Abstract
Introduction
Patients who require highly complex abdominal wall hernia repair with composite soft tissue free flap coverage represent the most challenging population, and the most difficult to definitively treat. For many, this combined procedure represents their last chance to restore any sense of normalcy to their lives. To date, patient reported post-operative outcomes have been limited in the literature, in particular, quality of life has been an under-reported component of successful management.
Methods
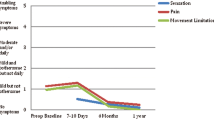
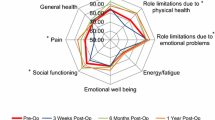
Patient-reported outcomes were analyzed using the 12-question HerQLes survey, a validated hernia-related quality of life survey to assess patient function after complex abdominal wall reconstruction. Using synthetic mesh for structural stability, and microsurgical flaps for soft tissue coverage, ten consecutive heterogeneous patients underwent repair of massive abdominal wall defects. Baseline preoperative HerQLes and numerical pain scores were then compared to those obtained postoperatively (at or greater than 6 months).
Results
All patients experienced improvement in their quality of life and pain scores post operatively with average follow-up at 15.9 months, even in those who experienced complications. All microsurgical flaps survived. There were no hernia recurrences.
Conclusion
Despite the extraordinary preoperative morbidity of massive abdominal wall defects, with an experienced General Surgery and Plastic Surgery multidisciplinary team, these highly complex patients are able to achieve a significant improvement in their pain and quality of life following repair and reconstruction with complex mesh hernia repair and microsurgical free tissue transfer.





Similar content being viewed by others
References
Gurunluoglu R et al (2016) Arteriovenous loop graft in abdominal wall reconstruction using free tissue transfer. J Plast Reconstr Aesthet Surg 69(11):1513–1515
Gurunluoglu R, Rosen MJ (2017) Recipient vessels for microsurgical flaps to the abdomen: a systematic review. Microsurgery 37:707–716
Hallock GG (2012) Delayed abdominal wall reconstruction of giant ventral hernias using the anterolateral thigh free flap for skin coverage. J Trauma Acute Care Surg 73(4):1028–1030
Kayano S et al (2012) Comparison of pedicled and free anterolateral thigh flaps for reconstruction of complex defects of the abdominal wall: review of 20 consecutive cases. J Plast Reconstr Aesthet Surg 65(11):1525–1529
Wong CH et al (2009) Reconstruction of complex abdominal wall defects with free flaps: indications and clinical outcome. Plast Reconstr Surg 124(2):500–509
Kim SW et al (2013) Reconstruction of infected abdominal wall defects using latissimus dorsi free flap. ANZ J Surg 83(12):948–953
Tukiainen E, Leppaniemi A (2011) Reconstruction of extensive abdominal wall defects with microvascular tensor fasciae latae flap. Br J Surg 98(6):880–884
Hahn E Jr, Lee ES, Keith JD (2016) A neurotized anterolateral thigh flap with a unique anastomosis to the gastroepiploic artery: a case report of a reconstruction of composite abdominal wall defect. Eplasty 16:ic29
Steffensen SM et al (2014) Latissimus dorsi free flap reconstruction of major abdominal defect in treatment of giant Marjolin’s ulcer: a short report focused on preoperative imaging. Acta Radiol Short Rep 3(1):2047981613516614
Kadoch V et al (2010) Latissimus dorsi free flap for reconstruction of extensive full-thickness abdominal wall defect. A case of desmoid tumor. J Visc Surg 147(2):e45–e48
Iida T et al (2013) Dynamic reconstruction of full-thickness abdominal wall defects using free innervated vastus lateralis muscle flap combined with free anterolateral thigh flap. Ann Plast Surg 70(3):331–334
Lv Y et al (2015) Abdominal wall reconstruction using a combination of free tensor fasciae lata and anterolateral thigh myocutaneous flap: a prospective study in 16 patients. Am J Surg 210(2):365–373
Sinna R et al (2010) Reconstruction of a full-thickness abdominal wall defect using an anterolateral thigh free flap. J Visc Surg 147(2):e49–e53
Bulic K et al (2008) Prosthetic mesh for infected abdominal wall defects? Report of a patient with a large full thickness abdominal wall defect and colostomy due to a gunshot wound. J Plast Reconstr Aesthet Surg 61(4):455–458
Servant JM, Arnault E, Revol M, Danino A (2006) Reconstruction of large thoracoabdominal defects using two-stage free tissue transfers and prosthetic materials. J Plast Reconstruct Aesthet Surg 59:360–365
Chevray PM, Singh NK (2003) Abdominal wall reconstruction with the free tensor fascia lata musculofasciocutaneous flap using intraperitoneal gastroepiploic recipient vessels. Ann Plast Surg 51(1):97–102
Grinsell D, Di Bella C, Choong PF (2012) Functional reconstruction of sarcoma defects utilising innervated free flaps. Sarcoma 2012:315190
Lin SJ, Butler CE (2010) Subtotal thigh flap and bioprosthetic mesh reconstruction for large, composite abdominal wall defects. Plast Reconstr Surg 125(4):1146–1156
Dorai AA, Halim AS (2007) Extended double pedicle free tensor fascia latae myocutaneous flap for abdominal wall reconstruction. Singap Med J 48(5):e141–e145
Bodin F, Dissaux B, Romain B, Rohr S, Brigand C (2015) Complex abdominal wall defect reconstruction using a latissimus dorsi free flap with mesh after malignant tumor resection. Microsurgery 37:38–43
Koshima I et al (1999) Dynamic reconstruction of the abdominal wall using a reinnervated free rectus femoris muscle transfer. Ann Plast Surg 43(2):199–203
Kuo YR et al (2004) One-stage reconstruction of large midline abdominal wall defects using a composite free anterolateral thigh flap with vascularized fascia lata. Ann Surg 239(3):352–358
Vranckx JJ et al (2015) Dynamic reconstruction of complex abdominal wall defects with the pedicled innervated vastus lateralis and anterolateral thigh PIVA flap. J Plast Reconstr Aesthet Surg 68(6):837–845
Krpata DM et al (2012) Design and initial implementation of HerQLes: a hernia-related quality-of-life survey to assess abdominal wall function. J Am Coll Surg 215(5):635–642
Kanters AE et al (2012) Modified hernia grading scale to stratify surgical site occurrence after open ventral hernia repairs. J Am Coll Surg 215(6):787–793
Blatnik JA, DM Krpata, Novitsky YW (2016) Transversus abdominis release as an alternative component separation technique for ventral hernia repair. JAMA Surg 151(4):383–384
Zarzaur BL et al (2011) Quality of life after abdominal wall reconstruction following open abdomen. J Trauma 70(2):285–291
Jensen KK (2017) Recovery after abdominal wall reconstruction. Dan Med J 64:3
Sosin M et al (2014) A patient-centered appraisal of outcomes following abdominal wall reconstruction: a systematic review of the current literature. Plast Reconstr Surg 133(2):408–418
Alleyne B et al (2017) Combined submuscular tissue expansion and anterior component separation technique for abdominal wall reconstruction: long-term outcome analysis. J Plast Reconstr Aesthet Surg 70:752–758
Acknowledgements
We would like to thank Pat Shoda and Susan Lopez for their photography expertise and assistance preparing this manuscript.
Funding
Michael Rosen MD receives research support from Intuitive and Miromatrix, and salary support from the Americas Hernia Society Quality Collaborative (AHSQC). David Krpata MD is a consultant for Medtronic. All other listed authors have no financial disclosures. No funding was received for this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
REA declares no conflict of interest. JG declares no conflict of interest. DK declares no conflict of interest. SR declares no conflict of interest. MR declares no conflict of interest. RG declares no conflict of interest.
Ethical approval
The article does not contain any identifiable information and the content is compliant with HIPPA regulations and human rights.
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all patients.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aliotta, R.E., Gatherwright, J., Krpata, D. et al. Complex abdominal wall reconstruction, harnessing the power of a specialized multidisciplinary team to improve pain and quality of life. Hernia 23, 205–215 (2019). https://doi.org/10.1007/s10029-019-01916-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-019-01916-w