Abstract
Purpose
The objective of this study is to evaluate the safety and long-term outcomes of GORE Synecor™ in ventral hernia repair (VHR).
Methods
This retrospective, single-center case review analyzed outcomes in patients who underwent VHR with Synecor from May 2016 to December 2022. Primary outcomes were hernia recurrence and mesh infection rates. Secondary outcomes were 30-day morbidity, 30-day mortality, 30-day readmission, re-operation, surgical-site infection (SSI) and occurrence (SSO) rates, and occurrences requiring intervention (SSOI).
Results
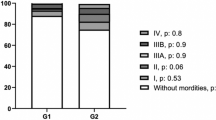
278 patients were identified. Mean follow-up was 24.1 (0.2–87.1) months. Mean hernia defect size was 63.4 (± 77.2) cm2. Overall hernia recurrence and mesh infection rates were 5.0% and 1.4% respectively. No mesh infections required full explantation. We report the following overall rates: 13.3% 30-day morbidity, 4.7% 30-day readmission, 2.9% re-operation, 7.2% SSI, 6.1% SSO, and 2.9% SSOI. 30-day morbidity was significantly higher in non-clean (42.1% vs 11.2%, p < 0.01), onlay (OL) mesh (37.0% vs preperitoneal (PP) 16.4%, p = 0.05 vs retrorectus (RR) 15.0%, p < 0.05 vs intraperitoneal (IP) 5.2%, p < 0.001), and open cases (23.5% vs 3.1% laparoscopic vs 4.4% robotic, p < 0.01). SSI rates were significantly higher in non-clean (31.6% vs 5.4%, p < 0.001), OL mesh (29.6% vs RR 11.3%, p < 0.05 vs PP 5.5%, p < 0.01 vs IP 0.0%, p < 0.001), and open cases (15.2% vs 0% laparoscopic vs 0% robotic, p < 0.05).
Conclusion
Long-term performance of a novel hybrid mesh in VHR demonstrates a low recurrence rate and favorable safety profile in various defect sizes and mesh placement locations.
Similar content being viewed by others
Data availability
The data presented in this study is available upon request from the corresponding author.
References
Kohler A, Lavanchy JL, Lenoir U, Kurmann A, Candinas D, Beldi G (2019) Effectiveness of prophylactic intraperitoneal mesh implantation for prevention of incisional hernia in patients undergoing open abdominal surgery. JAMA Surg 154(2):109–115. https://doi.org/10.1001/jamasurg.2018.4221
Bedewi MA, El-Sharkawy MS, Al Boukai AA, Al-Nakshabandi N (2012) Prevalence of adult paraumbilical hernia. Assessment by high-resolution sonography: a hospital-based study. Hernia 16(1):59–62. https://doi.org/10.1007/s10029-011-0863-4
Sneiders D, Yurtkap Y, Kroese LF, Kleinrensink G, Lange JF, Gillion JF (2019) Risk factors for incarceration in patients with primary abdominal wall and incisional hernias: a prospective study in 4472 patients. World J Surg 43(8):1906–1913. https://doi.org/10.1007/s00268-019-04989-x
Luijendijk RW, Hop WCJ, van den Tol MP et al (2000) A comparison of suture repair with mesh repair for incisional hernia. NEJM 343(6):392–398. https://doi.org/10.1056/nejm200008103430603
Burger JWA, Luijendijk RW, Hop WCJ, Halm JA, Verdaasdonk EGG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240(4):578–585. https://doi.org/10.1097/01.sla.0000141193.08524.e7
Sauerland S, Schmedt CG, Lein S, Leibl BJ, Bittner R (2005) Primary incisional hernia repair with or without polypropylene mesh: a report on 384 patients with 5-year follow-up. Langenbecks Arch Surg 390(5):408–412. https://doi.org/10.1007/s00423-005-0567-2
Khansa I, Janis JE (2019) The 4 principles of complex abdominal wall reconstruction. Plast Reconstr Surg - Glob Open. https://doi.org/10.1097/gox.0000000000002549
López-Cano M, Martin-Dominguez LA, Pereira JA, Armengol-Carrasco M, García-Alamino JM (2018) Balancing mesh-related complications and benefits in primary ventral and incisional hernia surgery. A meta-analysis and trial sequential analysis. PLoS ONE 13(6):e0197813. https://doi.org/10.1371/journal.pone.0197813
Mathes T, Walgenbach M, Siegel R (2016) Suture versus mesh repair in primary and incisional ventral hernias: a systematic review and meta-analysis. World J Surg 40(4):826–835. https://doi.org/10.1007/s00268-015-3311-2
Nguyen MT, Berger RL, Hicks SC, Davila JA, Li LT, Kao LS, Liang MK (2014) Comparison of outcomes of synthetic mesh vs suture repair of elective primary ventral herniorrhaphy. JAMA Surg 149(5):415. https://doi.org/10.1001/jamasurg.2013.5014
FitzGerald JF, Kumar AS (2014) Biologic versus synthetic mesh reinforcement: what are the pros and cons? Clin Colon Rectal Surg 27(04):140–148. https://doi.org/10.1055/s-0034-1394155
Baylón K, Rodríguez-Camarillo P, Elías-Zúñiga A, Díaz-Elizondo JA, Gilkerson R, Lozano K (2017) Past, present and future of surgical meshes: a review. Membr (Basel) 7(3):47. https://doi.org/10.3390/membranes7030047
Lake SP, Stoikes NFN, Badhwar A, Deeken CR (2019) Contamination of hybrid hernia meshes compared to bioresorbable Phasix™ Mesh in a rabbit subcutaneous implant inoculation model. Ann Med Surg 46:12–16. https://doi.org/10.1016/j.amsu.2019.08.004
Reid CM, Jacobsen GR (2018) A current review of hybrid meshes in abdominal wall reconstruction. Plast Reconstr Surg 142(3S):92S. https://doi.org/10.1097/PRS.0000000000004860
Rios-Diaz AJ, Hitchner M, Christopher AN, Broach R, Cunning JR, Fischer JP (2021) Early clinical and patient-reported outcomes of a new hybrid mesh for incisional hernia repair. J Surg Res 265:49–59. https://doi.org/10.1016/j.jss.2021.03.030
Parikh RS, Faulkner JD, Bilezikian JA, Hooks WB, Hope WW (2021) A short-term preliminary evaluation of ventral hernia repair using a new prosthetic mesh. Int J Abdom Wall Hernia Surg 4(3):90. https://doi.org/10.4103/ijawhs.ijawhs_48_20
Linn JG, Mallico EJ, Doerhoff CR, Grantham DW, Washington RG (2023) Evaluation of long-term performance of an intraperitoneal biomaterial in the treatment of ventral hernias. Surg Endosc 37(5):3455–3462. https://doi.org/10.1007/s00464-022-09803-9
Kao AM, Arnold MR, Augenstein VA, Heniford BT (2018) Prevention and treatment strategies for mesh infection in abdominal wall reconstruction. Plast Reconstr Surg 142(3S):149S. https://doi.org/10.1097/PRS.0000000000004871
Whitehead-Clarke T, Windsor A (2021) Surgical site infection: the scourge of abdominal wall reconstruction. Surg Infect (Larchmt) 22(4):357–362. https://doi.org/10.1089/sur.2020.325
Pande T, Naidu CS (2020) Mesh infection in cases of polypropylene mesh hernioplasty. Hernia 24(4):849–856. https://doi.org/10.1007/s10029-020-02142-5
Hodgkinson JD, Maeda Y, Leo CA, Warusavitarne J, Vaizey CJ (2017) Complex abdominal wall reconstruction in the setting of active infection and contamination: a systematic review of hernia and fistula recurrence rates. Colorectal Dis 19(4):319–330. https://doi.org/10.1111/codi.13609
Plymale MA, Davenport DL, Walsh-Blackmore S, Hess J, Griffiths WS, Plymale MC, Totten CF, Roth JS (2020) Costs and complications associated with infected mesh for ventral hernia repair. Surg Infect (Larchmt) 21(4):344–349. https://doi.org/10.1089/sur.2019.183
Bachman S, Ramshaw B (2008) Prosthetic material in ventral hernia repair: how do I choose? Surg Clin North Am 88(1):101–112. https://doi.org/10.1016/j.suc.2007.11.001
Shankaran V, Weber DJ, Reed RL, Luchette FA (2011) A review of available prosthetics for ventral hernia repair. Ann Surg 253(1):16–26. https://doi.org/10.1097/SLA.0b013e3181f9b6e6
Rosen MJ, Bauer JJ, Harmaty M et al (2017) Multicenter, prospective, longitudinal study of the recurrence, surgical site infection, and quality of life after contaminated ventral hernia repair using biosynthetic absorbable mesh: the COBRA study. Ann Surg 265(1):205. https://doi.org/10.1097/SLA.0000000000001601
Lindmark M, Löwenmark T, Strigård K, Gunnarsson U (2023) Ventral hernia repair with concurrent intra-abdominal surgery: Results from an eleven-year population-based cohort in Sweden. Am J Surg 226(3):360–364. https://doi.org/10.1016/j.amjsurg.2023.06.006
Bittner JG, El-Hayek K, Strong AT, LaPinska MP, Yoo JS, Pauli EM, Kroh M (2018) First human use of hybrid synthetic/biologic mesh in ventral hernia repair: a multicenter trial. Surg Endosc 32(3):1123–1130. https://doi.org/10.1007/s00464-017-5715-6
Lewis R, Forman B, Preston M, Heidel E, Alvoid-Preston B, Ramshaw B (2022) The use of a novel synthetic resorbable scaffold (TIGR Matrix®) in a clinical quality improvement (CQI) effort for abdominal wall reconstruction (AWR). Hernia 26(2):437–445. https://doi.org/10.1007/s10029-020-02221-7
Petro CC, Nahabet EH, Criss CN, Orenstein SB, von Recum HA, Novitsky YW, Rosen MJ (2015) Central failures of lightweight monofilament polyester mesh causing hernia recurrence: a cautionary note. Hernia 19(1):155–159. https://doi.org/10.1007/s10029-014-1237-5
Cobb WS, Warren JA, Ewing JA, Burnikel A, Merchant M, Carbonell AM (2015) Open retromuscular mesh repair of complex incisional hernia: predictors of wound events and recurrence. JACS 220(4):606–613. https://doi.org/10.1016/j.jamcollsurg.2014.12.055
Maskal S, Miller B, Ellis R, Phillips S, Prabhu A, Beffa L, Krpata D, Rosenblatt S, Rosen M, Petro CC (2023) Mediumweight polypropylene mesh fractures after open retromuscular ventral hernia repair: incidence and associated risk factors. Surg Endosc 37(7):5438–5443. https://doi.org/10.1007/s00464-023-10039-4
Wang See C, Kim T, Zhu D (2020) Hernia mesh and hernia repair: a review. Eng Regeneration 1:19–33. https://doi.org/10.1016/j.engreg.2020.05.002
Zhu LM, Schuster P, Klinge U (2015) Mesh implants: an overview of crucial mesh parameters. World J Gastrointest Surg 7(10):226–236. https://doi.org/10.4240/wjgs.v7.i10.226
Klinge U, Klosterhalfen B, Conze J, Limberg W, Obolenski B, Ottinger AP, Schumpelick V (1998) Modified mesh for hernia repair that is adapted to the physiology of the abdominal wall. Eur J Surg 164(12):951–960. https://doi.org/10.1080/110241598750005138
Sharbaugh ME, Patel PB, Zaman JA, Ata A, Feustel P, Singh K, Singh TP (2021) Robotic ventral hernia repair: a safe and durable approach. Hernia 25(2):305–312. https://doi.org/10.1007/s10029-019-02074-9
Sugiyama G, Chivukula S, Chung PJ, Alfonso A (2015) Robot assisted transabdominal preperitoneal ventral hernia repair. JSLS 19(4):00092. https://doi.org/10.4293/JSLS.2015.00092
Funding
No funding information to disclose for this project.
Author information
Authors and Affiliations
Contributions
Conceptualization: Jonathan Z Li, Ryan C Broderick, Garth R Jacobsen; Formal analysis and investigation: Graham J Spurzem, Jonathan Li; Writing—original draft preparation: Graham J Spurzem, Jonathan Z Li; Writing—review and editing: Graham J Spurzem, Ryan C Broderick, Santiago Horgan, Garth R Jacobsen; Supervision: Bryan J Sandler, Santiago Horgan, Garth R Jacobsen.
Corresponding author
Ethics declarations
Ethical approval
This retrospective case review study was approved by the University of California, San Diego Institutional Review Board.
Human and animal rights
This research study was conducted retrospectively from data obtained for clinical purposes. All procedures were performed as part of standard routine care. There were no procedures involving animals.
Informed consent
A waiver of informed consent was granted for this study by the University of California, San Diego Institutional Review Board.
Conflict of interest
Dr. Broderick is a consultant for Stryker Corporation. Dr. Sandler is a consultant for Intuitive Surgical and Boston Scientific. Dr. Horgan is a consultant for Stryker Corporation, Intuitive Surgical, Fortimedix Surgical, and Alume Biosciences. Dr. Jacobsen is a consultant for Gore Medical and Viacyte. Drs. Spurzem & Li have no disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Spurzem, G.J., Broderick, R.C., Li, J.Z. et al. Maximizing mesh mileage: evaluating the long-term performance of a novel hybrid mesh for ventral hernia repair. Hernia (2024). https://doi.org/10.1007/s10029-024-02995-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10029-024-02995-0