Abstract
The debate surrounding nature versus nurture remains a central question in neuroscience, psychology, and in psychiatry, holding implications for both aging processes and the etiology of mental illness. Epigenetics can serve as a bridge between genetic predisposition and environmental influences, thus offering a potential avenue for addressing these questions. Epigenetic clocks, in particular, offer a theoretical framework for measuring biological age based on DNA methylation signatures, enabling the identification of disparities between biological and chronological age. This structured review seeks to consolidate current knowledge regarding the relationship between mental disorders and epigenetic age within the brain. Through a comprehensive literature search encompassing databases such as EBSCO, PubMed, and ClinicalTrials.gov, relevant studies were identified and analyzed. Studies that met inclusion criteria were scrutinized, focusing on those with large sample sizes, analyses of both brain tissue and blood samples, investigation of frontal cortex markers, and a specific emphasis on schizophrenia and depressive disorders. Our review revealed a paucity of significant findings, yet notable insights emerged from studies meeting specific criteria. Studies characterized by extensive sample sizes, analysis of brain tissue and blood samples, assessment of frontal cortex markers, and a focus on schizophrenia and depressive disorders yielded particularly noteworthy results. Despite the limited number of significant findings, these studies shed light on the complex interplay between epigenetic aging and mental illness. While the current body of literature on epigenetic aging in mental disorders presents limited significant findings, it underscores the importance of further research in this area. Future studies should prioritize large sample sizes, comprehensive analyses of brain tissue and blood samples, exploration of specific brain regions such as the frontal cortex, and a focus on key mental disorders. Such endeavors will contribute to a deeper understanding of the relationship between epigenetic aging and mental illness, potentially informing novel diagnostic and therapeutic approaches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
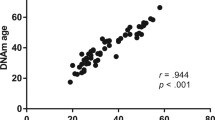
The nature-nurture debate still holds unanswered questions in the neurosciences and psychology and is relevant for understanding the etiology of mental illness. As a connector between disposition and environment, epigenetics may be capable of answering some of these questions, since the epigenome is the molecular switchboard that mediates between environmental influences and the interpretation of genetic information in the different cell types of the body [1]. However, deep neuroepigenetic insights in humans are complicated by the fact that the plasticity of the epigenome—unlike genetic variation —is variable between the different somatic cell types of an organism and over time. The need for invasive sampling procedures is therefore an almost insurmountable hurdle for human neuroepigenetics unless there is a strong clinical indication. Nevertheless, in order to gain some insights, the field has recently focused on such molecular markers through which inferences can be made about other body cell types from biomaterials obtained in a less invasive manner (e.g. leukocytes, buccal mucosa cells, urine). In particular, changes over time in the epigenome (DNA methylation [DNAm]) or chromosomes (telomere length) are documented in the literature to measure the biological age of a sample (Fig. 1). In particular, epigenetic clocks are theoretically suitable for detecting discrepancies between the measured biological age of a sample and the chronological age of a sample in order to detect indications of an accelerated or decelerated aging process that might be responsive to environmental influences.
The molecular aging process in cells affects the genome integrity and the DNAm signature. The ends of chromosomes are organized as telomeric complexes. Telomeres comprise of [TTAGGG]n tandem repeats of double-stranded DNA and protruding single-stranded 3’-overhangs. Due to the absence of telomerase activity in healthy somatic cells gradual telomere shortening with each cell cycle is an age-dependent process, which limits the maximum number of cell divisions, thus providing a protective anti-proliferative mechanism. Telomere length is correlated with biological aging. However, their length of origin at the beginning of ontogeny seems to be heterogeneous between sexes and ethnicities [59], which complicates calibration when longitudinal measurements are not available. Whereas genome-wide studies on DNAm signatures in monozygotic twins suggest a high level of persistence of early genome programming [60], subtle changes in numerous genetic loci are observed at the same time, which correlate with biological age. These form the basis for the concept of so-called epigenetic clocks [23,24,25]. Such age-related DNAm variations can take place in intergenic regions (yellow shaded) as well as in the vicinty of gene promoters (red shaded), where they can take influence on gene regulation. The frequently used ‘Horvath clock’ is, in combination with Illumina’s Infinium HumanMethylome450 BeadChips, calibrated for 353 CpG sites, which can be associated with genes, promoters, long-range regulatory elements or intergenic DNA with no known function [26, 27]. The illustration exemplarily shows an age-related hypermethylated intergenic region as well as a hypomethylated gene promoter during fetal growth that cis-activates mRNA synthesis from adjacent transcription start site (TSS). Below are shown the results of senescence, whereafter the same intergenic region became hypomethlylated and the promoter became hypermethylated. Promoter hypermethylation resulted in the suppression of mRNA synthesis from the adjacent TSS
Every human being ages. The most obvious manifestations of this process include skin changes, hair greying and/or loss of hair, changes in vision, bone density and dental appearance as well as reductions in physical performance, and cognitive capacities [2, 3]. In healthy somatic cells, the maximum number of cell divisions is limited by an aging process through molecular programming. Accompanying symptoms of cellular aging include genomic instability, telomere shortening, epigenetic changes, mitochondrial dysfunction, stem cell depletion, altered intercellular communication and immune senescence [4]. Premature aging is a condition in which biological hallmarks of the aging process do not match the changes expected with respect to the chronological age. This can be caused by various environmental influences. For example, strong sunlight exposure, especially UV light, can lead to increased DNA damage in skin cells and visible changes in the skin. Other environmental triggers can be smoking, unhealthy diet, alcohol consumption, lack of sleep and negative stress. In rarer cases, there are genetic diseases that can massively accelerate the natural aging process, such as Bloom syndrome, Werner syndrome, dyskeratosis congenita or Hutchison Gilford progeria syndrome[5, 6].
Interestingly, a variety of mental illnesses are symptomatically reminiscent of premature aging. Noticeable are motor, sensory, and cognitive impairments as well as alterations in cardiovascular and metabolic markers, and cellular biomarkers [7, 8]. People with mental illness also have an increased risk of mortality [9]. To study the correlations and cause-and-effect mechanisms between biological aging and mental illness, reliable age markers are required.
Molecular alterations dependent on age impact the epigenome’s plasticity on different molecular levels, such as DNA cytosine methylation, histone post-translational modifications as well as the 3D organization of the DNA in the nucleus and how it changes over time [10,11,12]. Epigenomes differ between the distinct somatic cell types of an organism, whereas their genomes do not. The epigenome is the sum of chemical compounds that modify or mark the genome in such a way that the information it contains can be interpreted in different cell types and at different time points, adapted to the requirements at hand [1].
The most direct level of epigenome modification is DNA cytosine methylation. This involves the covalent transfer of a methyl group to the cytosine within CpG dinucleotides through DNA methyl transferases (DNMTs) [13]. DNAm is – among other processes – involved in gene regulation, cell differentiation and development, X chromosome inactivation, and genetic imprinting [14,15,16,17,18] as well as in cognitive processes such as learning and memory formation [19]. Interestingly, environmental influences can affect DNAm signatures relevant for human behavior [20]. DNAm changes across the lifespan and forms age-typical patterns at several genomic loci [21, 22]. In the last decade, methods have been developed that exploit DNAm patterns to measure the epigenetic age of a specimen. To date, several models for ‘epigenetic clocks’ exist [23,24,25], differing in for example, the type of tissue/cells being used and the number of CpG sites examined. Frequently used is Horvarth’s epigenetic clock, which uses 353 CpG positions to determine an epigenetic age which correlates to 0.96 with chronological age. This model is reported to fit for 51 tissue types [26, 27]. Other commonly used clocks focus on peripheral tissue such as blood or saliva [28, 29]. Epigenetic clocks are outstandingly interesting since, in contrast to non-repairable DNA damage that impairs genome integrity and can induce mutations, changes in the epigenome are fundamentally reversible. Because they are at the same time apparently responsive to some environmental influences, it may be hypothesized that the aging-dependent DNAm signature could be influenced bidirectionally and thus be a biomarker for accelerated but also for decelerated aging processes.
In the field of neuroscience, there is evidence that stress and nutrition may slow down or accelerate epigenetic aging. Mental illnesses also appear to influence epigenetic age. However, so far these studies have been performed primarily on peripheral tissue and different studies come to inconsistent conclusions [25]. Although peripheral tissues, such as blood, prove to be convenient due to their easy accessibility, cortical mental illnesses and brain tissue aging samples are the most practical for studying DNAm in mental disorders [30]. A limiting factor for research is that they are usually not available for most conditions and healthy control groups in vivo. Given these limitations, we must carefully weigh up whether peripheral tissue can be used as a proxy for brain tissue. There are indications that epigenetic aging markers of peripheral blood and brain may exhibit rather small, and sometimes even no correlations, at least in older individuals [31]. Notably, when considering either physiological or psychological correlates of accelerated epigenetic aging in blood cells, results for physiological outcomes are consistent (e.g. lung function), but results for psychological outcomes are very inconsistent (e.g. mental illness) [25]. In sum, the reliability of epigenetic clock data obtained from peripheral tissues with respect to their applicability in psychology seems questionable. Therefore, in this review, we interrogate current state of knowledge about the relationship between mental disorders and epigenetic age in the brain.
Methods
The review is based on the PRISMA guidelines.
Inclusion criteria
PICO criteria
The PICO (population, intervention/exposure, comparison, outcome) criteria were used to specify the research question.
Population
No specific inclusion criteria were defined for demographic or other variables.
Intervention/exposure
individuals with mental illnesses.
Comparison
The control group included people without mental illness.
Outcome
The epigenetic age in the brain, and/or a difference between the epigenetic age in the brain between people with and without mental illnesses.
Types of studies
The studies had to be published in German or English language in international peer-reviewed scientific journals. There were no restrictions regarding the study design. Due to the young age of the research field, no restrictions were made for publication years.
Epigenetic clock
Following Oblak et al.’s definition of epigenetic clock [25], studies were included that determined epigenetic age based on methylation patterns at CpG dinucleotides.
Search strategy
Using a literature search of the EBSCO (Psychology and Behavioral Sciences Collection), Pubmed, APA PsycArticles, PubPsych (Psyndex, NARCIS, PASCAL, ERIC), and ClinicalTrials.gov databases, relevant studies were selected that had been published by February 21, 2022. A search using the keywords “epigenetic clock” OR “epigenetic age” OR “epigenetic aging” OR “age acceleration” OR “age deceleration” OR “DNAm age” OR “dna methylation” AND “brain” yielded 7,623 titles. Studies that did not involve epigenetic clocks, mental disorders, or did not directly target the human brain were excluded. Gray literature was searched, and relevant authors were contacted. Using the snowball method, references of the found original articles and relevant reviews were checked for any further studies. A total of 12 studies were identified that matched the criteria. Figure 2 illustrates the selection process using a flowchart.
Data synthesis
Information was extracted on study designs, subjects, mental disorders, methods of data collection, sampled tissues, DNA extraction, genetic and epigenetic analyses, models of the epigenetic clock, and main results of the studies. Study characteristics are summarized in Table S1.
Assessment of study quality and risk of bias
With the help of the Critical Appraisal Checklist for Analytical Cross Sectional Studies of the Joanna Briggs Institute [32], the methodological quality of the studies was assessed. Because some of the studies also examined other variables than brain epigenetic age and included additional samples, the estimation of the risk of bias refers only to the outcome criteria, and not to the entire study.
Evaluation of the quality of evidence
Evaluation of the quality of evidence was accomplished using the GRADE (Grading of Recommendations, Assessment, Development and Evaluation) manual. Study design, risk of bias, inconsistency, indirectness, imprecision of results, and possible publication bias were all considered [33]. Following the GRADE approach firstly evaluates the study design. Thereafter, the above criteria are considered, leading either to improved or worsened quality of evidence. Concerning study designs, randomized controlled studies possess a high quality of evidence. In contrast, observational studies possess a low quality of evidence. In the next step, the risk of bias is considered, and then the studies are checked for inconsistency (i.e., conflicting results). In the case of unexplainable inconsistencies, the quality of evidence is downgraded. Indirectness of results may result from differences between populations or interventions compared in a study, measures of only a proxy of the outcome of interest, or indirect comparisons between experimental and control groups. Afterwards, imprecision of studies is assessed. Imprecision may be due to small sample sizes and large confidence intervals. A further factor that may lower quality of evidence is publication bias [33]. A publication bias occurs in cases where relevant study results are not published, for example, because of non-significant results. This can lead to a misinterpretation of the evidence [34]. For each outcome (i.e., brain areas for each disease), the quality of evidence is determined separately. Four levels of quality can be achieved (high, moderate, low, and very low). These indicate the degree of confidence that effect estimates approximate real effects [35].
Results
Psychopathological entities
All studies featured a controlled cross-sectional design. Two studies examined bipolar affective disorder (BAD) [36, 37], three studies examined depression [38,39,40], one study examined posttraumatic stress disorder (PTSD) [40], one study examined obsessive compulsive disorder [41], five studies examined schizophrenia or schizoaffective disorder [42,43,44,45], and two studies examined alcohol addiction or alcohol abuse [40, 46]. Only one study included patients with different psychological disorders (i.e., PTSD, depression, and alcohol abuse) [40].
Biomaterials and aging markers
All studies included brain specimens for epigenetic age examinations, whereby seven studies used exclusively brain tissues [36, 39,40,41,42, 44, 46]. Five studies also analyzed epigenetic age in peripheral blood [37, 38, 43, 45, 47], and one study also included liver tissue [47]. In two studies additional molecular aging markers were assessed, such as telomere length and the copy number of mitochondrial DNA per cell [36, 37]. In one study, DNA cytosine methylation was not assessed using DNA methylation chip arrays but instead by methylated DNA-binding protein (MBP)-seq [38]. MBP-seq is a method that involves the pulldown of methylated DNA using MBP, followed by deep sequencing to map DNA methylation patterns across the genome. One study, moreover, considered the klotho (KL) longevity gene polymorphism rs9315202 and examined a possible association of this genetic variation with epigenetic aging [40].
Six studies used original data from their own brain studies [36, 40,41,42, 46], and one of them, respectively, also from blood [38]. Two studies exclusively used publicly available brain datasets [39, 44], while another two used brain and blood datasets [43, 45]. Two studies used own original blood data in combination with public brain datasets [37, 47] and liver datasets [47] (Table S1).
DNAm analyses and epigenetic clock models
Eleven of the studies used Horvath’s model in combination with different versions of Illumina’s Human DNA Methylation BeadChip Arrays (27K, 450K, EPIC) to determine epigenetic ages [26, 27]. Consequently, different but largely overlapping numbers of CpG sites were interrogated. Wu and co-workers further applied Hannum’s and Levine’s epigenetic clock models [28, 29] for their analyses [45]. Due to the excessive discrepancies between the epigenetic and chronological ages determined by these methods, the main results of this study relied exclusively on Horvath’s epigenetic clock. Only one study did not use BeadChip arrays [38]. Instead, this study used methyl-CpG-binding domain sequencing (MBD-seq). Therefore, the authors developed a custom epigenetic clock model, which they adapted and recalibrated using Horvath’s method. MBD-seq interrogates DNAm in a genome-wide manner. It is a precipitation method that uses MBD proteins to selectively capture CpG-methylated genome fragments, which thereafter undergo deep-sequencing. An overview of these studies, methodological characteristics, and main results can be found in Table S1 (see above, Sect. 3.3).
Outcomes
Bipolar affective disorder
BAD has been examined in two studies [36, 37]. In their first study, the examination of epigenetic age in brain tissue was used to validate blood-derived findings. [37]. This study used publicly available cerebellar data from BAD patients and control subjects. No differences were found in the entire group or in subgroups divided by age. In 2020, the same research group conducted a study on hippocampal tissue from BAD-I patients and non-psychiatric control subjects [36]. Again, no significant acceleration in aging was found between BAD and control groups in the total sample. After splitting the samples into young and older individuals, a significant difference was found among the older subjects regarding accelerated aging. Furthermore, the group showed that epigenetic accelerated aging correlated negatively with telomere length and not at all with the number of mitochondrial DNA per cell. In another study with subgroups, no difference was found considering accelerated aging in BAD patients with and without suicide as a cause of death (Table 1).
Major depression
Depression has been examined in three studies [38,39,40]. Tissue from Brodmann area 11 as well as neurons and glial cells of the prefrontal cortex [39], Brodmann area 25 [38, 39], Brodmann area 10 [38], and Brodmann areas 9, 46, 12, 32, and 4 were examined [40]. Whereas Li et al. found no difference in the acceleration of epigenetic aging [39], Han et al. describe that the epigenetic age of patients with depression was on average 1.11 years higher than that of healthy subjects [38]. Wolf et al., who examined PTSD and alcohol addiction in addition to depression did not show results for depression [40] (Table 1).
Post-traumatic stress disorder
In addition to their analyses of depression, Wolf et al. examined the association between PTSD and epigenetic age in Brodmann areas 9, 46, 12, 32, and 4 and possible correlation with a klotho (KL) gene variant [40]. Their observations suggest a correlation between a KL SNP (rs9315202), PTSD and accelerated aging in the motor cortex in the elderly: Here, carriers of the rarer allele but not of the major allele were conspicuously often diagnosed PTSD and concomitantly exhibited accelerated epigenetic aging [40] (Table 1).
Obsessive compulsive disorder
De Oliveira et al. examined the correlation between obsessive compulsive disorder and epigenetic age in the anterior cingulate cortex, orbitofrontal cortex, nuclei accumbens and caudatus, and putamen [41]. While a trend towards slowered epigenetic aging was found in the anterior cingulate cortex, the other areas showed trends for accelerated aging, but neither trend was significant (Table 1).
Schizophrenia and schizoaffective disorder
Five studies examined the correlation between accelerated epigenetic aging and schizophrenia, more specifically, schizoaffective disorder. Considering that these studies partly used Gene Expression Omnibus (GEO) datasets, specimens used in three studies show at least partial overlap [43,44,45]. The areas examined were prefrontal cortex [43,44,45,46], striatum [45, 46], superior temporal gyrus [42], hippocampus and cerebellum [45, 46]. In their study, solely Wu et al. reported significant differences between the subjects with schizophrenia and the control group regarding epigenetic aging [45]. This study included the largest number of samples, but also overlapped with the other studies. The authors examined the prefrontal cortex, cerebellum, striatum, and hippocampus, but only found a difference in the frontal cortex, in terms of slowed epigenetic age. After a subgroup analysis, this difference remained significant only in the youngest group (20–39 years). In the midrange group (40–59 years), there was a trend toward slower aging in people with schizophrenia. No difference was found in people over the age of 60. Different areas of the prefrontal cortex were not investigated separately in this study (Table 1).
Alcohol addiction and abuse
Two studies examined alcohol addiction and alcohol abuse [40, 47]. Wolf et al. showed a significant correlation between alcohol dependence and accelerated aging in men in the motor cortex [40], whereas Rosen et al. showed slower epigenetic aging in Brodmann area 9 in the alcohol addiction or abuse group compared to the control group [47]. Fourteen of the 23 subjects were diagnosed with alcohol abuse, but not with alcohol addiction (Table 1).
Discussion
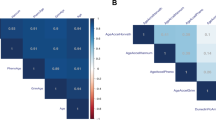
In this structured review, we systematically analyzed studies on the putative role of epigenomic aging processes in patients with mental disorders and calculated effect sizes for the results reported in each study. We found that most studies used Horvath’s model of the epigenetic clock and either brain tissue or a combination of brain tissue with peripheral blood to assess markers of epigenetic aging. Schizophrenia and schizoaffective disorder, depression and bipolar disorder are the mental disorders, which were most frequently addressed in the studies included in the structured review. Brain regions most focused on were in the frontal cortex. Significant effect sizes were calculated for five studies targeting mainly frontal brain regions but different mental disorders. In these five studies, Horvath’s, and in one case Hannum’s and Levine’s epigenetic clock models were applied, and the results are based on highly varying sample sizes. To our knowledge, we present here the first structured review on studies on the role of epigenetic aging in mental disorders. We propose that our results may help to guide successful future methodological approaches to key functions of the epigenetic clock in different mental disorders.
Brain regions
It is well known that most mental disorders are related to neurobiological aberrations in the prefrontal cortex [48,49,50,51]. Although distinct prefrontal dysfunctions are associated with each mental disorder [52], it is reasonable to assume that they all may be represented by markers of the epigenetic clock in frontal brain tissue [38, 53]. It is thus not surprising that most of the studies included in our structured review mainly addressed the frontal cortex to detect changes in the epigenetic clock in patients with mental disorders. Significant results were reported from authors who used frontal brain tissue for epigenetic analyses. In striatal, medial temporal, and cerebellar tissue, no significant associations between the epigenetic clock and mental disorders were found. Our data therefore suggest that tissue from different regions of the frontal cortex should be assessed systematically with distinct epigenetic methods to gain more specific insights into changes of the epigenetic clock related to mental disorders.
Mental disorders
Schizophrenia and depression were targeted by most studies on the epigenetic clock in mental disorders. Depression is known to depend to a considerable extent on serotonergic and dopaminergic changes in the brain [54,55,56], whereas brain pathology underlying schizophrenia is more complex and also includes morphological brain abnormalities [57]. Despite these considerable differences, brain pathology related to both mental disorders is mainly located in the frontal cortex. Only [45] reported a significant difference in the frontal cortex for epigenetic aging between patients with schizophrenia and a healthy control group. These differences strongly depended on the age of subjects. In a subgroup analysis, epigenetic slowing was significant only in the youngest group (20–39 years). In the midrange group (40–59 years), there was a trend towards slower aging in patients with schizophrenia. No difference was found in people over the age of 60. These age differences may be related to aging-related neurodevelopment, developmental aspects of schizophrenia, duration of the disease, duration of medication, or interactions of all these factors [58]. This issue needs to be addressed in future studies of aberrant epigenetic aging associated with mental disorders. Notably, that the study by Wu et al. [45] included the largest sample sizes among those reviewed in this structured review. Different areas of the prefrontal cortex were not investigated separately in this study.
Choice of methods
In the context of increasing numbers of CpG sites covered by DNA methylation BeadChip arrays, the number of statistical tests included in an ANOVA or other common statistical operations, also increases due to the increased number of variables (CpG sites). This gives rise to the well-known problem of alpha error accumulation. As the number of tests increases, the alpha error (false positive) also increases, resulting in a higher probability of finding a difference that is solely due to random variation. Consequently, the likelihood of erroneously rejecting the null hypothesis increases. The commonly used approach to correct for multiple comparisons is the Bonferroni approach. Alternative methods such as the family-wise error rate and the false discovery rate can be also employed. However, compared with the Bonferroni approach, they provide less stringent corrections and have a rather moderate impact on the study's power. Some of these corrections adjust the significance level downward based on the number of tests conducted. Instead of testing at a level of p < 0.05, for instance, a more stringent level like p < 0.0000005 may be employed when conducting a larger number of tests. This sets a very stringent threshold for significance. However, the strictness of these corrections introduces another issue. This is the reduction of study power due to controlling the alpha error. While the likelihood alpha errors is decreased by this method, the probability of making a beta error (falsely classifying a true effect as non-significant) increases. To mitigate this problem, one can increase the sample size to reduce the beta error again. It is important to note that this approach also has its limitations. When designing a study, the acceptable probabilities of errors must be carefully considered. In genomic research, one needs to be skeptical with respect to studies that utilize a large number of CpG sites, have a small sample size, and do not employ correction methods. We are here confronted with an acknowledged issue known as "p-hacking", which statisticians are well-aware of. This problem arises when authors, either intentionally or unintentionally, exploit calculated effects and argument with remarkable findings, which actually lack existence since they are solely attributed to random variation. Consequently, “p-hacking” has resulted in replication crises, especially in genomic research that utilizes DNA microarrays.
Risk of bias
The risk of bias varied considerably between the individual criteria and studies. Low risk criteria were determined to be the clear inclusion criteria, the reliability and validity of the epigenetic age measurement method, and the statistical analyses. 83.33% of the studies showed high risk of bias due to failure to identify potentially confounding factors and inadequate approach to them. Only one-third of the studies showed a low risk of bias on the criterion of standardized and objective disturbance diagnostics. Due to a lack of information, the remaining studies had an uncertain risk in this criterion. Seven of the 12 studies showed a lower risk of bias in more than 50% of the criteria, whereas only two studies showed a low risk of bias in more than 80% of the criteria.
Data synthesis and assessment of evidence quality
For each disease, a significant effect was found in at most one study and that only in specific brain areas or subgroup studies. Replications are needed to confirm the results. Table 1 shows the evidence profile of the individual outcomes with the assessment of evidence quality. A maximum of one study each showed significant results of accelerated aging in older BAD patients in the hippocampus (1/1), depression in the prefrontal cortex and subcortical areas (1/3), PTSD in the motor cortex with an interaction effect with SNP (1/1), alcohol addiction in men in the motor cortex (1/1), and significantly slowed aging in the frontal cortex in people with schizophrenia (1/4) and alcohol addiction (1/2). It is important to note that the quality of evidence for all outcomes must be classified as very low, which is due to the cross-sectional study design, an increased risk of bias, inconsistent, partly indirect results, small sample sizes and possible publication bias.
Conclusions
Our structured review provides the first systematic overview of published data on the role of epigenetic aging in mental disorders, including the calculation of effect sizes for significant results of the reviewed studies. Results of our analyses show only a few significant effect sizes of published data. Importantly, however, we detected significant effect sizes for data from studies, which included large sample sizes, used both brain tissue and peripheral blood samples for epigenetic analyses, targeted markers of epigenetic aging in the frontal cortex, and focused on schizophrenia and depressive disorders. Both Horvath’s and Hannum’s and Levine’s epigenetic clock models proved to be valid conceptual bases for research on epigenetic aging in patients with mental disorders. Since data on the relevance of the age of patients for epigenetic aging is sparse, this issue needs to be investigated in detail in future studies on aberrant functions of the epigenetic clock in mental disorders. Moreover, the issue of putative therapeutic consequence from knowledge of changes in epigenetic aging in patients with mental disorders needs to be addressed. Controlled longitudinal clinical trials are required to clarify whether neuropsychological interventions, psychotherapy, and pharmacological treatment may reverse abnormal epigenetic aging associated with mental disorders.
The key advantage of epigenetic clock models is that it is not necessary to obtain biopsy material from the brain to measure the valid biological age of a subject. At the same time, however, one should be very aware that the measurement of a few hundred selected DNA methylation markers provides only a tiny insight into the epigenomic changes that most likely take place in the context of complex psychiatric diseases and gene regulation changes in the central nervous system.
We propose that the results of our structured review may help to guide successful future methodological approaches to key functions of the epigenetic clock in different mental disorders.
Data availability
All data generated during this study are results of analyses of previously published data sources. All data generated are included in this published article [and its supplementary information files].
Abbreviations
- ANOVA:
-
Analysis of Variance
- BAD:
-
Bipolar Affective Disorder
- CpG:
-
Cytosine-phosphate-guanine
- DNAm:
-
DNA methylation
- DNMTs:
-
DNA methyl transferases
- GEO:
-
Gene Expression Omnibus
- GRADE:
-
Grading of Recommendations, Assessment, Development and Evaluation
- KL:
-
Klotho
- MD:
-
Major depression
- OCD:
-
Obsessive-compulsive disorder
- PICO:
-
Population, Intervention/Exposure, Comparison, Outcome
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PTSD:
-
Posttraumatic Stress Disorder
- SNP:
-
Single Nucleotide Polymorphism
- SZA:
-
Schizoaffective disorder
- WHO:
-
World Health Organization
References
Lipps H-J, Postberg J, Jackson DA (2010) Epigenetics, Disease and Behaviour, vol 48. Portland Press, London
Aging and health [https://www.who.int/news-room/fact-sheets/detail/aging-and-health]
Piefke M, Onur OA, Fink GR (2012) Aging-related changes of neural mechanisms underlying visual-spatial working memory. Neurobiol Aging 33(7):1284–1297
Lopez-Otin C, Blasco MA, Partridge L, Serrano M, Kroemer G (2013) The hallmarks of aging. Cell 153(6):1194–1217
Lessel D, Kubisch C (2019) Hereditary Syndromes with Signs of Premature Aging. Dtsch Arztebl Int 116(29–30):489–496
Schnabel F, Kornak U, Wollnik B (2021) Premature aging disorders: A clinical and genetic compendium. Clin Genet 99(1):3–28
Darrow SM, Verhoeven JE, Révész D, Lindqvist D, Penninx BW, Delucchi KL, Wolkowitz OM, Mathews CA (2016) The Association Between Psychiatric Disorders and Telomere Length: A Structured review Involving 14,827 Persons. Psychosom Med 78(7):776–787
Wertz J, Caspi A, Ambler A, Broadbent J, Hancox RJ, Harrington H, Hogan S, Houts RM, Leung JH, Poulton R et al (2021) Association of History of Psychopathology With Accelerated Aging at Midlife. JAMA Psychiat 78(5):530–539
Walker ER, McGee RE, Druss BG (2015) Mortality in mental disorders and global disease burden implications: a systematic review and structured review. JAMA Psychiat 72(4):334–341
Booth LN, Brunet A (2016) The Aging Epigenome. Mol Cell 62(5):728–744
Zhang W, Qu J, Liu GH, Belmonte JCI (2020) The aging epigenome and its rejuvenation. Nat Rev Mol Cell Biol 21(3):137–150
Postberg J, Lipps HJ, Cremer T (2010) Evolutionary origin of the cell nucleus and its functional architecture. Essays Biochem 48(1):1–24
Bird AP (1986) CpG-rich islands and the function of DNA methylation. Nature 321(6067):209–213
Biliya S, Bulla LA Jr (2010) Genomic imprinting: the influence of differential methylation in the two sexes. Exp Biol Med (Maywood) 235(2):139–147
Hackett JA, Surani MA (2013) DNA methylation dynamics during the mammalian life cycle. Philos Trans R Soc Lond B Biol Sci 368(1609):20110328
Hermann A, Gowher H, Jeltsch A (2004) Biochemistry and biology of mammalian DNA methyltransferases. Cell Mol Life Sci 61(19–20):2571–2587
Hirasawa R, Feil R (2010) Genomic imprinting and human disease. Essays Biochem 48(1):187–200
Smith ZD, Meissner A (2013) DNA methylation: roles in mammalian development. Nat Rev Genet 14(3):204–220
Roth TL, Roth ED, Sweatt JD (2010) Epigenetic regulation of genes in learning and memory. Essays Biochem 48(1):263–274
McGowan PO, Szyf M (2010) Environmental epigenomics: understanding the effects of parental care on the epigenome. Essays Biochem 48(1):275–287
Jones MJ, Goodman SJ, Kobor MS (2015) DNA methylation and healthy human aging. Aging Cell 14(6):924–932
Murgatroyd C, Wu Y, Bockmühl Y, Spengler D (2010) The Janus face of DNA methylation in aging. Aging (Albany NY) 2(2):107–110
Bocklandt S, Lin W, Sehl ME, Sánchez FJ, Sinsheimer JS, Horvath S, Vilain E (2011) Epigenetic predictor of age. PLoS ONE 6(6):e14821
Horvath S, Raj K (2018) DNA methylation-based biomarkers and the epigenetic clock theory of aging. Nat Rev Genet 19(6):371–384
Oblak L, van der Zaag J, Higgins-Chen AT, Levine ME, Boks MP (2021) A systematic review of biological, social and environmental factors associated with epigenetic clock acceleration. Aging Res Rev 69:101348
Horvath S (2013) DNA methylation age of human tissues and cell types. Genome Biol 14(10):R115
Horvath S (2015) Erratum to: DNA methylation age of human tissues and cell types. Genome Biol 16(1):96
Hannum G, Guinney J, Zhao L, Zhang L, Hughes G, Sadda S, Klotzle B, Bibikova M, Fan JB, Gao Y et al (2013) Genome-wide methylation profiles reveal quantitative views of human aging rates. Mol Cell 49(2):359–367
Levine ME, Lu AT, Quach A, Chen BH, Assimes TL, Bandinelli S, Hou L, Baccarelli AA, Stewart JD, Li Y et al (2018) An epigenetic biomarker of aging for lifespan and healthspan. Aging (Albany NY) 10(4):573–591
Liu C, Jiao C, Wang K, Yuan N (2018) DNA Methylation and Psychiatric Disorders. Prog Mol Biol Transl Sci 157:175–232
Grodstein F, Lemos B, Yu L, Klein HU, Iatrou A, Buchman AS, Shireby GL, Mill J, Schneider JA, De Jager PL et al (2021) The association of epigenetic clocks in brain tissue with brain pathologies and common aging phenotypes. Neurobiol Dis 157:105428
Moola S, Munn Z, Tufanuru C, Aromataris E, Sears K, Sfetcu R, Currie M, Lisy K, Qureshi R, Mattis P, Mu PF (ed.) (2020) Chapter 7: Systematic reviews of etiology and risk: In: JBI Manual for Evidence Synthesis (https://synthesismanual.jbi.global): The Joanna Briggs Institute: ISBN 978-0-6488488-2-0: https://doi.org/10.46658/JBIMES-24-06
Schünemann H, Brożek J, Guyatt G, Oxman A (2013) GRADE handbook for grading quality of evidence and strength of recommendations. https://gdt.gradepro.org/app/handbook/handbook.html
Sterling TD (1959) Publication Decisions and their Possible Effects on Inferences Drawn from Tests of Significance—or Vice Versa. J Am Stat Assoc 54(285):30–34
Meerpohl JJ, Langer G, Perleth M, Gartlehner G, Kaminski-Hartenthaler A, Schünemann H (2012) GRADE guidelines: 3. Rating the quality of evidence (confidence in the estimates of effect). Z Evid Fortbild Qual Gesundhwes 106(6):449–456
Fries GR, Bauer IE, Scaini G, Valvassori SS, Walss-Bass C, Soares JC, Quevedo J (2020) Accelerated hippocampal biological aging in bipolar disorder. Bipolar Disord 22(5):498–507
Fries GR, Bauer IE, Scaini G, Wu MJ, Kazimi IF, Valvassori SS, Zunta-Soares G, Walss-Bass C, Soares JC, Quevedo J (2017) Accelerated epigenetic aging and mitochondrial DNA copy number in bipolar disorder. Transl Psychiatry 7(12):1283
Han LKM, Aghajani M, Clark SL, Chan RF, Hattab MW, Shabalin AA, Zhao M, Kumar G, Xie LY, Jansen R et al (2018) Epigenetic Aging in Major Depressive Disorder. Am J Psychiatry 175(8):774–782
Li Z, He Y, Ma X, Chen X (2018) Epigenetic age analysis of brain in major depressive disorder. Psychiatry Res 269:621–624
Wolf EJ, Chen CD, Zhao X, Zhou Z, Morrison FG, Daskalakis NP, Stone A, Schichman S, Grenier JG, Fein-Schaffer D et al (2021) Klotho, PTSD, and advanced epigenetic age in cortical tissue. Neuropsychopharmacology 46(4):721–730
de Oliveira KC, Camilo C, Gastaldi VD, Sant’Anna Feltrin A, Lisboa BCG (2021) de Jesus Rodrigues de Paula V, Moretto AC, Lafer B, Hoexter MQ, Miguel EC et al. Brain areas involved with obsessive-compulsive disorder present different DNA methylation modulation. BMC Genom Data 22(1):45–45
McKinney BC, Lin H, Ding Y, Lewis DA, Sweet RA (2017) DNA methylation evidence against the accelerated aging hypothesis of schizophrenia. NPJ Schizophr 3:13
McKinney BC, Lin H, Ding Y, Lewis DA, Sweet RA (2018) DNA methylation age is not accelerated in brain or blood of subjects with schizophrenia. Schizophr Res 196:39–44
Voisey J, Lawford BR, Morris CP, Wockner LF, Noble EP, Young RM, Mehta D (2017) Epigenetic analysis confirms no accelerated brain aging in schizophrenia. NPJ Schizophr 3(1):26
Wu X, Ye J, Wang Z, Zhao C (2021) Epigenetic Age Acceleration Was Delayed in Schizophrenia. Schizophr Bull 47(3):803–811
Viana J, Hannon E, Dempster E, Pidsley R, Macdonald R, Knox O, Spiers H, Troakes C, Al-Saraj S, Turecki G et al (2017) Schizophrenia-associated methylomic variation: molecular signatures of disease and polygenic risk burden across multiple brain regions. Hum Mol Genet 26(1):210–225
Rosen AD, Robertson KD, Hlady RA, Muench C, Lee J, Philibert R, Horvath S, Kaminsky ZA, Lohoff FW (2018) DNA methylation age is accelerated in alcohol dependence. Transl Psychiatry 8(1):182
Gilabert-Juan J, Varea E, Guirado R, Blasco-Ibanez JM, Crespo C, Nacher J (2012) Alterations in the expression of PSA-NCAM and synaptic proteins in the dorsolateral prefrontal cortex of psychiatric disorder patients. Neurosci Lett 530(1):97–102
Larsen NY, Vihrs N, Moller J, Sporring J, Tan X, Li X, Ji G, Rajkowska G, Sun F, Nyengaard JR (2022) Layer III pyramidal cells in the prefrontal cortex reveal morphological changes in subjects with depression, schizophrenia, and suicide. Transl Psychiatry 12(1):363
Zhang L, Verwer RWH, Zhao J, Huitinga I, Lucassen PJ, Swaab DF (2021) Changes in glial gene expression in the prefrontal cortex in relation to major depressive disorder, suicide and psychotic features. J Affect Disord 295:893–903
Glienke K, Willmund GD, Zimmermann P, Piefke M (2017) Complex real life-related prospective memory in soldiers with and without post-traumatic stress disorder. J Trauma Stress Disor Treat 6(3). https://doi.org/10.4172/2324-8947.1000176
Schulte-Ruther M, Greimel E, Markowitsch HJ, Kamp-Becker I, Remschmidt H, Fink GR, Piefke M (2011) Dysfunctions in brain networks supporting empathy: an fMRI study in adults with autism spectrum disorders. Soc Neurosci 6(1):1–21
Johnston-Wilson NL, Sims CD, Hofmann JP, Anderson L, Shore AD, Torrey EF, Yolken RH (2000) Disease-specific alterations in frontal cortex brain proteins in schizophrenia, bipolar disorder, and major depressive disorder. The Stanley Neuropathology Consortium Mol Psychiatry 5(2):142–149
Beblo T, Kater L, Baetge S, Driessen M, Piefke M (2017) Memory performance of patients with major depression in an everyday life situation. Psychiatry Res 248:28–34
Klimek V, Schenck JE, Han H, Stockmeier CA, Ordway GA (2002) Dopaminergic abnormalities in amygdaloid nuclei in major depression: a postmortem study. Biol Psychiatry 52(7):740–748
Zangen A, Nakash R, Overstreet DH, Yadid G (2001) Association between depressive behavior and absence of serotonin-dopamine interaction in the nucleus accumbens. Psychopharmacology 155(4):434–439
Uranova NA, Vostrikov VM, Orlovskaya DD, Rachmanova VI (2004) Oligodendroglial density in the prefrontal cortex in schizophrenia and mood disorders: a study from the Stanley Neuropathology Consortium. Schizophr Res 67(2–3):269–275
Yusupov N, Dieckmann L, Erhart M, Sauer S, Rex-Haffner M, Kopf-Beck J, Bruckl TM, Czamara D, Binder EB (2023) Transdiagnostic evaluation of epigenetic age acceleration and burden of psychiatric disorders. Neuropsychopharmacology 48(9):1409–1417. https://doi.org/10.1038/s41386-023-01579-3
Ly K, Walker C, Berry S, Snell R, Marks E, Thayer Z, Atatoa-Carr P, Morton S (2019) Telomere length in early childhood is associated with sex and ethnicity. Sci Rep 9(1):10359
van Dongen J, Gordon SD, McRae AF, Odintsova VV, Mbarek H, Breeze CE, Sugden K, Lundgren S, Castillo-Fernandez JE, Hannon E et al (2021) Identical twins carry a persistent epigenetic signature of early genome programming. Nat Commun 12(1):5618
Jaffe AE, Gao Y, Deep-Soboslay A, Tao R, Hyde TM, Weinberger DR, Kleinman JE (2016) Mapping DNA methylation across development, genotype and schizophrenia in the human frontal cortex. Nat Neurosci 19(1):40–47
Wockner LF, Noble EP, Lawford BR, Young RM, Morris CP, Whitehall VL, Voisey J (2014) Genome-wide DNA methylation analysis of human brain tissue from schizophrenia patients. Transl Psychiatry 4(1):e339
Pidsley R, Viana J, Hannon E, Spiers H, Troakes C, Al-Saraj S, Mechawar N, Turecki G, Schalkwyk LC, Bray NJ et al (2014) Methylomic profiling of human brain tissue supports a neurodevelopmental origin for schizophrenia. Genome Biol 15(10):483
Torabi Moghadam B, Etemadikhah M, Rajkowska G, Stockmeier C, Grabherr M, Komorowski J, Feuk L, Carlström EL (2019) Analyzing DNA methylation patterns in subjects diagnosed with schizophrenia using machine learning methods. J Psychiatr Res 114:41–47
Murphy TM, Crawford B, Dempster EL, Hannon E, Burrage J, Turecki G, Kaminsky Z, Mill J (2017) Methylomic profiling of cortex samples from completed suicide cases implicates a role for PSORS1C3 in major depression and suicide. Transl Psychiatry 7(1):e989
Guintivano J, Aryee MJ, Kaminsky ZA (2013) A cell epigenotype specific model for the correction of brain cellular heterogeneity bias and its application to age, brain region and major depression. Epigenetics 8(3):290–302
Chen C, Zhang C, Cheng L, Reilly JL, Bishop JR, Sweeney JA, Chen HY, Gershon ES, Liu C (2014) Correlation between DNA methylation and gene expression in the brains of patients with bipolar disorder and schizophrenia. Bipolar Disord 16(8):790–799
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was conducted using own institutional means (Witten/Herdecke University to Jan Postberg and Martina Piefke).
Author information
Authors and Affiliations
Contributions
MS together with JP conducted the initial literature screening and analyses, with statistical refinement by VN and MP. JP and MP provided the project supervision and guidance. JP and MP wrote the paper, with assistance from VN, LW and MS. VN and MP calculated the effect sizes.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Relevance of this study (in simple language)
People often wonder whether our traits come from our genes (nature) or our environment (nurture). This question is important for understanding how we age and why some people develop mental illnesses. Epigenetics is a field that looks at how the regulation of our genes are influenced by our environment. Scientists use something called "epigenetic clocks" to measure how our genes age (biological age) compared to our actual age (chronological age). We looked at studies that explore how mental illnesses might be related to how our genes age. We searched through lots of research papers to find the ones that looked at this connection. We focused on studies with big groups of people, ones that studied both brain tissue and blood, and those that looked at specific parts of the brain, like the frontal cortex. We paid special attention to studies about schizophrenia and depression. We found that there weren't many studies that showed clear results, but some interesting findings stood out. The most promising studies were the ones with lots of participants, those that looked at both brain tissue and blood, and those that focused on the frontal cortex and mental illnesses like schizophrenia and depression. Even though we didn't find many clear answers in the studies we looked at, it's clear that more research is needed. By studying larger groups of people, looking at different parts of the brain, and focusing on specific mental illnesses, we can learn more about how our genes age and why some people develop mental health problems. This could help us find better ways to diagnose and treat these conditions in the future.
Supplementary information
Below is the link to the electronic supplementary material.
10048_2024_771_MOESM1_ESM.xlsx
Supplementary file1 Table S1. File ‘Table_S1.xls’ contains a technical comparison between the analyzed studies. This table provides a technical comparison of the studies analyzed in the research, focusing on various aspects such as the disorder studied, data sources, study groups, genotyping methods, DNA methylation analysis, mitochondrial DNA copy number assessment, telomere length evaluation, added sample information, epigenetic clock models used, number of CpGs analyzed, GEO datasets used, and sources of the studies. (XLSX 14 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Postberg, J., Schubert, M.T., Nin, V. et al. A perspective on epigenomic aging processes in the human brain and their plasticity in patients with mental disorders – a systematic review. Neurogenetics (2024). https://doi.org/10.1007/s10048-024-00771-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10048-024-00771-x