Abstract
External ventricular drain (EVD) insertion using the freehand technique is often associated with misplacements resulting in unfavorable outcomes. Augmented Reality (AR) has been increasingly used to complement conventional neuronavigation. The accuracy of AR guided EVD insertion has been investigated in several studies, on anthropomorphic phantoms, cadavers, and patients. This review aimed to assess the current knowledge and discuss potential benefits and challenges associated with AR guidance in EVD insertion. MEDLINE, EMBASE, and Web of Science were searched from inception to August 2023 for studies evaluating the accuracy of AR guidance for EVD insertion. Studies were screened for eligibility and accuracy data was extracted. The risk of bias was assessed using the Cochrane Risk of Bias Tool and the quality of evidence was assessed using the Newcastle-Ottawa-Scale. Accuracy was reported either as the average deviation from target or according to the Kakarla grading system. Of the 497 studies retrieved, 14 were included for analysis. All included studies were prospectively designed. Insertions were performed on anthropomorphic phantoms, cadavers, or patients, using several different AR devices and interfaces. Deviation from target ranged between 0.7 and 11.9 mm. Accuracy according to the Kakarla grading scale ranged between 82 and 96%. Accuracy was higher for AR compared to the freehand technique in all studies that had control groups. Current evidence demonstrates that AR is more accurate than free-hand technique for EVD insertion. However, studies are few, the technology developing, and there is a need for further studies on patients in relevant clinical settings.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
1 Introduction
The insertion of an external ventricular drain (EVD) is a widely performed neurosurgical procedure for measuring and treating increased intracerebral pressure (Dey et al. 2012). The current standard is freehand insertion based on anatomical landmarks. The drain is usually inserted through Kocher’s point (1–2 cm anterior to the coronal suture and 1–2 cm lateral to the cranial anteroposterior midline) and aimed at an imaginary intersection formed by transverse and sagittal planes passing through the external auditory meatus and the medial cantus, respectively (Huyette et al. 2008). Successful placement is then verified by the loss of resistance as the ventricular wall is punctured and the subsequent flow of cerebrospinal fluid through the EVD (Huyette et al. 2008). The procedure is performed blindly without visualizing subsurface structures and catheter misplacements are common (Clifton et al. 2019; Cho et al. 2020). Misplacement is reported in 10–40% of cases and is associated with irreversible tissue damage, hematomas, and unfavorable outcomes (Sarrafzadeh et al. 2014; Kakarla et al. 2008).
Several technological solutions are available to assist the surgeon in EVD placement (Aljoghaiman et al. 2022; Stuart et al. 2021). Intraoperative computed tomography (CT), 3D ultrasound, endoscopic navigation, fluoroscopic guidance and stereotactic neuro-navigation have all been shown to increase insertion accuracy (Aljoghaiman et al. 2022; Stuart et al. 2021). However, the different solutions all carry their own sets of limitations, which may make them useful in some settings and not in others. Ideally, a universal guidance solution for EVD-placement should be low cost, self-sufficient, easily portable between operating rooms (ORs) or intensive care units (ICUs), quick to set up, easy to use and provide accurate three-dimensional guidance with an intuitive interface. EVD placements are commonly performed in emergency settings and more complex and bulky systems such as neuro-navigation, intraoperative CT or Cone Beam CT may not be easily available. The presentation of 3D structures in 2D on separate screens is associated with attention shift that may lead to fatigue, prolonged operating time, and a potential increase in errors due to task switching (Cho et al. 2020; AlAzri et al. 2017).
Augmented Reality (AR) is an emerging method for neuro-navigation where computer-generated 3D images are overlayed onto real-world objects, significantly reducing attention shifts during procedures (Cho et al. 2020; Besharati Tabrizi and Mahvash 2015; Iop et al. 2022). AR has been shown to improve accuracy in the surgical treatment of intracranial pathologies such as aneurysms, gliomas, meningiomas, and acoustic neuromas (Cabrilo et al. 2014; Louis et al. 2021). However, research on the utilization of AR for EVD insertion is limited (Aljoghaiman et al. 2022) and largely experimental (Li et al. 2018; Skyrman et al. 2021; Chiou et al. 2022; 2023; Schneider et al. 2021; 2023; Kunz et al. 2021; Lai et al. 2022). This study aimed to review the current knowledge on the use of AR guidance for the insertion of EVDs, to evaluate and discuss potential benefits and challenges. A special focus was placed on reported accuracies.
2 Methods and material
Before conducting the analysis, a comprehensive protocol outlining the objectives and strategies for data collection and analysis was developed. This protocol adhered to the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) guidelines (Page et al. 2021).
2.1 Search strategy and selection process
Literature on AR guided EVD insertions published until August 2023 was reviewed using MEDLINE, EMBASE and Web of Science. Potential studies were identified using the following key-terms (including MeSH terms, relevant abbreviations, synonyms, variations due to plurality and spelling): “ventriculostomy”, “external ventricular drain”, “accuracy”, “guidance” and “augmented reality”. The detailed search strategy is provided in the supplementary file (Online Resource 1). Following the primary search, duplicates were removed. Studies were then further selected based on title, abstract and full text. Studies where AR was used to visualize the insertion of an EVD using the freehand technique were included for analysis. The reference lists of the studies included were screened for possible relevant publications. Other systematic reviews, virtual simulation studies, and studies where accuracy was not reported were excluded.
2.2 Data extraction
Variables of interest included study characteristics (country, design, and year of publication), location where the procedure was performed (bedside, simulated operation room, or operation room), surgeon experience level, type of AR interface, type of subject (patients, cadaver, or anthropomorphic phantom), follow-up method, and outcome measures. The primary outcome was the accuracy of inserting an EVD using AR.
2.3 Assessment of bias and certainty of evidence
The Newcastle-Ottawa quality Assessment Scale (NOS) checklist (Gierisch et al. 2014) for cohort studies was used to assess the quality of reporting in the analyzed studies. Studies were rated as good quality if they had 3 or 4 stars in the selection domain, 1 or 2 stars in the comparability domain and 3 or 4 stars in the outcome domain. Studies were of fair quality if they scored 2 stars in the selection domain, 1 or 2 stars in the comparability domain, and 2 or 3 stars in the outcome domain. Studies were classified as poor if they scored 0 or 1 star in the selection domain, no stars in the comparability domain and 0 or 1 star in the outcome domain. Bias was assessed using the bias domains of the Cochrane Risk of Bias Tool for Randomized Controlled Trials (Higgins et al. 2011). The tool has the following domains: random sequence bias, allocation concealment, blinding of participants, blinding of outcome assessment, incomplete outcome data, selective reporting, and other sources of bias. The Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach was employed to rate the body of evidence supporting the review’s key findings (Schünemann et al. 2008). A GRADE summary of findings table assembled using the GRADEpro Guideline Development Tool is provided (“GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University 2020 (Developed by Evidence Prime, Inc.). Available from Gradepro.Org.,” n.d.).
2.4 Statistical analysis
Continuous variables were summarized using means, while categorical variables were presented as counts and percentages. The accuracy of freehand insertion using AR guidance was reported either as means or percentages, extracted directly from the studies or calculated based on reported outcomes. To visualize the average accuracy of each study forest plots were used, indicating the range where 95% of the observed accuracies lie (two standard deviations from the mean). The Kruskal-Wallis test was used to analyze the variance of accuracy for the different devices. A p value lower than 0.05 was deemed significant. All statistical analyses were performed using the statistical software R (R Foundation for Statistical Computing, Vienna, Austria).
3 Results
The search through the included databases provided 497 studies, of which 199 were duplicates. After removing duplicates, 298 studies remained and were screened based on titles and abstracts, yielding 40 studies for full text analysis. Of the 40 studies, 14 studies were identified to analyze the use of AR for EVD insertion (Fig. 1). The most common reason for exclusion upon full-text analysis was that non-AR navigational systems had been investigated. Moreover, one specific study was excluded as it employed AR solely as a method for a senior neurosurgeon to supervise a junior colleague.
3.1 Study characteristics
All 14 included studies were prospectively designed and published between 2019 and 2023. These studies were conducted in the United States of America (29%), Germany (21%), Taiwan (14%), China (7%), Sweden (7%), Italy (7%), the Netherlands (7%), and Belgium (7%) (Table 2).
Most studies (79%) performed insertions on anthropomorphic phantoms. One study performed subsequent experiments using cadaveric subjects. Two studies also corroborated their findings on patients. Experiments on anthropomorphic phantoms were done in an OR setting. Two studies (14%) were performed on patients, and in one of these studies (7%), the insertions were performed in a bedside setting. One study (7%) performed insertions solely on cadaveric subjects. The number of insertions for each study ranged from 10 to 150.
In most experiments, insertions were conducted by experienced neurosurgeons (79%). Two studies included only medical students (14%). One study included students and employees at the study center. The employees’ clinical experience was not reported. One study featured a heterogeneous group of participants, including medical students, engineers in augmented reality (AR), neurosurgeons, surgical residents, and interventional radiologists.
The AR-solutions all contained three core components. First, creating the virtual 3D-model of the cranium and subsurface structures using preoperative imaging (CT or MRI). Second, the registration of the 3D-reconstruction on real anatomy in real-time, using markers to match virtual and real spaces. Both registration and navigation were frameless. Third, a visualization device was used to combine virtual and real environments. Once the registration was performed, the ventricles were visible through the visualization device. Devices were either head mounted displays (HMD) or external monitors (Table 3).
Regarding the AR interface, all experiments used frameless navigation. The primary device used for subsurface structure visualization was the Microsoft HoloLens HMD (79%). Other devices included external monitors (Samsung Galaxy Tab S5e (7%), Microsoft Surface Pro 7 tablet (7%), GCX screen (7%)) and a hybrid operating room-based augmented reality surgical navigational system (ARSN) (7%).
The assessment of accuracy was based on postoperative CT (93%), or CBCT (7%) scans. The definition of accuracy varied among studies: 11 studies (79%) quantified accuracy as the distance, in millimeters, by which the catheter tip deviated from the preoperatively planned target. Two studies assessed accuracy according to the Kakarla grading system (Table 1) (Kakarla et al. 2008). One study reported accuracy based on both the deviation from the planned path and the Kakarla grading system. Four studies also (28%) performed freehand insertions without AR guidance, as a reference for accuracy assessment (Tables 2 and 3).
3.2 Risk of bias and certainty of evidence
Based on the Cochrane Risk of Bias tool, 11 studies (79%) were categorized as “poor,” and three studies (21%) as "good" (Online Resource 2). The predominant sources of bias were the absence of randomization and a lack of allocation concealment, both leading to selection bias. Following the assessment of the studies’ quality according to NOS, most studies were classified as fair (67%), two studies were classified as good (16%) and two as poor (16%) (Online Resource 3). Using the GRADE approach, the existing body of evidence exhibited a low level of certainty regarding both the accuracy of AR-guided EVD insertions and the superiority of AR over the freehand approach (Online Resource 4).
3.3 Accuracy of EVD insertion using AR
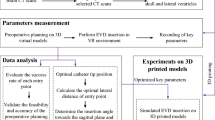
The 11 Studies reporting the deviation from the planned path revealed an average accuracy ranging between 0.7 to 11.9 mm (Fig. 2). Insertions performed by neurosurgeons consistently exhibited higher accuracy with deviations below 5.2 mm. There were no significant differences (p = 0.755) in accuracy for the different interfaces: Microsoft HoloLens (HMD), ARSN (External monitor), and tablet screens. The type of subject experimented on did not yield significant variations in accuracy. The study by Li et al. (2018) including neurosurgeons and a control group, investigating bedside placement of EVD on patients, demonstrated a significant improvement in accuracy. The average deviation from target decreased from 11.3 to 4.3 mm.
Reported average accuracy from each study with respective 95% interval. Studies that did not report accuracy in means were excluded in this plot. Dotted line marks 5 mm. Grey circles: average accuracy of AR-guided EVD insertion. Black squares: accuracy achieved by control groups performing freehand insertions
The studies by Van Gestel et al. (2021) and Eom et al. (2022), involved medical students using Microsoft HoloLens. Both studies had control groups using the freehand technique. Compared to these control groups, the use of Microsoft HoloLens improved accuracy. The deviations decreased from 19.9 to 11.9 mm, and from 13.5 to 7.4 mm, in the respective study.
The study by Benmahdjoub et al. (2023) that included students and employees achieved high accuracy for both AR devices (Xiaomi tablet and Microsoft HoloLens), both exhibiting an average deviation of 2 mm. The study by Bounajem et al. (2023) which included medical students, clinicians, and engineers using Microsoft HoloLens, reported a low average deviation of 1.9 mm.
Studies that used the Kakarla grading system showed AR accuracies, between 82 and 96% (Fig. 3). Among these studies, two conducted comparative analyses between AR-assisted and the freehand technique. In these control groups, the accuracy of EVD insertion was 72% and 73%, respectively. Notably, the study conducted by Schneider et al. (2023) initially indicated that the freehand technique (73%) yielded higher accuracy than AR (68%). However, after undergoing three sessions of training with AR navigation, accuracy significantly improved to 95%. In all three studies, EVD insertions were carried out by neurosurgeons using Microsoft HoloLens. The study conducted by Kunz et al. (2021) was performed on patients, and the other two on anthropomorphic phantoms.
Percentage of accurately placed drains according to the Kakarla grading system. The rate of accurate AR insertion is presented in black. The accuracy reported by control groups using the freehand technique is presented in grey. The study by Umana et al. (2021) lacks a control group
4 Discussion
The conventional freehand technique, relying on anatomical landmarks, remains the main method for EVD insertion (Huyette et al. 2008). However, due to the lack of subsurface guidance, misplacement rates are high, even in experienced hands (Frisk et al. 2022; Munzer et al. 2019). This review summarizes the current evidence for the use of AR for EVD insertion (Li et al. 2018; Skyrman et al. 2021; Chiou et al. 2022; 2023; Schneider et al. 2021; 2023; Kunz et al. 2021; Benmahdjoub et al. 2023; Bounajem et al. 2023; Gibby et al. 2021), in an effort to provide insights into the benefits and challenges of implementing AR navigation for EVD placement.
4.1 Benefits
Current literature indicates that AR may serve as an accurate guidance system for EVD insertion. When performed by neurosurgeons, AR guided EVD insertions exhibited 5 mm deviation from the planned target (Li et al. 2018; Skyrman et al. 2021; Chiou et al. 2022; 2023; Schneider et al. 2021; 2023; Kunz et al. 2021; Benmahdjoub et al. 2023; Bounajem et al. 2023; Gibby et al. 2021). In that context, the typical width of a normal ventricle is within the range of 9.6 to 18.3 mm (Toma et al. 2009). With a 5 mm deviation, the catheter tip would still be correctly placed in the ipsilateral ventricle in most cases. The inbound error of most conventional navigation systems is in the range of 2–3 mm (Frisk et al. 2022). AR studies using the Kakarla grading system (Kakarla et al. 2008) also showed that 82–96% of the catheters were correctly placed in the ventricle (Kakarla grade I). Compared to the freehand technique, AR navigation excels in accuracy.
In clinical practice, EVD insertions are often performed by junior residents (Guha et al. 2017), and it is of interest to note that insertions performed by non-specialists were more accurate than freehand. In this review, four of the studies included non-specialists. While Eom et al. (2022) and Van Gestel et al. (2021) reported deviations exceeding 7 mm, Benmahdjoub et al. (2023) and Bounajem et al. (2023) found deviations lower than 2 mm. Additionally, Van Gestel et al. (2021) and Bounajem et al. (2023) discovered that non-specialists positively influenced the learning curve, resulting in superior performance among untrained individuals compared to trained ones.
EVD insertions are often urgent procedures, and the use of conventional navigational technologies may conflict with the need for speed (AlAzri et al. 2017). In this context, AR presents a fast and user-friendly alternative requiring less bulky hardware at a competitive cost (Chiou et al. 2023; Khoshnevisan and Allahabadi 2012; Mikhail et al. 2019). Importantly, AR-navigation systems based on HMD-technology are sufficiently mobile to be used outside of the OR, such as in emergency bedside procedures (Karmonik et al. 2018).
4.2 Challenges
The benefits of adding AR-navigation to the relatively simple procedure of EVD-insertion are arguably greatest in novice hands (Li et al. 2018; Skyrman et al. 2021; Schneider et al. 2021; Kunz et al. 2021; Van Gestel et al. 2021; Eom et al. 2022). However, proficiency requires familiarity and training with the systems. Neither the novice nor the expert can expect to perform AR-navigated procedures with ease, if the systems are used only in extreme cases when their benefit is obvious. Apprehensions of the neurosurgeons, that a relatively straightforward procedure becomes overly complex need to be addressed if the technology is to become adopted (Skyrman et al. 2021).
The adoption of AR for EVD insertion introduces some technological challenges. One is the choice of interface. Optic see-through devices can impair depth perception due to accommodation-divergence, where the eye must continuously refocus between the nearby glass display and the distant real object. In contrast, semi-transparent HMDs and external displays reduce perceptual discrepancies by offering control of both virtual and real environments. Schneider et al. and Kunz et al. (2021) discussed that most HMDs are designed for domestic use and may not perform as well in an OR. External monitors provide navigation without the need for eye tracking, but their placement in the OR may be challenging. Additionally, insufficient data processing and transfer speeds may introduce delays in remapping the virtual environment to the real world and cause disturbing visual lag (Dixon et al. 2014).
Another challenge associated with all types of navigation is brain shift (Munzer et al. 2019; Yeh and Wickens 2001). This may be remedied by using intraoperative imaging to update the AR view (Mikhail et al. 2019). However, none of the included studies have addressed this issue.
The use of AR guidance may lead to “inattentional blindness”, where the surgeon becomes distracted by information added to the visual field. Solid overlays may be replaced by wire-mesh and inverse-realism overlay techniques to reduce inattentional blindness (Lai et al. 2022; Dixon et al. 2014; Yeh and Wickens 2001; Marcus et al. 2015). None of the studies reviewed provided a cost–benefit analysis. If the cost is too high, it could hinder adoption of the technology in smaller centers or in low- and middle-income settings, where it may provide the greatest benefit (Meola et al. 2017).
4.3 Limitations of current studies
The majority of the studies were conducted on anthropomorphic phantoms. While these phantoms are designed to be realistic, they do not fully replicate a clinical situation (Chiou et al. 2022). Unfortunately, the studies on patients had small sample sizes. Not all studies incorporated control groups, which hinders the assessment of improved accuracy. Meta-analysis of accuracies could not be performed since outcome metrics were heterogenous. Most studies did not report the number of insertion attempts required for successful placement, limiting the reliability of the accuracy data. A high number of attempts is associated with an elevated risk of infection, tissue damage, and hemorrhage (Yuen et al. 2018). Most studies exhibited a high risk of selection bias and suboptimal quality according to the NOS, decreasing the overall quality of the evidence.
4.4 Future studies
Randomized controlled trials are needed to compare the efficiency of AR navigation to conventional navigation in a clinical setting. Important variables are the choice of interface, the ease of use, efficacy, accuracy, solutions to inattentional blindness and visual lag. Cost-effectiveness of AR navigation in relation to surgical volumes must be investigated. It is imperative that AR interfaces are developed to seamlessly integrate with the demands of an operating room environment and come at a competitive cost.
5 Conclusion
Current evidence demonstrates that AR is more accurate than free-hand technique for EVD insertion. However, studies are few, the technology developing and there is a need for further studies on patients in relevant clinical settings.
Data availability
The data utilized for the writing of this article can be provided by the corresponding author upon reasonable request.
References
AlAzri A, Mok K, Chankowsky J, Mullah M, Marcoux J (2017) Placement accuracy of external ventricular drain when comparing freehand insertion to neuronavigation guidance in severe traumatic brain injury. Acta Neurochir 159(8):1399–1411. https://doi.org/10.1007/s00701-017-3201-5
Aljoghaiman M, Bergen B, Takroni R, Wang B, Eangles P, Farrokhyar F, Sharma S (2022) Image-guided versus freehand ventricular drain insertion: systematic review and meta-analysis. World Neurosurgery 160:85-93.e5. https://doi.org/10.1016/j.wneu.2022.01.036
Benmahdjoub M, Thabit A, van Veelen M-LC, Niessen WJ, Wolvius EB, van Walsum T (2023) Evaluation of AR visualization approaches for catheter insertion into the ventricle cavity. IEEE Trans Visualization Comput Graphics. https://doi.org/10.1109/TVCG.2023.3247042
Bounajem MT, Cameron B, Sorensen K, Parr R, Gibby W, Prashant G, Evans JJ, Karsy M (2023) Improved accuracy and lowered learning curve of ventricular targeting using augmented reality-phantom and cadaveric model testing. Neurosurgery 92(4):884–891. https://doi.org/10.1227/neu.0000000000002293
Cabrilo I, Bijlenga P, Schaller K (2014) Augmented reality in the surgery of cerebral aneurysms: a technical report. Neurosurgery. https://doi.org/10.1227/NEU.0000000000000328
Chiou S-Y, Zhang Z-Y, Liu H-L, Yan J-L, Wei K-C, Chen P-Y (2022) Augmented reality surgical navigation system for external ventricular drain. Healthcare 10(10):1815. https://doi.org/10.3390/healthcare10101815
Chiou S-Y, Liu L-S, Lee C-W, Kim D-H, Al-Masni MA, Liu H-L, Wei K-C, Yan J-L, Chen P-Y (2023) augmented reality surgical navigation system integrated with deep learning. Bioengineering 10(5):617. https://doi.org/10.3390/bioengineering10050617
Cho J, Rahimpour S, Andrew Cutler C, Goodwin R, Lad SP, Codd P (2020) Enhancing reality: a systematic review of augmented reality in neuronavigation and education. World Neurosurg 139:186–195. https://doi.org/10.1016/j.wneu.2020.04.043
Clifton W, Dove C, Damon A, Freeman WD, Brown B (2019) 3-Dimensional simulation videography for instructional placement of bedside external ventricular drains. World Neurosurg 131:242. https://doi.org/10.1016/j.wneu.2019.07.049
Dey M, Jaffe J, Stadnik A, Awad IA (2012) External ventricular drainage for intraventricular hemorrhage. Curr Neurol Neurosci Rep 12(1):24–33. https://doi.org/10.1007/s11910-011-0231-x
Dixon BJ, Daly MJ, Chan HHL, Vescan A, Witterick IJ, Irish JC (2014) Inattentional blindness increased with augmented reality surgical navigation. Am J Rhinol Allergy 28(5):433–437. https://doi.org/10.2500/ajra.2014.28.4067
Eom S, Sykes D, Rahimpour S, Gorlatova M (2022) NeuroLens: augmented reality-based contextual guidance through surgical tool tracking in neurosurgery. In: 2022 IEEE International symposium on mixed and augmented reality (ISMAR), 355–64. https://doi.org/10.1109/ISMAR55827.2022.00051.
Frisk H, Lindqvist E, Persson O, Weinzierl J, Bruetzel LK, Cewe P, Burström G, Edström E, Elmi-Terander A (2022) Feasibility and accuracy of thoracolumbar pedicle screw placement using an augmented reality head mounted device. Sensors 22(2):522. https://doi.org/10.3390/s22020522
Gestel V, Frederick TF, Vannerom C, Verhellen A, Gallagher AG, Elprama SA, Jacobs An et al (2021) The effect of augmented reality on the accuracy and learning curve of external ventricular drain placement. Neurosurg Focus 51(2):E8. https://doi.org/10.3171/2021.5.FOCUS21215
Gibby W, Cvetko S, Gibby A, Gibby C, Sorensen K, Andrews EG, Maroon J, Parr R (2021) The application of augmented reality-based navigation for accurate target acquisition of deep brain sites: advances in neurosurgical guidance. J Neurosurg. https://doi.org/10.3171/2021.9.JNS21510
Gierisch Jennifer M, Beadles C, et al. (2014) NEWCASTLE-OTTAWA scale coding manual for cohort studies. In: health disparities in quality indicators of healthcare among adults with mental illness [Internet]. Department of Veterans Affairs (US). https://www.ncbi.nlm.nih.gov/books/NBK299087/.
“GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University, 2020 (Developed by Evidence Prime, Inc.). Available from Gradepro.Org.” n.d.
Guha D, Alotaibi NM, Nguyen N, Gupta S, McFaul C, Yang VX. D (2017) Augmented reality in neurosurgery: a review of current concepts and emerging applications. Canadian J Neurological Sci Le J Canadien Des Sci Neurologiques. https://doi.org/10.1017/cjn.2016.443
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savović J, Schulz KF, Weeks L, Sterne JAC (2011) The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Huyette DR, Turnbow BJ, Kaufman C, Vaslow DF, Whiting BB, Michael YOh (2008) Accuracy of the freehand pass technique for ventriculostomy catheter placement: retrospective assessment using computed tomography scans. J Neurosurg 108(1):88–91. https://doi.org/10.3171/JNS/2008/108/01/0088
Iop A, El-Hajj VG, Gharios M, de Giorgio A, Monetti FM, Edström E, Elmi-Terander A, Romero M (2022) Extended reality in neurosurgical education: a systematic review. Sensors 22(16):6067. https://doi.org/10.3390/s22166067
Kakarla UK, Chang SW, Theodore N, Spetzler RF, Kim LJ (2008) Safety and accuracy of bedside external ventricular drain placement. Op Neurosurg. https://doi.org/10.1227/01.NEU.0000312390.83127.7F
Karmonik C, Boone TB, Khavari R (2018) Workflow for visualization of neuroimaging data with an augmented reality device. J Digit Imaging 31(1):26–31. https://doi.org/10.1007/s10278-017-9991-4
Khoshnevisan A, Allahabadi NS (2012) Neuronavigation: principles, clinical applications and potential pitfalls. Iran J Psychiatry 7(2):97–103
Kunz C, Hlaváč M, Schneider M, Pala A, Henrich P, Jickeli B, Wörn H, Hein B, Wirtz R, Mathis-Ullrich F (2021) Autonomous planning and intraoperative augmented reality navigation for neurosurgery. IEEE Trans Med Robotics Bionics 3(3):738–749. https://doi.org/10.1109/TMRB.2021.3091184
Lai M, Skyrman S, Kor F, Homan R, El-Hajj VG, Babic D, Edström E, Elmi-Terander A, Hendriks BHW, de With PHN (2022) Development of a CT-compatible, anthropomorphic skull and brain phantom for neurosurgical planning, training, and simulation. Bioengineering 9(10):537. https://doi.org/10.3390/bioengineering9100537
Li Ye, Chen X, Wang N, Zhang W, Li D, Zhang L, Xin Qu et al (2018) A wearable mixed-reality holographic computer for guiding external ventricular drain insertion at the bedside. J Neurosurg. https://doi.org/10.3171/2018.4.JNS18124
Louis RG, Steinberg GK, Duma C, Britz G, Mehta V, Pace J, Selman W, Jean WC (2021) Early experience with virtual and synchronized augmented reality platform for preoperative planning and intraoperative navigation: a case series. Operative Neurosurg 21(4):189–196. https://doi.org/10.1093/ons/opab188
Marcus HJ, Pratt P, Hughes-Hallett A, Cundy TP, Marcus AP, Yang G-Z, Darzi A, Nandi D (2015) Comparative effectiveness and safety of image guidance systems in neurosurgery: a preclinical randomized study. J Neurosurg 123(2):307–313. https://doi.org/10.3171/2014.10.JNS141662
Meola A, Cutolo F, Carbone M, Cagnazzo F, Ferrari M, Ferrari V (2017) Augmented reality in neurosurgery: a systematic review. Neurosurg Rev 40(4):537–548. https://doi.org/10.1007/s10143-016-0732-9
Mikhail M, Mithani K, Ibrahim GM (2019) Presurgical and intraoperative augmented reality in neuro-oncologic surgery: clinical experiences and limitations. World Neurosurg 128:268–276. https://doi.org/10.1016/j.wneu.2019.04.256
Munzer BW, Khan MM, Shipman B, Mahajan P (2019) Augmented reality in emergency medicine: a scoping review. J Med Internet Res 21(4):e12368. https://doi.org/10.2196/12368
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Sarrafzadeh A, Smoll N, Schaller K (2014) Guided (VENTRI-GUIDE) versus freehand ventriculostomy: study protocol for a randomized controlled trial. Trials 15:478. https://doi.org/10.1186/1745-6215-15-478
Schneider M, Kunz C, Pal’a A, Wirtz CR, Mathis-Ullrich F, Hlaváč M (2021) Augmented reality-assisted ventriculostomy. Neurosurg Focus 50(1):E16. https://doi.org/10.3171/2020.10.FOCUS20779
Schneider M, Kunz C, Wirtz CR, Mathis-Ullrich F, Pala A, Hlavac M (2023) Augmented reality-assisted versus freehand ventriculostomy in a head model. J Neurological Surg, Part A Central European Neurosurg. https://doi.org/10.1055/s-0042-1759827
Schünemann HJ, Oxman AD, Brozek J, Glasziou P, Jaeschke R, Vist GE, Williams JW et al (2008) Grading quality of evidence and strength of recommendations for diagnostic tests and strategies. BMJ (clinical Research Ed) 336(7653):1106–1110. https://doi.org/10.1136/bmj.39500.677199.AE
Skyrman S, Lai M, Edström E, Burström G, Förander P, Homan R, Kor F et al (2021) Augmented reality navigation for cranial biopsy and external ventricular drain insertion. Neurosurg Focus 51(2):E7. https://doi.org/10.3171/2021.5.FOCUS20813
Stuart MJ, Antony J, Withers TK, Ng W (2021) Systematic review and meta-analysis of external ventricular drain placement accuracy and narrative review of guidance devices. J Clin Neurosci 94:140–151. https://doi.org/10.1016/j.jocn.2021.10.014
Tabrizi Mahvash B LM (2015) Augmented reality-guided neurosurgery: accuracy and intraoperative application of an image projection technique. J Neurosurg 123(1):206–211. https://doi.org/10.3171/2014.9.JNS141001
Toma AK, Camp S, Watkins LD, Grieve J, Kitchen ND (2009) External ventricular drain insertion accuracy: Is there a need for change in practice? Neurosurgery. https://doi.org/10.1227/01.NEU.0000356973.39913.0B
Yeh M, Wickens CD (2001) Display signaling in augmented reality: effects of cue reliability and image realism on attention allocation and trust calibration. Hum Factors 43(3):355–365. https://doi.org/10.1518/001872001775898269
Yuen J, Selbi W, Muquit S, Berei T (2018) Complication rates of external ventricular drain insertion by surgeons of different experience. Ann R Coll Surg Engl 100(3):221–225. https://doi.org/10.1308/rcsann.2017.0221
Umana GE, Scalia G, Yagmurlu K, Mineo R, Di Bella S, Giunta M et al (2021). Multimodal Simulation of a Novel Device for a Safe and Effective External Ventricular Drain Placement. Frontiers in neuroscience 15:690705. https://doi.org/10.3389/fnins.2021.690705
Robertson FC, Sha RM, Amich JM, Essayed W, Lal A, Lee BH et al (2021). Frameless neuronavigation with computer vision and real-time tracking for bedside external ventricular drain placement: a cadaveric study. Journal of neurosurgery, 136(5), 1475–1484. https://doi.org/10.3171/2021.5.JNS211033
Funding
Open access funding provided by Karolinska Institute. None of the authors received any funds for the writing of this manuscript. AET was supported by Region Stockholm in a clinical research appointment.
Author information
Authors and Affiliations
Contributions
Conceptualization: Ali Buwaider. Methodology: Ali Buwaider; Data curation: Ali Buwaider; Victor Gabriel El-Hajj. Formal analysis and investigation: Ali Buwaider Writing—original draft preparation: Ali Buwaider Writing—review and editing: All authors; Supervision: Adrian Elmi-Terander; Erik Edström; Walter Jean. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Buwaider, A., El-Hajj, V.G., Iop, A. et al. Augmented reality navigation in external ventricular drain insertion—a systematic review and meta-analysis. Virtual Reality 28, 141 (2024). https://doi.org/10.1007/s10055-024-01033-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10055-024-01033-9