Abstract
Purpose
This scoping review explores various parameters of the mandible in progressive facial asymmetry (FA) in hemifacial microsomia (HFM) patients, highlighting its relationship with sex, population, and age group.
Methods
The review was based on a comprehensive search of PubMed, EBSCOhost, and Web of Science. Eligible studies that met the inclusion criteria form part of the selection study. The included studies were appraised using screening and quantitative criteria of mixed-method appraisal tools. The authors utilised a pre-set data extraction form to obtain information from the included studies.
Results
Eleven studies met the inclusion criteria. The mandible parameters used were angular measurements, chin point, ramal height, body length, and total length. There was no relationship between FA and sex in HFM patients in the included studies. Most of the studies were comprised of European participants (55%), followed by Americans (36%) and Chinese (9%). The age groups included in the selected studies were categorised as dentition age (18%), early-to-middle childhood (18%), and varied ages (64%). The data presented in this review only pertains to the anomalous characteristics recorded on the affected side in HFM patients. No concomitant control data was recorded in this review.
Conclusion
An assessment of the included studies revealed that FA does not increase with age in HFM. Hence, FA is non-progressive in HFM patients. This information is relevant to diagnosing and managing HFM patients. More reports are needed on the progression of FA in HFM patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hemifacial microsomia (HFM) is a congenital anomaly in which one-half of the face does not develop normally. HFM is derived from the first and second pharyngeal arches malformation [1]. It is the second most prevalent congenital craniofacial defect after cleft lip and palate (1: 3,500-5,600 in the United States of America) [2]. It has been speculated to be due to genetic, maternal, and environmental conditions leading to stapedial artery injury (replaced by an external carotid system in adults), dysgenesis of Meckel’s cartilage and aberrant migration of neural crest cells [3]. This defect is more evident in the jaw and ear areas, though the involvement of the eye, cheek, nerve, soft tissue, other cranial parts, and neck may accompany it. HFM can also be described as skeletal or soft-tissue defects or a combination of skeletal and soft-tissue defects [4]. Although HFM implies facial involvement only, individuals with HFM often have associated extracranial defects such as neurological, cardiac, genitourinary, pulmonary, gastrointestinal, and skeletal malformations [5,6,7,8,9]. In a clinical presentation, mandibular hypoplasia has been the cornerstone of this deformity with unilateral or bilateral microtia. Craniofacial growth in the affected patients depends on the extent of the deformity [1]. Mandibular size, shape, and location to the maxilla and base of the skull are determined by bone deposition and resorption on the periosteal and endosteal surfaces [10, 11]. The increase in vertical height of the ramus and its posterior movement occurs due to bone deposition on the posteroinferior surface and resorption on the anterior surface [10]. Resorption occurring along the anterior border of the ramus also adds to the length of the mandibular body [10, 11]. The mandibular body, the arch’s shape and width are determined by resorption on the medial surface and deposition on the lateral surface [10]. The mandibular skeletal midline deviates to the affected side with unilateral growth impairment [11].
During the 4th week of embryonic life, distinct face development is identifiable from five facial primordia structures surrounding the stomodeum [12,13,14]; these include one frontonasal prominence and paired maxillary and mandibular processes [15, 16]. The latter two processes originate from the first branchial arch [16, 17]. The innervation to the face arises from the first and second pharyngeal arches, while the blood vessels are derived from the third aortic arch [17]. All these develop to form the structures of the future face [16, 17]. Disruption in the migration and differentiation pathway of the pluripotent neural crest cells results in congenital abnormalities [12, 14].
Facial asymmetry (FA) classification includes congenital, acquired, or developed from an unknown aetiology [18]. HFM is one of the congenital disabilities responsible for facial asymmetry. Asymmetry of the mandibles could involve the ramus, the condyle, the body, and symphysis, which may result in size, volume, or position changes. Skeletal deviation equal to or greater than 4 mm is considered asymmetry noticeable in an individual’s face, while a skeletal deviation less than 4 mm is identified as mild and unnoticeable [19, 20]. In addition to skeletal deformity, soft tissue thickness also influences facial disproportion; hence, a deviation equal to or greater than 2 mm of the soft tissue is marked as facial asymmetry [21, 22].
Some authors hypothesised that mandibular growth defect contributes to FA in HFM patients [23]. Other authors have suggested that mandibular growth defect does not influence FA in HFM patients. The indicators of FA include changes in the maxillary occlusal plane, piriform rim angle, intergonial angle, and chin point deviation [24, 25]. Hence, there are contrasting data on the influence of mandibular growth defects on FA in HFM.
Previous reviews focused on FA, temporomandibular disorders, and mandibular asymmetry. However, only a few discussed the progression of FA due to mandibular disproportion (asymmetry) in HFM patients [23, 26,27,28,29]. The knowledge of skeletal and soft tissue defects is fundamental in the reconstructive approach to facial surgery [30, 31]. This review aims to map out various parameters of the mandible (i.e., the deviation of occlusal plane, piriform angle, intergonial angle, chin point, mandibular ramus height, body length and total mandibular length) in the progression of FA in HFM patients, highlighting its relationship with sex, population, and age group.
Materials and methods
A scoping review based on the framework developed by Arksey and O’Malley [32] and further expanded by Levac et al. [33] was used in this analysis. The literature on the progression of FA due to the mandibular morphology and disproportion (asymmetry) in HFM patients was extensively searched. The following steps were taken in the search process: identifying the research question, identifying relevant studies, study selection, charting the data, and collating, summarising, and reporting the results.
Research question
What were the available studies on the progression of FA due to a deformed mandible in HFM patients?
Sub–question
-
a.
In which countries were these studies completed?
-
b.
What age range or grouping was used to report these studies?
-
c.
To determine facial asymmetry, what parameters were used (i.e., changes in the maxillary occlusal plane, piriform rim angle, intergonial angle, chin point deviation, mandibular ramal height, mandibular body length, total mandibular length)?
Search strategies
A systematic search of the literature was conducted on PubMed (National Centre of Biotechnology Information, Bethesda, Maryland, United States), EBSCOhost (EBSCO Information Services, Ipswich, Massachusetts, USA), and Web of Science (Clarivate Analysis, PLC, Philadelphia, Pennsylvania, USA). The keywords used for this search include hemifacial microsomia, progressive facial asymmetry, mandibular asymmetry, mandibular growth restriction, mandibular hypoplasia, facial asymmetry, and mandibular morphology. These keywords were used in combination with the Boolean term (AND, OR), such as “hemifacial microsomia AND facial asymmetry” OR “hemifacial microsomia AND mandibular growth restriction” OR “hemifacial microsomia AND mandibular growth” OR “hemifacial microsomia AND mandibular hypoplasia” OR “hemifacial microsomia AND mandibular asymmetry” OR “hemifacial microsomia AND mandibular morphology” OR “facial asymmetry AND mandibular morphology” OR “facial asymmetry AND mandibular hypoplasia” OR “hemifacial microsomia AND progressive facial asymmetry” OR “progressive facial asymmetry AND mandibular asymmetry”. An initial limited search of PubMed was completed by analysing the text words in titles, abstracts, and index terms used to describe articles (see Appendix I). A second search using identified keywords and index terms was used across all databases. The third step search was also conducted across all databases using a reference list of all identified articles. The most recent search of this review was accessed on 31st December 2023.
The scoping review results were reported using the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-analysis) guidelines for Scoping review.
Inclusion criteria
The inclusion criteria included studies on the progression of FA in HFM. Original articles on mandibular asymmetry, morphology, and hypoplasia between 1969 and 2022. Articles, reports, and books available in English, articles already translated into English, and articles in dual languages formed part of this review.
Exclusion criteria
Research articles, reviews, and reports on the progression of FA in HFM before 1969 were excluded during study selection (Pruzansky reported the first study on mandibular hypoplasia classification in 1969). Reviews of HFM in progressive FA were excluded. Studies not primarily on the progression of FA in HFM and animal-based HFM studies did not form part of this review.
Study selection
A set of questions aligned with the study’s objective assessed the relevant studies identified during the literature search. Following the search, all identified citations were collated and uploaded into EndNote 20 (Clarivate Analytics, PA, USA), and duplicates were removed. Study selection was made by two authors (PMA, BRO), who screened titles and abstracts of all retrieved studies to assess eligibility. When eligibility could not be determined, full articles were retrieved.
Quality appraisal
The quality appraisal of the included studies was conducted using screening criteria for all studies (Table 1). Quantitative descriptive criteria of the Mixed Methods Appraisal Tool (MMAT)-Version 2018 were used for the included studies [34]. The appraisal was done by colleagues (OA and OF), not part of this review. A score of 20% is given when an eligible study fulfils one quantitative criterion, 40% if it fulfils two criteria, 60% if it fulfils three criteria, 80% if it fulfils four criteria, and 100% if it fulfils all quantitative criteria.
Data extraction and analysis
A data extraction form was used to extract details on characteristics of the included studies by two authors (PMA, BRO), such as author name, date of publication, population, sample size, male (%), female (%), age range, aim of the study, methodology, and significant findings. The extraction form was subjected to review. Co-authors LL and AM independently used this form to extract data from all eligible studies. Microsoft Excel 2019 was used to compile all data on a spreadsheet. The content analysis of each article included in the review was done.
Results
Description of included studies
A total of 3491 articles were identified during the literature search, including research papers, reports, and books. Two thousand four hundred and thirty-two duplicates were removed. After screening titles and abstracts, 1015 articles were excluded based on the exclusion criteria. Forty-four full-text articles that met the eligibility criteria were reviewed. Thirty-three articles were excluded because they lacked evidence on the progression of FA, although they showed evidence of mandibular morphology, morphometrics, asymmetry, and surgical intervention. However, eleven articles were eligible and included in this review (Fig. 1).
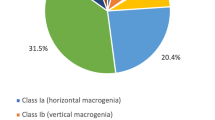
Table 2 summarises the included studies and their significant findings. Table 3 shows the frequency distribution of FA parameters in the included studies. Figure 2 shows the level of knowledge of included studies on the progression of FA in relation to Pruzansky-Kaban type classification, dentition age range and mandibular morphometrics. Figure 3 illustrates an assessment of all the included studies based on the facial asymmetry parameters in hemifacial microsomia patients. Most (55%) of the included studies were conducted in Europe [25, 35,36,37,38,39], 36% were conducted in the United States of America [24, 40,41,42], and 9% were conducted in the People’s Republic of China [43]. The largest sample size is 210 [43], while the lowest is 7 [40].
Number of studies suggesting the progression of facial asymmetry in relation to Pruzansky-Kaban type classification, dentition age range and mandibular morphometrics in the literature from 1969 to date. The X-axis shows the classification, dentition age and measurement of the deformed mandible, and the Y-axis illustrates the number of studies
All included studies were observational; 82% were retrospective studies [24, 25, 36, 37], while 18% were prospective studies [35, 38]. Only three of the included studies (27%) were cross-sectional [24, 39, 43], while the remaining (82%) were longitudinal studies [25, 35,36,37,38,39,40,41,42] (Table 2). A total of 67% of the included studies described sex in their report [25, 36,37,38,39,40,41, 43]. Age grouping varied among the included studies; two (18%) utilised dentition age grouping [24, 39], two (18%) utilised infancy to childhood [41, 43], while others (64%) used varied age grouping [25, 35,36,37,38,39,40, 42]. Three (27%) of the included studies suggested the progression of facial asymmetry [24, 42, 43], while the remaining (73%) suggested that FA remains constant in HFM patients [25, 35,36,37,38,39,40,41].
The methodological quality of the included studies
The eleven included studies were deemed good quality as they answered the first two screening questions and fulfilled at least three quantitative criteria of MMAT. Regarding the quantitative criteria, one study met three criteria- 60% and ten met four criteria- 80% (Table 2).
Table 3 shows the frequency distribution of FA parameters in the eleven included studies. The more common parameters used in the included studies were: 64% used ramus height [35, 36]. 27% used chin point [25, 40, 41], 27% used occlusal plane angle [24, 37, 38], 36% used gonial/intergonial angle [24, 39,40,41], 27% used total mandibular length [39,40,41], 27% used mandibular body length [41,42,43]. In addition, a few of the included studies discussed the treatment approach and outcome (Table 4).
Studies suggesting evidence of progressive facial asymmetry in relation to Pruzansky-Kaban type classification, dentition age range and mandibular morphometrics
Ten (91%) of the included studies utilised either Pruzansky [35, 39,40,41,42] or Pruzansky-Kaban [24, 25, 36, 37, 43] types to classify the mandibular asymmetry in HFM. Two (18%) of the included studies utilised dentition age [24, 39], two (18%) of the included studies utilised infancy to childhood stage [41, 43] for age grouping. The majority (91%) of the included studies showed evidence of knowledge of mandibular morphometry in HFM patients [24, 25, 35,36,37].
Assessment of all the included studies based on their conclusion on the progressiveness of FA in hemifacial microsomia patients
An assessment of mandibular morphometric parameters was used to determine the progressiveness of FA in the HFM population in all (100%) of the included studies [24, 25, 35,36,37,38,39]. An increase in the values of the parameters is associated with progressive FA and was denoted as ‘Yes’ (Fig. 3). These include occlusal plane/angle [24], gonial/intergonial angle [24], piriform angle [24], ramus height [42, 43], mandibular length [42], and body length [42, 43].
A decrease or no change in the parameters’ values is associated with FA’s non-progressiveness and was denoted as ‘No’ (Fig. 3). These include chin point [25, 38, 41], gonial/intergonial angle [39,40,41], ramus height [35, 36, 39,40,41], mandibular length [38, 39, 41] and body length [40].
Some studies did not report on these parameters (Fig. 3). These include chin point [24, 35,36,37, 39, 40, 42, 43], occlusal plane/angle [25, 35,36,37,38,39], gonial/intergonial angle [25, 35,36,37,38, 42, 43], piriform angle [25, 35,36,37,38,39], ramus height [24, 25, 37, 38], mandibular length [24, 25, 35,36,37, 40] and body length [24, 25, 35,36,37,38,39, 41, 43].
Discussion
This review seeks to map out the various parameters of the mandible in the progression of FA in HFM patients, highlighting its relationship with sex, population, and age group. This review suggests that FA in HFM patients remain constant with time (age). All included studies were completed in countries such as the United States of America, China, Sweden, Italy, Finland and the Netherlands. Kearns et al. [24] and Kaprio et al. [39] used dentition age groups, Polley et al. [41] and Zhang et al. [43] utilised infancy to childhood age grouping, while others utilised various age groups in the included studies. FA was evaluated using parameters such as chin point, occlusal plane/angle, gonial/intergonial angle, piriform angle, ramus height, mandibular length, and body length [24, 25, 35,36,37,38,39]. The most reported parameter is ramus height, while the least reported parameter is piriform rim angle [24, 25, 35,36,37,38,39].
The mandible is the most affected facial bone in HFM, with FA reported as either increasing or remaining constant with age in HFM patients [25, 39, 42, 43]. Authors reporting progressive FA advocate for early surgical intervention to minimise end-stage deformity and psychosocial-economic impact, whereas others view FA as non-progressive, recommending surgical intervention at the end of growth due to the need for revisional surgery and increased psychosocial-economic burden [23, 25, 42]. The severity of the deformed mandible can be determined using various classification methods, with the Pruzansky or Pruzansky-Kaban classification being the gold standard for hypoplastic mandible in HFM [8, 44, 45]. Other classifications, such as SAT, OMENS, and OMENS+, were not used in the included studies [6, 9, 46]. Understanding these classifications ensures a proper treatment approach to mandibular lengthening through osteotomy, distraction osteogenesis, and grafting in maxillofacial or plastic surgery and orthodontics [47]. In addition to skeletal correction, structural fat grafts are used to augment soft tissue deformity in HFM patients, although this technique often requires multiple revisions [48]. New visualising techniques, including three-dimensional printed operation templates, offer advanced intervention planning despite challenges in treatment timelines and availability [49]. There are opposing views regarding the growth potential of the mandible in HFM patients. Some clinicians report the affected mandible becomes retarded in growth compared to the unaffected side [50], while others state the affected mandible grows parallel to the unaffected side [51, 52]. Evidence from dentition age groupings suggests an increase in deformity severity with age [24], although some studies, such as Polley and colleagues, indicate that the asymmetric mandible remains constant throughout growth [41]. Overall, while the growth pattern for different HFM severities appears non-progressive, severe HFM cases show otherwise [43]. This is crucial for diagnosing and managing HFM patients [24, 41, 53]. Also, it is noteworthy that rotations can still increase in one axis and decrease in another even when there are no overall growth changes [54]. An inherent genetic factor may cause asymmetry and increased angular measurement in FA [42]. However, some studies report that chin point values remain constant with age [25]. It is recommended that mandibular asymmetry correction in HFM be carried out during the mixed dentition age (6–12 years), though this is not the primary focus of this review [4, 55].
Assessment of HFM can be done either quantitatively or qualitatively [4] to determine the progressiveness of FA. Researchers have used parameters such as chin point, occlusal plane/angle, gonial/intergonial angle, piriform rim angle, ramus height, mandibular body length and total mandibular length to ascertain the extent of FA in HFM patients. Individual assessment of the indicators of FA on either progressive or non-progressive from the included articles in this review favoured the more non-progressive nature of HFM compared to few studies that favoured the progressive nature of the condition. Some authors have hypothesised that early treatment of HFM could promote midfacial growth and facial symmetry [3, 56]. At the same time, a report by Pluijmers et al. [57] does not support the hypothesis of the long-term stability of early treatment in HFM patients.
All the included studies in this review were completed in countries such as the United States of America, China, and various European nations; none were from Africa. Although there is a large body of existing literature on HFM, reports are primarily from international populations, with a few from the African continent [58,59,60,61,62]. It does not translate to Africa being spared of the burden of this congenital anomaly.
Psychological and biological features influence sexual dimorphism. Facial sexual dimorphism becomes more distinct after puberty due to the increased levels of androgen and oestrogen [63]. The shape difference decreases with age as the female mandible becomes like the male mandible while both sexes gain size [64]. Evidence from the included study shows no relationship between FA and gender dimorphism in the HFM population. Correspondingly, Nagy et al. [65] reported a similar distribution between sexes and dismissed the concept of prevalence in male patients and laterality to the right side. There is no sexual dimorphism in both progressive and non-progressive FA from the included studies. Therefore, there is no difference in treatment approach to HFM in both sexes. FA is typically found in humans; this becomes obvious in HFM patients due to the apparent defect to the mandible and associated facial skeleton [36, 42]. Multi-interventional approaches by healthcare providers such as otolaryngologists, audiologists, orthodontics, orthognathic surgeons, plastic surgeons, medical geneticists, and clinical psychologists are needed to manage and treat HFM.
The limitations of this review include the use of heterogenous age grouping, small sample size, less reporting on sex distribution in the sample size, insufficient empirical data on the severe skeletal or soft tissue deviation, the use of orthopantomograms to measure mandibular growth in some of the included studies may not cover the true depth of three-dimensional growth of the mandible and inconsistent use of angular measurement of FA in the included studies do not allow us to explore further facial asymmetry progression in other eligible studies. Furthermore, there is a lack of robust studies in the field of HFM; thus, no definitive conclusions can be drawn regarding the collective characteristics of this anomaly. All the included articles were longitudinal [25, 35, 38, 40, 42], except two [24, 43]. In the study reported by Shetye et al. [42], there is confusion regarding using the terms rate and ratio between the affected and unaffected sides in the HFM. Many of the eligible studies are case series studies [57]. Case series studies are regarded as low levels of evidence-based medicine. Therefore, caution is required to make firm conclusions when interpreting the information from these types of studies [57].
Conclusion
The included studies widely use the Pruzansky or Pruzansky-Kaban classification systems. There is a correlation between progressive FA and dentition-age grouping. The FA parameters used in this review include chin point, gonial/intergonial angle, piriform angle, mandibular ramus height, mandibular length, and body length. An assessment of the included studies on FA parameters favoured more on the non-progressive nature of HFM. American and European populations have reported more on the progression of FA, with fewer reports from the Asian population. Evidence from the included studies indicates that FA does not increase in HFM patients, as demonstrated by the constant ratio of the affected side compared to the non-affected side during growth. The substantial establishment of a significant increase in FA with age in HFM remains uncertain. Hence, we premise that there is no progression of FA in HFM patients. However, the timing of the surgical intervention should be based on the functional or aesthetic needs of the patients. HFM patients with functional requirements such as obstructive sleep apnoea and feeding difficulty due to micrognathia or retrognathia may require interventions before skeletal maturity. The decision to operate on HFM prior to or after skeletal maturity should be individual-specific, considering both functional and psychosocial factors. More data are required from African and Asian populations for scholarly contribution to managing and treating HFM.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- FA:
-
Facial Asymmetry
- HFM:
-
Hemifacial Microsomia
- MMAT:
-
Mixed Method Appraisal Tool
- OMENS (+):
-
Orbit distortion, Mandible hypoplasia, Ear anomaly, Nerve involvement, Soft tissue deficiency, Extracraniofacial defects
- PRISMA:
-
Preferred Reporting Items for Systematic reviews and Meta-analyses
- SAT:
-
Skeletal Auricular Soft tissue
- USA:
-
United States of America
- WHO:
-
World Health Organization
References
Young A, Spinner A (2022) Hemifacial Microsomia. StatPearls Publishing, Treasure Island (FL). https://pubmed.ncbi.nlm.nih.gov/32809654/. Accessed 04 November 2022
Hartsfield J (2007) Review of the etiologic heterogeneity of the oculo-auriculo-vertebral spectrum (Hemifacial Microsomia)*. Orthod Craniofac Res 10:121–128. https://doi.org/10.1111/j.1601-6343.200700391.x
Chen X, Yang X, Gu S et al (2020) Early hemi-mandibular lengthening by distraction osteogenesis contributes to compensatory maxillary growth. J Craniomaxillofac Surg 48:357–364. https://doi.org/10.1016/j.jcms.2020.02.016
Murray JE, Kaban LB, Mulliken JB (1984) Analysis and treatment of hemifacial microsomia. Plast Reconstr Surg 74:186–199. https://doi.org/10.1097/00006534-198408000-00003
Pierpont MEM, Moller JH, Gorlin RJ, Edwards JE (1982) Congenital cardiac, pulmonary, and vascular malformations in oculoauriculovertebral dysplasia. Pediatr Cardiol 2:97–302. https://doi.org/10.1007/BF02426976
David DJ, Mahatumarat C, Cooter RD (1987) Hemifacial microsomia: a multisystem classification. Plast Reconstr Surg 80:525–535. https://doi.org/10.1097/00006534-198710000-00008
Rollnick BR, Kaye CI, Nagatoshi K, Hauck W, Martin AO, Reynolds JF (1987) Oculoauriculovertebral dysplasia and variants: phenotypic characteristics of 294 patients. Am J Med Genet 26:361–375. https://doi.org/10.1002/ajmg.1320260215
Cohen M Jr, Rollnick BR, Kaye CI (1989) Oculoauriculovertebral spectrum: an updated critique. Cleft Palate J 26:276–286
Horgan JE, Padwa BL, Labrie RA, Mulliken JB (1995) OMENS-Plus: analysis of craniofacial and extracraniofacial anomalies in hemifacial microsomia. Cleft Palate Craniofac J 32:405–412. https://doi.org/10.1597/1545-1569_1995_032_0405_opaoca_2.3.co_2
Kaban LB, Mulliken JB, Murray JE (1981) Three-dimensional approach to analysis and treatment of hemifacial microsomia. Cleft Palate J 18:90–99
Springate SD (2019) An investigation of growth rotations of jaws. University College London, London https://discovery.ucl.ac.uk/id/eprint/10071949/Accessed 02 February 2023
Roth DM, Bayona F, Baddam P, Graf D (2021) Craniofacial Development: neural crest in Molecular Embryology. Head Neck Pathol 15:1–15. https://doi.org/10.1007/s12105-021-01301-z
Sperber GH (1989) Craniofacial Embryology. Wright, London
Srinivasan A, Toh YC (2019) Human pluripotent stem cell-derived neural crest cells for tissue regeneration and disease modeling. Front Mol Neurosci 12:39. https://doi.org/10.3389/fnmol.2019.00039
Johnston M (1990) Embryology of the head and neck. In: McCarthy J (ed) Plastic surgery. WB Saunders, Philadelphia PA, pp 2451–2495
Carstens MH (2002) Development of the facial midline. J Craniofac Surg 13:129–187. https://doi.org/10.1097/00001665-200201000-00032
Nguyen JD, Duong H (2023) Anatomy, Head and Neck: Face. [Updated 2023 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK551530/ Accessed 15 July 2023
Cheong YW, Lo LJ (2011) Facial asymmetry: etiology, evaluation, and management. Chang Gung Med J 34:341–351
Silva NCFd A, ÉRBd, Mello KCFR, Mattos JNR, Normando D (2011) Habilidade De Ortodontistas E leigos na percepção de assimetrias da mandíbula. Dent Press J Orthod 16(4):e31–38. https://doi.org/10.1590/s2176-94512011000400007
Lee JK, Jung PK, Moon CH (2014) Three-dimensional cone beam computed tomographic image reorientation using soft tissues as reference for facial asymmetry diagnosis. Angle Orthod 84:38–47. https://doi.org/10.2319/112112-890.1
Ramirez-Yañez GO, Stewart A, Franken E, Campos K (2010) Prevalence of mandibular asymmetries in growing patients. Eur J Orthod 33:236–242. https://doi.org/10.1093/ejo/cjq057
Kim JY, Jung HD, Jung YS, Hwang CJ, Park HS (2014) A simple classification of facial asymmetry by TML system. J Craniomaxillofac Surg 42:313–320. https://doi.org/10.1016/j.jcms.2013.05.019
Kaban LB (2009) Mandibular asymmetry and the fourth dimension. J Craniofac Surg 20(1):622–631. https://doi.org/10.1097/SCS.0b013e318195249c
Kearns GJ, Padwa BL, Mulliken JB, Kaban LB (2000) Progression of facial asymmetry in hemifacial microsomia. Plast Reconstr Surg 105:492–498. https://doi.org/10.1097/00006534-200002000-00002
Renkema RW, van Beelen I, Koudstaal MJ, Caron CJJM (2022) The effect of natural growth on chin point deviation in patients with unilateral craniofacial microsomia: a retrospective study. J Craniofac Surg 50:615–620. https://doi.org/10.1016/j.jcms.2022.07.006
Akhil G, Senthil Kumar KP, Raja S, Janardhanan K (2015) Three-dimensional assessment of facial asymmetry: a systematic review. J Pharm Bioallied Sci 7:S433–437. https://doi.org/10.4103/0975-7406.163491
Thiesen G, Gribel BF, Freitas MP (2015) Facial asymmetry: a current review. Dent Press J Orthod 20:110–125. https://doi.org/10.1590/2177-6709.20.6.110-125.sar
Marques FBC, de Lima LS, Oliveira PLE et al (2021) Are temporomandibular disorders associated with facial asymmetry? A systematic review and meta-analysis. Orthod Craniofac Res 24:1–16. https://doi.org/10.1111/ocr.12404
Babczyńska A, Kawala B, Sarul M (2022) Genetic factors that affect asymmetric mandibular growth - A systematic review. Symmetry 14(3):490. https://doi.org/10.3390/sym14030490
Kawamoto HK (1976) The kaleidoscopic world of rare craniofacial clefts: order out of chaos (Tessier classification). Clin Plast Surg 3:529–572
Omodan A, Pillay P, Lazarus L, Madaree A, Satyapal K (2019) Scoping review of the morphology and anthropometry of Tessier craniofacial clefts numbers 3 and 4. Syst Rev 8:1–12. https://doi.org/10.1186/s13643-019-0951-6
Arksey H, O’Malley L (2005) Scoping studies: towards a methodological framework. Int J Soc Res Method 8(1):19–32. https://doi.org/10.1080/1364557032000119616
Levac D, Colquhoun H, O’Brien KK (2010) Scoping studies: advancing the methodology. Implement Sci 5:69. https://doi.org/10.1186/1748-5908-5-69
Hong QN, Fàbregues S, Bartlett G et al (2018) The mixed methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inf 34:285–291. https://doi.org/10.3233/EFI-180221
Meazzini MC, Mazzoleni F, Bozzetti A, Brusati R (2012) Comparison of mandibular vertical growth in hemifacial microsomia patients treated with early distraction or not treated: follow up till the completion of growth. J Craniomaxillofac Surg 40:105–111. https://doi.org/10.1016/j.jcms.2011.03.004
Ongkosuwito EM, van Neck JW, Wattel E, van Adrichem LN, Kuijpers-Jagtman AM (2013) Craniofacial morphology in unilateral hemifacial microsomia. Br J Oral Maxillofac Surg 51:902–907. https://doi.org/10.1016/j.bjoms.2012.10.011
Ongkosuwito EM, van Vooren J, van Neck JW et al (2013) Changes of mandibular ramal height, during growth in unilateral hemifacial microsomia patients and unaffected controls. J Craniomaxillofac Surg 41:92–97. https://doi.org/10.1016/j.jcms.2012.05.006
Rune B, Selvik G, Sarnäs KV, Jacobsson S (1981) Growth in hemifacial microsomia studied with the aid of roentgen stereophotogrammetry and metallic implants. Cleft Palate J 18:128–146
Kaprio L, Grann A, Leikola J, Saarikko A, Kurimo J, Kiukkonen A (2023) Nonprogressive mandibular changes in children with type I and II craniofacial microsomia. Orthod Craniofac Res 00:1–9. https://doi.org/10.1111/ocr.12719
Kusnoto B, Figueroa AA, Polley JW (1999) A longitudinal three-dimensional evaluation of the growth pattern in hemifpoacial microsomia treated by mandibular distraction osteogenesis: a preliminary report. J Craniofac Surg 10:480–486. https://doi.org/10.1097/00001665-199911000-00006
Polley JW, Figueroa AA, Liou EJ-W, Cohen M (1997) Longitudinal analysis of Mandibular Asymmetry in Hemifacial Microsomia. Plast Reconstr Surg 99(2):328–339. https://doi.org/10.1097/00006534-199702000-00005
Shetye PR, Grayson BH, McCarthy JG (2023) Longitudinal Skeletal Growth Analysis of Mandibular Asymmetry in Unoperated patients with unilateral Craniofacial Microsomia (UCFM). Cleft Palate Craniofac J 60:69–74. https://doi.org/10.1177/10556656211054002
Zhang Z, Chen X, Kim BS et al (2023) Quantitative structural analysis of hemifacial microsomia mandibles in different age groups. Front Pediatr 11:1157607. https://doi.org/10.3389/fped.2023.1157607
Pruzansky S (1969) Not all dwarfed mandibles are alike. Birth Defects 5:120–129
Kaban LB, Moses MH, Mulliken JB (1988) Surgical correction of hemifacial microsomia in the growing child. Plast Reconstr Surg 82:9–19
Vento AR, LaBrie RA, Mulliken JB (1991) The O.M.E.N.S. classification of hemifacial microsomia. Cleft Palate Craniofac J 28:68–76 discussion 77. https://doi.org/10.1597/1545-1569_1991_028_0068_tomens_2.3.co_2
Srivastava D, Singh H, Mishra S, Sharma P, Kapoor P, Chandra L (2018) Facial asymmetry revisited: part II-Conceptualising the management. J Oral Biol Craniofac Res 8:15–19. https://doi.org/10.1016/j.jobcr.2017.09.008
Rajan S, Ajayakumar K, Sasidharanpillai S, George B (2019) Autologous Fat Graft for Soft tissue camouflage in Craniofacial Microsomia. J Cutan Aesthet Surg 12:223–226. https://doi.org/10.4103/jcas.Jcas_99_18
Paul MA, Opyrchał J, Knakiewicz M, Jaremków P, Bajtek J, Chrapusta A (2020) Hemifacial Microsomia Review: recent advancements in understanding the Disease. J Craniofac Surg 31:2123–2127. https://doi.org/10.1097/scs.0000000000006616
Padwa BL, Mulliken JB, Maghen A, Kaban LB (1998) Midfacial growth after costochondral graft construction of the mandibular ramus in hemifacial microsomia. J Oral Maxillofac Surg 56:122–127. https://doi.org/10.1016/s0278-2391(98)90847-3. discussion 127–128
Meazzini MC, Mazzoleni F, Canzi G, Bozzetti A (2005) Mandibular distraction osteogenesis in hemifacial microsomia: long-term follow-up. J Craniomaxillofac Surg 33:370–376. https://doi.org/10.1016/j.jcms.2005.07.004
Kim BC, Bertin H, Kim HJ et al (2018) Structural comparison of hemifacial microsomia mandible in different age groups by three-dimensional skeletal unit analysis. J Craniomaxillofac Surg 46:1875–1882. https://doi.org/10.1016/j.jcms.2018.08.009
Liu W, Xu X, Zhao S et al (2022) Mandibular distraction Osteogenesis First for children with severe unilateral Hemifacial Microsomia: treatment strategy and outcomes. J Craniofac Surg 33(2):485–490. https://doi.org/10.1097/SCS.0000000000008252
Rune B, Sarnäs K-V, Selvik G, Jacobsson S (1983) Roentgen stereometry with the aid of metallic implants in hemifacial microsomia. Am J Orthod 84:231–247. https://doi.org/10.1016/0002-9416(83)90131-8
Lu TC, Kang GC, Yao CF et al (2016) Simultaneous maxillo-mandibular distraction in early adolescence as a single treatment modality for durable correction of type II unilateral hemifacial microsomia: follow-up till completion of growth. J Craniomaxillofac Surg 44:1201–1208. https://doi.org/10.1016/j.jcms.2016.07.002
Qiu X, Sun H, Zhu M et al (2021) Using orthodontic elastic traction during the active period of distraction osteogenesis to increase the effective vertical extension of hemifacial microsomia patients: a multi-center randomised clinical trial. J Craniomaxillofac Surg 49:1054–1063. https://doi.org/10.1016/j.jcms.2021.06.013
Pluijmers B (2019) On Craniofacial Microsomia shape and surgery [Ph.D. thesis]: Erasmus University, Rotterdam https://repub.eur.nl/pub/119281
Allam KA (2021) Hemifacial microsomia: clinical features and associated anomalies. J Craniofac Surg 32:1483–1486. https://doi.org/10.1097/SCS.0000000000007408
Werler MM, Sheehan JE, Hayes C, Padwa BL, Mitchell AA, Mulliken JB (2004) Demographic and Reproductive Factors Associated with Hemifacial Microsomia. Cleft Palate Craniofac J 41:494–500. https://doi.org/10.1597/03-110.1
Preston CB, Losken HW, Evans WG (1985) Restitution of facial form in a patient with Hemifacial Microsomia: a case report. Angle Orthod 55:197–205. https://doi.org/10.1043/0003-3219(1985)055<0197:Roffia>2.0.Co;2
Losken HW, Preston CB, Evans WG (1983) Hemifacial microsomia. A case report. S Afr Med J 64(13):500–502
Taiwo A (2020) Classification and management of hemifacial microsomia: a literature review. Ann Ib Postgrad Med 18:S9–S15
Kleisner K, Tureček P, Roberts SC et al (2021) How and why patterns of sexual dimorphism in human faces vary across the world. Sci Rep 11(1):5978. https://doi.org/10.1038/s41598-021-85402-3
Glowacki J, Christoph K (2013) Gender differences in the growing, abnormal, and aging jaw. Dent Clin North Am 57:263–280. https://doi.org/10.1016/j.cden.2013.01.005
Nagy K, Kuijpers-Jagtman AM, Mommaerts MY (2009) No evidence for long-term effectiveness of early osteodistraction in Hemifacial Microsomia ‘Outcomes article’. Plast Reconstr Surg 124:2061–2071. https://doi.org/10.1097/PRS.0b013e3181bcf2a4
Acknowledgements
Thanks to Okikioluwa Aladeyelu (SL) and Oyesanmi Fabunmi (OF) of the School of Laboratory Medicine and Medical Sciences, University of KwaZulu-Natal, for participating in the appraisal of eligible studies. Nonkuthalo Ngcakaza-Mchunu, Medical School Library, University of KwaZulu-Natal, for providing resources to help us set up and conduct this research study.
Funding
This study received no specific funding.
Open access funding provided by University of KwaZulu-Natal.
Author information
Authors and Affiliations
Contributions
PMA and BRO conceptualisation; PMA & BRO collected and data analysis; PMA wrote the manuscript first draft; PMA, BRO, AM, & LL wrote and edited manuscript; A.M. and LL supervision. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This paper is a systematic scoping study that relies strictly on reviewing existing literature. Ethical approval is not required since no animal or human participants were in this study.
Competing interests
The authors declare no competing interests.
Additional information
Correspondence and requests for materials should be addressed to LL.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix I: search strategy
Appendix I: search strategy
MEDLINE via PubMed on 15th July 2022
PubMed 15/07/2022 = 625.
(((((((((“hemifacial microsomia” AND “facial asymmetry”) OR (“hemifacial microsomia” AND “mandibular growth restriction”)) OR (“hemifacial microsomia” AND “mandibular growth”)) OR (“hemifacial microsomia” AND “mandibular hypoplasia”)) OR (“hemifacial microsomia” AND “mandibular asymmetry”)) OR (“hemifacial microsomia” AND “mandibular morphology”)) OR (“facial asymmetry” AND “mandibular morphology”)) OR (“facial asymmetry” AND “mandibular hypoplasia”)) OR (hemifacial microsomia AND progressive facial asymmetry)) OR (progressive facial asymmetry AND mandibular asymmetry) NOT (review[pt])))))))))
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Atiba, P.M., Omotoso, B.R., Madaree, A. et al. Hemifacial microsomia: a scoping review on progressive facial asymmetry due to mandibular deformity. Oral Maxillofac Surg (2024). https://doi.org/10.1007/s10006-024-01276-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10006-024-01276-5