Abstract
Purpose
In the presence of infection, acidic pH of a lignocaine local anesthetic causes undesirable effects such as burning on injection, relatively slow onset, and lack of numbness. Buffered lignocaine will increase the pH of the solution and may resolve above problems. Thus, the objective of this study is to compare the efficacy of buffered lignocaine with that of commercial lignocaine.
Method
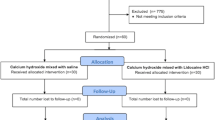
Seventy patients with infected teeth were randomly divided into two equal groups. The study group received buffered lignocaine (8.4% sodium bicarbonate added to 2% lignocaine mixture) while the control received commercial lignocaine preparation (2% lignocaine with 1:80,000 adrenaline). Burning while injection, pain using VAS scale and onset of action with EPT (electric pulp tester) were recorded.
Results
In the study group, the VAS score after injection was 1.20 ± 0.68 and the control group was 2.57 ± 0.92 (p = 0.001). There was a statistically significant reduction in pain reduction in the study group. The time of onset was 3.97 ± 0.71 and 5.67 ± 1.15 min, respectively, and the difference was statically significant. Only one-third of the study group experienced burning on injection as compared to two-thirds in the control group.
Conclusion
Buffered lignocaine is more effective as compared to commercial lignocaine in the extraction of infected teeth.
CTRI number
CTRI/2022/01/039476.
Similar content being viewed by others
Data Availability
The data that support the findings of this study are available on request from the corresponding author.
References
Rood JP (1977) The use of buffered lignocaine solution in the presence of acute inflammation. J Dent 5(2):128–130
Pandey P, Nandkeoliar T, Tikku AP, Singh D, Singh MK (2021) Prevalence of dental caries in the Indian population: a systematic review and meta-analysis. J Int Soc Prev Community Dent 11(3):256–265. https://doi.org/10.4103/jispcd.JISPCD_42_21
Sarvela PJ, Paloheimo PJ, Nikki PH (1994) Comparison of pH-adjusted bupivacaine 0.75% and a mixture of bupivacaine 0.75% and lidocaine 2%, both with hyaluronidase in day-case cataract surgery under regional anesthesia. Anesth Analg 79:35–9
Stanley Malamed (2020) Handbook of local anesthesia, 7th edn. Elsevier, India, p 15
Malamed SF (2004) Handbook of local anesthesia, 5th edn. Elsevier, India, CV Mosby, St.Louis, p 36–37
Larson PO, Ragi G, Swandby M, Darcey B, Polzin G, Carey P (1991) Stability of buffered lidocaine and epinephrine used for local anesthesia. J Dermatol Surg Oncol 17:411–414
Fitton AR, Ragbir M, Milling MA (1996) The use of pH adjusted lignocaine in controlling operative pain in the day surgery unit: a prospective, randomised trial. Br J Plast Surg 49(6):404–408. https://doi.org/10.1016/s0007-1226(96)90011-9
Christoph RA, Buchanan L, Begalla K, Schwartz S (1988) Pain reduction in local anesthetic administration through pH buffering. Ann Emerg Med 17:117–120
Vent A, Surber C, Johansen G, Tracy N, Figueiredo V, Schönbächler G, Imhof L, Buset C, Hafner J (2020) Buffered lidocaine 1%/epinephrine 1:100,000 with sodium bicarbonate (sodium hydrogen carbonate) in a 3:1 ratio is less painful than a 9:1 ratio: a double-blind, randomized, placebo-controlled, crossover trial. J Am Acad Dermatol 83(1):159–165
Arora G, Degala S, Dasukil S (2019) Efficacy of buffered local anaesthetics in head and neck infections. Br J Oral Maxillofac Surg. https://doi.org/10.1016/j.bjoms.2019.06.021
Gupta S, Kumar A, Sharma AK, Purohit J, Narula JS (2018) “Sodium bicarbonate”: an adjunct to painless palatal anesthesia. Oral Maxillofac Surg 22(4):451–455. https://doi.org/10.1007/s10006-018-0730-x
Condouris GA, Shakalis A (1964) Potentiation of the nerve depressant effect of local anaesthetics by carbon dioxide. Nature 204:57–58
Bromage PR, Burfoot MF, Crowell DE et al (1967) Quality of epidural blockade iii: carbonated local anaesthetic solutions. BrJ Anaesthesia 39:197–209
Kashyap VM, Desai R, Reddy PB, Menon S (2011) Effect of alkalinisation of lignocaine for intraoral nerve block on pain during injection, and speed of onset of anaesthesia. Br J Oral Maxillofac Surg 49(8):e72–e75. https://doi.org/10.1016/j.bjoms.2011.04.068
Brandis K (2011) Alkalinisation of local anaesthetic solutions. Aust Prescr 34:173–175
Ritchie JM, Ritchie B, Greengard P (1965) The effect of the nerve sheath on the action of local anesthetics. J Pharmacol Exp Ther 150(1):160–164
Malamed SF (2004) Neurophysiology. In: Malamed SF (ed) Handbook of local anesthesia, 5th edn. Elsevier, India, pp 24–25
Phero JA, Nelson B, Davis B, Dunlop N, Phillips C, Reside G, Tikunov AP, White RP Jr (2017) Buffered versus non-buffered lidocaine with epinephrine for mandibular nerve block: clinical outcomes. J Oral Maxillofac Surg 75(4):688–693. https://doi.org/10.1016/j.joms.2016.09.055
Funding
Self-funded.
Author information
Authors and Affiliations
Contributions
All authors whose names appear on the submission made substantial contributions to the planning of study, interpretation of data, and conclusion of the study. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethical approval
Institutional ethical clearance obtained and informed consent was obtained by percipients to participate in the study.
Competing interests
The authors have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tole, N., Neeli, A. Evaluation of the efficacy of buffered local anesthetic in extraction of infected teeth—randomized double-blind study. Oral Maxillofac Surg (2024). https://doi.org/10.1007/s10006-024-01206-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10006-024-01206-5