Abstract
Purpose
The choice of mesh and anchoring device in laparoscopic ventral hernia repair is controversial. Clinically important long-term properties of mesh and anchoring device such as mesh shrinkage have been sparsely investigated. Furthermore, the effect of various anchoring devices on mesh properties has never been examined.
Methods
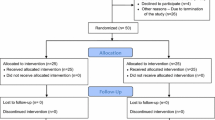
In 20 sheep, using laparoscopy, we inserted three PhysiomeshTM (large pore, lightweight) and three VentralightTMST (small pore, mediumweight), anchored with ProTackTM, SecurestrapTM or GlubranTM, respectively. After 6 and 12 months, 10 sheep at each time-point, we euthanized the animals, harvested the meshes with fascia, and measured the exact size and area of the mesh, expressing mesh shrinkage as a percentage of the initial area.
Results
The shrinkage of PhysiomeshTM was 35.7 %, 23.8 % and 17.7 % when anchored with ProtackTM, GlubranTM or SecurestrapTM, respectively. Shrinkage with ProtackTM was significantly higher than with either GlubranTM or SecurestrapTM, respectively (p<0.01 and p<0.01). The shrinkage of VentralightTMST was 19.3 %, 22.2 % and 19.6 % when anchored with ProtackTM, GlubranTM and SecurestrapTM, respectively (p>0.05 for all pairwise comparisons). Overall shrinkage of PhysiomeshTM anchored with ProtackTM was significantly higher for all comparisons (p<0.01).
Conclusion
Our results suggest that mesh shrinkage in sheep takes place within 6 months after implantation. A significant interaction between mesh and type of anchoring indicates that shrinkage may depend on both mesh properties and anchoring device. The results of the current study imply that the combined effect of mesh and anchoring device should be evaluated in future studies.




Similar content being viewed by others
References
Harslof SS, Wara P, Friis-Andersen H (2014) Fixation devices in laparoscopic ventral hernia repair: a review. Surg Technol Int 24:203–213
Zinther NB, Wara P, Friis-Andersen H (2010) Shrinkage of intraperitoneal onlay mesh in sheep: coated polyester mesh versus covered polypropylene mesh. Hernia 14:611–615
Bradley JF, 3rd, Williams KB, Wormer BA, Tsirline VB, Walters AL, Sing RF, Belyansky I, Heniford BT (2012) Preliminary results of surgical and quality of life outcomes of Physiomesh in an international, prospective study. Surg Technol Int 22:113–119
Deeken CR, Matthews BD (2013) Ventralight ST and SorbaFix versus physiomesh and securestrap in a porcine model. JSLS 17:549–559
Kukleta JF, Freytag C, Weber M (2012) Efficiency and safety of mesh fixation in laparoscopic inguinal hernia repair using n-butyl cyanoacrylate: long-term biocompatibility in over 1300 mesh fixations. Hernia 16:153–162
Morales-Conde S, Cadet H, Cano A, Bustos M, Martin J, Morales-Mendez S (2005) Laparoscopic ventral hernia repair without sutures–double crown technique: our experience after 140 cases with a mean follow-up of 40 months. Int Surg 90:S56–S62
Zinther NB, Wara P, Friis-Andersen H (2010) Intraperitoneal onlay mesh: an experimental study of adhesion formation in a sheep model. Hernia 14:283–289
Eriksen JR, Bech JI, Linnemann D, Rosenberg J (2008) Laparoscopic intraperitoneal mesh fixation with fibrin sealant (Tisseel) vs. titanium tacks: a randomised controlled experimental study in pigs. Hernia 12:483–491
Schug-Pass C, Sommerer F, Tannapfel A, Lippert H, Kockerling F (2009) The use of composite meshes in laparoscopic repair of abdominal wall hernias: are there differences in biocompatibily?: experimental results obtained in a laparoscopic porcine model. Surg Endosc 23:487–495
Reynvoet E, Chiers K, Van Overbeke I, Troisi R, Berrevoet F (2015) Intraperitoneal mesh devices for small midline hernias: mesh behavior in a porcine model. Hernia
Zogbi L, Trindade EN, Trindade MR (2013) Comparative study of shrinkage, inflammatory response and fibroplasia in heavyweight and lightweight meshes. Hernia 17:765–772
Weyhe D, Cobb W, Lecuivre J, Alves A, Ladet S, Lomanto D, Bayon Y (2015) Large pore size and controlled mesh elongation are relevant predictors for mesh integration quality and low shrinkage: systematic analysis of key parameters of meshes in a novel minipig hernia model. Int J Surg 22:46–53
Eriksen JR, Bisgaard T, Assaadzadeh S, Jorgensen LN, Rosenberg J (2013) Fibrin sealant for mesh fixation in laparoscopic umbilical hernia repair: 1-year results of a randomized controlled double-blinded study. Hernia
LeBlanc K (2015) Proper mesh overlap is a key determinant in hernia recurrence following laparoscopic ventral and incisional hernia repair. Hernia
Schreinemacher MH, van Barneveld KW, Dikmans RE, Gijbels MJ, Greve JW, Bouvy ND (2013) Coated meshes for hernia repair provide comparable intraperitoneal adhesion prevention. Surg Endosc 27:4202–4209
Misawa T, Sakamoto T, Kosuge M, Shiba H, Gocho T, Yanaga K (2009) Comparison of anchoring capacity of mesh fixation devices in ventral hernia surgery. Surg Laparosc Endosc Percutan Tech 19:345–347
Nguyen SQ, Divino CM, Buch KE, Schnur J, Weber KJ, Katz LB, Reiner MA, Aldoroty RA, Herron DM (2008) Postoperative pain after laparoscopic ventral hernia repair: a prospective comparison of sutures versus tacks. JSLS 12:113–116
Hollinsky C, Kolbe T, Walter I, Joachim A, Sandberg S, Koch T, Rulicke T, Tuchmann A (2010) Tensile strength and adhesion formation of mesh fixation systems used in laparoscopic incisional hernia repair. Surg Endosc 24:1318–1324
Ladurner R, Drosse I, Burklein D, Plitz W, Barbaryka G, Kirchhoff C, Kirchhoff S, Mutschler W, Schieker M, Mussack T (2011) Cyanoacrylate glue for intra-abdominal mesh fixation of polypropylene-polyvinylidene fluoride meshes in a rabbit model. J Surg Res 167:e157–e162
Clarke T, Katkhouda N, Mason RJ, Cheng BC, Algra J, Olasky J, Sohn HJ, Moazzez A, Balouch M (2011) Fibrin glue for intraperitoneal laparoscopic mesh fixation: a comparative study in a swine model. Surg Endosc 25:737–748
LeBlanc KA, Whitaker JM, Bellanger DE, Rhynes VK (2003) Laparoscopic incisional and ventral hernioplasty: lessons learned from 200 patients. Hernia 7:118–124
Kuehnert N, Kraemer NA, Otto J, Donker HC, Slabu I, Baumann M, Kuhl CK, Klinge U (2012) In vivo MRI visualization of mesh shrinkage using surgical implants loaded with superparamagnetic iron oxides. Surg Endosc 26:1468–1475
Acknowledgments
This study was supported by The Aase and Ejnar Danielsen Foundation, The A.P. Moeller Foundation and The Klein and wife foundation. The authors wish to acknowledge help from the staff of Aarhus University’s farm for experimental animal studies. The authors also wish to acknowledge associate professor Mogens Erlandsen, Section of Biostatistics, Department of Health, Aarhus University who helped with planning and conduction of the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Harsløf, S., Zinther, N., Harsløf, T. et al. Mesh shrinkage depends on mesh properties and anchoring device: an experimental long-term study in sheep. Hernia 21, 107–113 (2017). https://doi.org/10.1007/s10029-016-1528-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-016-1528-0