Abstract
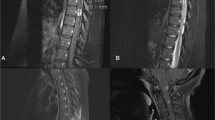
Neurosarcoidosis is uncommon with an incidence of approximately 5 to 15%. Central nervous system involvement can be divided into brain and spinal cord neurosarcoidosis. Spinal cord sarcoidosis is extremely rare, occurring in less than 1% of all sarcoidosis cases. Its manifestations may include cauda equina syndrome, radiculopathy, syringomyelia, cord atrophy, arachnoiditis, and myelopathy or transverse myelitis. We highlight two cases of spinal cord sarcoidosis, each presenting with longitudinally extensive transverse myelitis, that demonstrate the dilemmas that physicians face with regard to diagnosis and treatment. Given its rarity and the diversity of possible manifestations, establishing the diagnosis of spinal cord sarcoidosis is often very difficult. Extensive evaluation must be conducted to rule out primary neurologic, primary rheumatologic, infectious, and neoplastic diseases. MRI often demonstrates hyperintensity on T2-weighted images and enhancement following gadolinium administration. CSF analysis most consistently shows a lymphocytic pleocytosis and elevated proteins. While these less invasive investigations may be helpful, the gold standard for diagnosis is biopsy of neurologic or non-neurologic tissue confirming the presence of non-caseating granulomas. Evidence-based guidelines for the treatment of transverse myelitis secondary to sarcoidosis are lacking due to its rarity; therefore, therapy is based on expert and anecdotal experience and usually consists of high doses of steroids in combination with various immunosuppressive agents. The use of infliximab in particular appears promising, but there is a need for further investigation into the ideal treatment regimen.


Similar content being viewed by others
References
Tana C, Wegener S, Borys E, Pambuccian S, Tchernev G, Tana M, Giamberardino MA, Silingardi M (2015) Challenges in the diagnosis and treatment of neurosarcoidosis. Ann Med 47(7):576–591
Cação G, Branco A, Meireles M, Alves JE, Mateus A, Silva AM, Santos E (2017) Neurosarcoidosis according to Zajicek and scolding criteria: 15 probable and definite cases, their treatment and outcomes. J Neurol Sci 379:84–88
Wang L, Li Y (2015) Longitudinal ultra-extensive transverse myelitis as a manifestation of neurosarcoidosis. J Neurol Sci 355(1–2):64–67
Durel CA, Marignier R, Maucort-Boulch D, Iwaz J, Berthoux E, Ruivard M, André M, le Guenno G, Pérard L, Dufour JF, Turcu A, Antoine JC, Camdessanche JP, Delboy T, Sève P (2016) Clinical features and prognostic factors of spinal cord sarcoidosis: a multicenter observational study of 20 biopsy-proven patients. J Neurol 263(5):981–990
Ungprasert P, Matteson EL (2017) Neurosarcoidosis. Rheum Dis Clin N Am 43(4):593–606
Cohen-Aubart F, Galanaud D, Grabli D, Haroche J, Amoura Z, Chapelon-Abric C, Lyon-Caen O, Valeyre D, Piette JC (2010) Spinal cord sarcoidosis: clinical and laboratory profile and outcome of 31 patients in a case-control study. Medicine (Baltimore) 89(2):133–140
Fried ED, Landau AJ, Sher JH, Rao C (1993) Spinal cord sarcoidosis: a case report and review of the literature. J Assoc Acad Minor Phys 4(4):132–137
Zajicek JP, Scolding NJ, Foster O, Rovaris M, Evanson J, Moseley IF, Scadding JW, Thompson EJ, Chamoun V, Miller DH, McDonald W, Mitchell D (1999) Central nervous system sarcoidosis—diagnosis and management. QJM 92(2):103–117
Cerar T, Strle F, Stupica D, Ruzic-Sabljic E, McHugh G, Steere AC, Strle K (2016) Differences in genotype, clinical features, and inflammatory potential of Borrelia burgdorferi sensu stricto strains from Europe and the United States. Emerg Infect Dis 22(5):818–827
Halperin JJ (2018) Diagnosis and management of Lyme neuroborreliosis. Expert Rev Anti-Infect Ther 16(1):5–11
Halperin JJ (2011) Neurologic manifestations of Lyme disease. Curr Infect Dis Rep 13(4):360–366
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical standards
The manuscript does not contain clinical studies or patient data.
Disclosures
None.
Rights and permissions
About this article
Cite this article
Scott, A.M., Yinh, J., McAlindon, T. et al. Two cases of sarcoidosis presenting as longitudinally extensive transverse myelitis. Clin Rheumatol 37, 2899–2905 (2018). https://doi.org/10.1007/s10067-018-4144-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-018-4144-9