Kakkar R (2015) Echocardiographic evaluation of diastolic dysfunction in rheumatoid arthritis - a case-control study. Mod Rheumatol 25:552–557
Arts EE, Fransen J, Den Broeder AA, PLCM v R, Popa CD (2017) Low disease activity (DAS28≤3.2) reduces the risk of first cardiovascular event in rheumatoid arthritis: a time-dependent Cox regression analysis in a large cohort study. Ann Rheum Dis 76:1693–1699
Ntusi NAB, Francis JM, Sever E, Liu A, Piechnik SK, Ferreira VM, Matthews PM, Robson MD, Wordsworth PB, Neubauer S, Karamitsos TD (2018) Anti-TNF modulation reduces myocardial inflammation and improves cardiovascular function in systemic rheumatic diseases. Int J Cardiol 270:253–259
Rongen GA, van Ingen I, Kok M, Vonkeman H, Janssen M, Jansen TL (2018) Vasodilator function worsens after cessation of tumour necrosis factor inhibitor therapy in patients with rheumatoid arthritis only if a flare occurs. Clin Rheumatol 37:909–916
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study has been approved by the appropriate ethics committee and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All persons included into the study gave their informed consent prior to their inclusion in the study.
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Targońska-Stępniak, B., Biskup, M., Biskup, W. et al. Diastolic dysfunction in rheumatoid arthritis patients with low disease activity. Clin Rheumatol 38, 1131–1137 (2019). https://doi.org/10.1007/s10067-018-4369-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-018-4369-7