Abstract
Purpose
Laparoscopic ventral hernia repair (LVHR) with intra-peritoneal mesh placement is standard surgical treatment of abdominal wall hernias. During laparoscopic re-intervention, we examined adhesions that develop after previous intra-peritoneal mesh placement and ascertained morbidity and risk of adverse events.
Methods
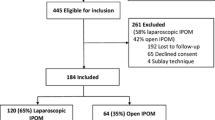
This is a retrospective, case-matched comparison of three patient groups—previous intra-peritoneal mesh (Group A), previous abdominal surgery (Group B) and no previous abdominal surgery (Group C). Matching was based on surgical procedure performed during laparoscopic re-intervention in Group A. Adhesions were described as grade, extent of previous mesh/scar involvement, involvement of abdominal quadrants and dissection technique required for adhesiolysis, each component being assigned value from 0 to 4. Total adhesion score (TAS) was generated as summative score for each patient (0 to 16). Access/adhesiolysis-related injuries, additional port requirement, deviations from planned surgery, operative time and length of hospital stay was noted. Relative risk of adverse events, i.e., inadvertent injuries and deviations from planned surgery, was calculated for Group A.
Results
Adhesion characteristics were most severe (highest TAS) in Group A. Access injuries occurred in 5, 4, 1.3% in Groups A, B, C, respectively. Adhesiolysis-related injury rate was 9%, 2.6% in Groups A, B, respectively. Relative risk of adverse events was 4 for Group A (compared to Groups B and C combined). Additional port requirement was highest for Group A. Mean operative time and length of hospital stay was significantly longer in Group A for LVHR.
Conclusions
Intra-peritoneal mesh placement is associated with adhesion formation that may increase risk during subsequent laparoscopic surgery.


Similar content being viewed by others
References
Sauerland S, Walgenbach M, Habermalz B, Seiler CM, Miserez M (2011) Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database Syst Rev 16(3):CD007781
Eker HH, Hansson BME, Buunen M, Janssen IMC, Pierik RE et al (2013) Laparoscopic vs open incisional hernia repair: a randomized clinical trial. JAMA Surg 148(3):259–263. doi:10.1001/jamasurg.2013.1466
Langbach O, Bukholm I, Benth JŠ, Røkke O (2015) Long term recurrence, pain and patient satisfaction after ventral hernia mesh repair. World J Gastrointest Surg 7(12):384–393. doi:10.4240/wjgs.v7.i12.384
Fortelny RH, Petter-Puchner AH, Glaser KS, Offner F et al (2010) Adverse effects of polyvinylidene fluoride-coated polypropylene mesh used for laparoscopic intraperitoneal onlay repair of incisional hernia. Br J Surg 97:7
Jenkins ED, Yom V, Melman L, Brunt LM, Eagon JC, Frisella MM, Matthews BD (2010) Prospective evaluation of adhesion characteristics to intraperitoneal mesh and adhesiolysis-related complications during laparoscopic re-exploration after prior ventral hernia repair. Surg Endosc 24:3002–3007
Halm JA, de Wall LL, Steyerberg EW, Jeekel J, Lange JF (2007) Intraperitoneal polypropylene mesh hernia repair complicates subsequent abdominal surgery. World J Surg 31:423–429
Zühlke HV, Lorenz EM, Straub EM, Savvas V (1990) Pathophysiology and classification of adhesions. Langenbecks Arch Chir Verh Dtsch Ges Chir (Suppl 2):1009–1016
Indrayan A (2012) Inference from means. In: Indrayan A (ed) Medical biostatistics, 3rd edn. CRC Press, Boca Raton
Silecchia G, Campanile FC, Sanchez L et al (2015) Laparoscopic ventral/incisional hernia repair: updated guidelines from the EAES and EHS endorsed Consensus Development Conference. Surg Endosc 29:2463–2484. doi:10.1007/s00464-015-4293-8
Mavros MN, Athanasiou S, Alexiou VG, Mitsikostas PK, Peppas G, Falagas ME (2011) Risk factors for mesh-related infections after hernia repair surgery: a meta-analysis of cohort studies. World J Surg 35(11):2389–2398
Lee J, Mabardy A, Kermani R, Lopez M, Pecquex N, McCluney A (2013) Laparoscopic vs open ventral hernia repair in the era of obesity. JAMA Surg 12:1–4
Forbes SS, Eskicioglu C, McLeod RS, Okrainec A (2009) Meta-analysis of randomized controlled trials comparing open and laparoscopic ventral and incisional hernia repair with mesh. Br J Surg 96:851–858
Moreau PE, Helmy N, Vons C (2012) Laparoscopic treatment of incisional hernia. State of the art in 2012. J Vasc Surg 149(5 Suppl):e40–e48
Mancini GA, Alexander AM (2013) Tissue ingrowth: the mesh–tissue interface: what do we know so far? In: Jacob BP, Ramshaw B (eds) The SAGES manual of hernia repair. Springer, New York
Suárez Grau JM, Chaves CR, Durantez FD, Jiménez MB (2014) Prostheses in laparoscopic ventral hernia repair. In: Bellido Luque JA, Suárez Grau JM (eds) Advances in laparoscopy of the abdominal wall hernia. Springer, London, pp 131–146
Grant SA (2013) Synthetic prosthetic choices in ventral hernia repair. In: Jacob BP, Ramshaw B (eds) The SAGES manual of hernia repair. Springer, New York
Chelala E, Debardemaeker Y, Elias B, Charara F, Dessily M, Allé JL (2010) Eighty-five redo surgeries after 733 laparoscopic treatments for ventral and incisional hernia: adhesion and recurrence analysis. Hernia 14(2):123–129
Wassenaar E, Schoenmaeckers E, Raymakers J, van der Palen J, Rakic S (2010) Mesh-fixation method and pain and quality of life after laparoscopic ventral or incisional hernia repair: a randomized trial of three fixation techniques. Surg Endosc 24(6):1296–1302
Holihan JL, Nguyen DH, Nguyen MT, Mo J et al (2016) Mesh location in open ventral hernia repair: a systematic review and network meta-analysis. World J Surg 40:89–99. doi:10.1007/s00268-015-3252-9
Adrales GL (2016) Abdominal wall spaces for mesh placement: onlay, sublay, underlay. In: Novitsky YW (ed) Hernia surgery current principles. Springer, Switzerland
Iqbal CW, Pham TH, Joseph A, Mai J, Thompson GB, Sarr MG (2007) Long-term outcome of 254 complex incisional hernia repairs using the modified Rives–Stoppa technique. World J Surg 31(12):2398–2404
Acknowledgements
We would gratefully like to acknowledge the contributions of Dr. Abhaya Indrayan and Ms. Laxmi Raghuvanshi to the statistical analysis of the data in this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. AS has no conflicts of interest to declare. Dr. PC has no conflicts of interest to declare. Dr. NSK has no conflicts of interest to declare. Dr. MB has no conflicts of interest to declare. Dr. VS has no conflicts of interest to declare. Dr. RK has no conflicts of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and animal rights
This study is a retrospective database analysis, and hence does not involve human or animal research.
Informed consent
For this type of study formal consent is not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sharma, A., Chowbey, P., Kantharia, N.S. et al. Previously implanted intra-peritoneal mesh increases morbidity during re-laparoscopy: a retrospective, case-matched cohort study. Hernia 22, 343–351 (2018). https://doi.org/10.1007/s10029-017-1686-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-017-1686-8