Abstract
Introduction
Assaults inflicting penetrating head and neck trauma have potential for serious morbidity or mortality. This paper studies in-depth all cases treated at a level one trauma centre in the North East of England over 10 years.
Methods
All patients assaulted with sharp implements to the head and neck treated from 2010 to 2019 were identified using clinical codes.
Results
Retrospective data collection were as follows: 214 patients identified (189 male, 25 female). Average age was 31.5 years (range 3–80). The majority presented between 20:00 and 05:00. Knives were the commonest weapon. Fifty-two had scalp, 137 face and 69 neck injuries. Forty-eight percent had additional non-head and neck injuries. Eighty-six percent required admission, 16.6% to intensive care. Oral and maxillofacial and plastic surgeons provided most treatment. One hundred two required treatment under general and 96 local anaesthetic. Sixteen patients had significant vascular injury, 1 brachial plexus injury, 4 facial nerve injuries (of which 3 repaired) and one required parotid duct repair. Mean length of stay was 3.7 days. No mortality was recorded. Incidence significantly increased from 2010 to 2019.
Conclusions
Head and neck penetrating injuries occur frequently, often with other injuries and mainly in young males. Incidence of significant vascular or nerve injury was low. This study provides important data for those planning trauma services.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Penetrating injuries are common in the UK comprising 12.9% of Accident and Emergency (A&E) trauma workload [1]. Causes include inter-personal violence, deliberate self-harm (DSH), accidents and terrorism and include injury with any sharp implement or firearms. Incidence is increasing in the UK. The Office of National Statistics knife crime data for England and Wales reported a 43% increase from 2011 to 2018–2019 [2]. However, the UK incidence remains significantly lower than countries such as the USA [3] and South Africa [4].
Head and neck (H&N) penetrating injuries constitute from 3.3 [5] to 8% [1] of total penetrating injuries in the UK and are similarly increasing [6]. These can be shocking to both patients and clinical teams and carry a substantial cost and resource burden to manage [1].
A handful of UK case series specific to penetrating H&N injuries have been published in the past decade. Three originated from London [6,7,8] and one from Liverpool [9], with study periods of 12 months to 6 years and patient cohorts of 25–65. Three considered penetrating neck injury (PNI) only [6, 8, 9].
Given that knife crime is increasing, the existence of robust comprehensive clinical data on penetrating injuries is important to assess the health implications and plan resources accordingly. Prior studies have involved relatively small cohorts over shorter periods and been mainly London-based. This study was designed to overcome these limitations through an in-depth long duration study of all penetrating H&N injuries in a peripheral UK region. Our unit, the Royal Victoria Infirmary in Newcastle upon Tyne, is a level one trauma centre, one of two serving northern England from the Scottish border to Yorkshire—a geographically very large and diverse area including several large conurbations with higher deprivation scores than the UK average [10].
This study is purposefully limited to injuries occurring via assault in order to investigate this specific cohort in detail. Cases were defined as assault if this was indicated in the patient history. No attempt was made to correlate with crime figures or other means as such data are not accessible. Although very similar injuries will be sustained via self-inflicted injuries and accidents, e.g. fan belts, propellers, power tools or falls onto sharp objects, it is specifically the epidemiology of assault that was sought. Studying this group in detail is important as crime-related trauma is a significant societal problem in most countries and robust data are required to strategise effective ways to address it.
The aims of this study are to gather detailed information on the following:
-
Demographics and injury timing
-
Change in incidence
-
Characteristics of injury, investigations, management and other resource use
-
Mortality
Materials and methods
A retrospective review was conducted using our trust’s electronic coding records to create a list of all patients presenting to A&E with H&N penetrating injuries between 1 January 2010 and 31 December 2019. Hospital codes currently used in the UK are derived from the International Classification of Diseases 10th Edition (ICD-10) [11]. Clinical coders in our institution undertook searches of the patient database using several relevant codes, e.g. “assault by sharp object”, stratified the search for head and neck location and removed duplicates. Inclusion criteria is any injury to the H&N region sustained by assault with any sharp instrument within this time period. There are no age limits. Exclusion criteria are non-assaults including from falls and accidents and firearms injuries.
Data were collected from electronic and paper patient records on variables as detailed in the results. The occurrence of the injury via assault was confirmed via records of the patient history given—histories given were taken at face value.
Results
Two hundred fourteen patients met the inclusion criteria.
Gender/age
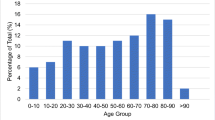
There were 189 male and 25 female. Average age is 31.5 with the range of 3–80 years (a child at nursery receiving a scissor cut to an ear by another child). Graph 1 shows age distribution by gender.
Postcode
Cases originated from throughout the served region but with a clear concentration closer to the centre of Newcastle upon Tyne. Figure 1 maps cases by postcode. Three city postcodes collectively contributed 28% of cases (60/214). The maximum number from a postcode outside Tyneside was 6. Four originated from prisons in postcode areas DH1 and NE65. Twenty-two were from outside the area.
Time/date of attendance
Most patients presented from 21:00 to 05:00 (see Graph 2), peaking from 4 to 5 am. Attendances during daytime hours were consistently much lower besides a peak of ten cases from 11 am to noon. Twenty-seven outside referrals or with no arrival time documented were excluded from these figures.
Caseload was fairly even through the year with small peaks in June and December, range 13 (October) to 23 (June). The highest month’s total was six in April 2015. Only 2017 and 2019 had cases every month.
Weapon
The commonest weapon was a knife in 86 cases. Other weapons comprised of the following: unknown 58, glass 40, machete 12, axe 6, razor blade 2, screwdriver 2, scissors 2, sword 2, pen 1, saw 1, fork 1 and stiletto shoe 1. There were no incidents recorded in this period involving other implements, e.g. chainsaw, nail gun, power tools.
H&N injuries
Sites of injury were categorised as scalp, face and neck. Fifty-two had scalp injury, 137 the face and 69 the neck. Combinations were common—scalp and face 18, face and neck 12, scalp and neck 5 and all three sites 4. Of those with facial injury, more specific sites were comprised of the following—cheek 33, ear 24, nose 19, lip 16 and eyelid 5.
Other H&N injuries comprised of the following: cervical vertebral fractures 2 (C1 and C6), penetrating globe injuries 3, skull base or calvarial fractures 5 and subarachnoid haemorrhage 1. One required lateral canthotomy in A&E for acute orbital compartment syndrome. Three patients received concomitant chemical burns which believed to be from ammonia (one also burned by boiling water thrown into the face) and one inhalation burns from alleged arson of their house.
Non-H&N injuries
One hundred two (48%) had penetrating injuries elsewhere—upper limb 53, lower limb 24, chest 30 (including pneumothorax 1, haemothorax 1, haemopneumothorax 7 and haemopericardium 3), abdomen 15, chest and abdomen 3 and buttock 2.
Imaging and findings
Seventy-six (36%) had CT or CT angiography (CTA) (including 53 of 69 PNI patients). Time to scan was 5—708 min with mean of 68 min. Some were performed at least partially for other reasons, e.g. bony trauma.
Very few CTAs showed significant vessel injury—specific arterial bleed 2 (one facial artery and one posterior neck vessel) and specific venous bleed 5 (including one “branch of IJV”, one anterior jugular vein and one IJV transection). Two further scans showed extravasation with no source identifiable, 11 haematoma, 11 tissue emphysema, 5 skull base or calvarial fractures and 5 facial fractures.
Patient management and admission
The breakdown of patient trajectory is as follows:
-
Self-discharged from A&E 7
-
Treated in A&E then discharged 21, of which treated with
-
LA (all by oral and maxillofacial surgery (OMFS)) 20
-
Simple dressing 1
-
-
Admitted directly from A&E 182, of which treated with
-
Simple dressing 3
-
LA in A&E 30
-
LA on ward or intensive care (ITU) 6
-
LA in theatre 16
-
LA in unspecified location 20
-
GA 102 (20 as joint cases with treatment for non H&N injuries)
-
Unknown inpatient treatment 5
-
-
Discharged from A&E with planned readmission for treatment under LA the next day (all by plastics) 4
Overall H&N injuries were managed by simple dressing in 4, LA in 96, GA in 102 cases and indeterminate in 5 cases.
Admitting specialty
OMFS took 32%, plastics 29%, A&E 16% and ENT 4% of admissions. Nine percent was admitted by either General Surgery, Orthopaedics, Cardiothoracics or Neurosurgery, with Ophthalmology, Critical Care, Burns and Vascular Surgery also managing a handful of cases and six under joint care.
All PNI cases were managed by OMFS except plastics input sought for one with a brachial plexus injury, and 8 managed by ear, nose and throat (ENT). Otherwise, no clear pattern was evident for referral to OMFS or plastics except the latter being favoured when limb injuries co-existed.
Level of care
Sixteen of 182 (8.8%) immediate admissions were to ITU (details in Table 1). Ten had PNI of which 5 had significant other injuries. Six went to ITU purely for non-H&N injuries. All required emergency surgery and six red cell transfusions.
Transfusions
Thirteen patients received blood transfusions (details in Table 1), in eight cases largely or entirely due to non-H&N injuries. One received a pre-hospital transfusion and the others in-hospital transfusions of one to four units of red cells.
Time to theatre
This was measured from arrival at A&E. For GA cases, mean time was 13.7 h with a range of 1–55 h. Six cases were less than 90 min—all involved PNI. For LA cases in theatre, mean time was 16.8 h with a range of 1–71 h.
Operative findings
Scalp injuries
Of the 52 patients, no specific neurovascular or bony injuries were recorded except a fragment of frontal outer table in one wound and an unspecified arterial bleed, easily controlled, in another.
Facial injuries
Of the 137 patients, the vast majority had superficial injuries with no specific structural injury.
Seven had significant vascular injuries. One patient with a knife lodged immediately adjacent to the internal carotid artery required carotid balloon cannulation although the arterial wall was later intact. Four had injured superficial temporal artery, one maxillary artery, one facial vessels and one an unspecified artery. Two patients had primary facial nerve repair (one buccal branch and one unspecified location), and one had a temporal branch injury too distal for repair. One further patient had buccal branch weakness post-op when no injury was noted at operation. One required parotid duct repair (one further patient had an intact duct on cannulation but developed a sialocele post-op). Two patients had tissue loss to the nasal tip and one glass foreign bodies.
Neck injuries
Of the 69 PNI cases, sternocleidomastoid was incised in five, trapezius in one and submandibular gland in three (one required excision)—one through and through to the valleculae. One patient had an enlarged lymph node biopsied, later reported as a traumatised node. One patient required temporary tracheostomy due to swelling around the airway.
Major vessels were cut in nine cases—one with common and internal carotid artery transections (treated with patch repair by the vascular surgeons), three with injured internal jugular veins (all tied off), four with facial vessels cut, two external jugular veins and one anterior jugular vein. Four other cases had injured smaller tributary vessels in the neck.
Three cases of nerve injury in the neck were noted—one great auricular nerve, one marginal mandibular (which was repaired) and one brachial plexus injury (primarily repaired). Combined with the facial injuries, this gives a total of four patients having facial nerve injury noted at operation (of which three were repaired).
Details of cases with significant structural injuries in the face or neck are in Table 2.
Length of stay
Mean hospital stay 3.7 days. Two patients were outliers at 34 and 33 days. These were a 61-year-old male stabbed to the right face and neck sustaining open scapula fracture, C1 fracture and hemiparesis and requiring complex multi-disciplinary input and a 42-year-old stabbed to the mouth, chest and shoulder respectively. The next longest stay was 17 days. Forty-five patients were admitted for less than 24 h. Two patients were self-discharged after admission.
Mean ITU stay was 3.7 days (range 1–10 days).
Mortality
No mortality was recorded.
Change in incidence
The mean annual caseload was 21.4 with a range of 11–33 (peaking in 2017) as shown in Graph 3. Simple linear regression analysis confirms a statistically significant increase in incidence from 2010 to 2019 (p = 0.0228) (GraphPad Software, San Diego, CA, USA).
Discussion
Compared to the data from London and Liverpool, the caseload in our unit appears lower. The numbers treated here are also well below those seen in some centres internationally. For example, a study in a trauma centre in Pietermaritzburg, South Africa, recorded 462 neck stab wounds in 46 months, with a mortality of 2% [12]. An analysis of 13 years’ data from a trauma centre in Los Angeles, USA, recorded 606 PNIs [13]. Another study in Mexico City recorded 123 stab wounds to the neck in a 3-year period [14]. This compares to 69 cases in 10 years in our study. All of these data originate within the last 10–15 years.
The main city we serve, Newcastle upon Tyne, has a population of 300,000, about half that of Pietermaritzburg, yet the figures above are very disparate. It is likely that a number of factors produce this difference. Our region has greater deprivation relative to the UK as whole, although this does not equate to the levels of deprivation seen in many areas worldwide, including large cities in many developed countries. Some of this correlation is related to gang violence, a significant cause of these injuries in teenagers in London [15]. It is known that the existence and activity of comparable gangs in the North East of England are far less than in London, which is reflected in the much lower caseload seen among these age groups at our institution. Correlation between levels of deprivation, gang activity, violence and arrest have been demonstrated internationally [16, 17]. Other wider societal factors are also influential, as clearly illustrated by the significant reduction in penetrating weapon assaults noted in South Africa during lockdowns due to the COVID-19 pandemic [18].
The mechanism of penetrating head and neck injuries varies internationally. For example, arrow head injuries are reportedly common in rural Nigeria [19], but extremely rare in the UK. Many other implements have been reported worldwide including pencils, chopstick, machine bolt, spear gun, chain saw, comb, wooden sticks and Taser barbs. The majority of our injuries recorded were inflicted by knives, with broken glass also common. It is likely that many of the latter cases were associated with violence following alcohol consumption in bars or elsewhere. Studies from comparable centres worldwide have also reported high numbers of knife stabbings to the head and neck [12, 13]. However, large series in the USA and South Africa also recorded large numbers of gunshot wounds—463 in 13 years [13] and 58 in 46 months respectively [12]. Although gunshot wounds were not measured in our study, such injuries are very rare in our region. This is likely due to the very tight regulations on gun ownership in the UK, which means that the number of firearms in circulation is much lower than some other countries, e.g. the USA. Therefore, knives, which are much more readily available, are the predominant weapon. Knife crime and violence inflicted with knives continue to increase in the UK to 2021 [20], a trend reflected in our regional data.
Other studies concur that young males are most likely to sustain these injuries [1, 5,6,7, 9, 21], most often from knives [1, 6, 9]. Peak occurrence from late evening to early morning is noted elsewhere (particularly Friday, Saturday and Sunday) [1], with earlier peaks for younger patients [21]. Annual patterns vary, with peaks noted in summer [1] and winter [9]. There may be variations in factors between regions and different years.
Previous studies focused on PNIs. This study has shown that facial injuries are significantly commoner, with scalp injuries also common. A subset with other H&N injuries like fractures, intra-cranial haemorrhage and burns is clearly demonstrated. The two cervical spine fractures here (both from PNI) were very unusual as they are rare in PNI [13]. Forty-eight percent had concurrent non-H&N penetrating injuries here and 50% elsewhere [5], in many cases taking precedence over H&N injuries. Clinicians managing trauma cases need to be alert to all of these possibilities.
No attempt was made to categorise PNIs by zone, given recent evidence favouring immediate surgery for unstable patients and CTA investigation of stable patients regardless of anatomical zone [14,15,−16]. Six of 69 PNI patients underwent immediate surgery—3 on clinical grounds without imaging. One had common and internal carotid transections, one external carotid and maxillary artery and retromandibular vein transections and one brachial plexus injury. Of the 3 imaged patients, no definite vascular injury was seen, although one had an unspecified arterial bleed and retromandibular vein injury at operation. Fifty-three PNI patients in total underwent CTA, higher than other studies [9], and 25 had surgical exploration despite negative scans. All would be classed as “negative explorations” as no vascular injuries were found operatively, which could be considered excessive according to guidelines recommending non-operative management for such cases [16.] Other studies have also reported high rates of these negative explorations [9]. These recent guidelines advocate a move away from a “zonal” assessment of PNI and to base decisions on requirement for emergency surgery on haemodynamic stability and the presence/absence of so-called hard signs of injury of vital structures. These hard signs include expanding haematoma, airway compromise, difficulty swallowing and others. The recommendation is patients lacking any hard signs and who are haemodynamically stable do not require emergency surgery, and should be further evaluated with CTA. Nine of our 69 PNI cases in total had major vessel injury. Other studies report reasonably similar numbers although with varying patient cohorts—3 (possibly 5) of 63 [9], 5 of 31 (although some may have been firearms injuries) [6] and 6 of 25 cases [8]. One pharyngo-oesophageal but no laryngo-tracheal injuries occurred, despite occurring in 12.5% of PNIs elsewhere [9]. Incidence of facial nerve and parotid duct injury here was low.
One hundred two of 207 (49%) treated patients had a GA. This appears high compared to other studies, e.g. 26 [6] to 35% [9] of PNI patients, although 65% was reported for penetrating injuries overall [1]. Notably, the OMFS team treated many wounds under LA in A&E, a trend not replicated by other specialties. A high proportion (86%) of patients were admitted directly from A&E, other studies reporting 25.7 [5] to 70% [7]. An 8.8% of our patients being admitted to ITU is significantly lower than the 32% reported elsewhere [1].
It was interesting to see the differing admitting specialities for similar injuries, predominantly either OMFS or Plastics. From our study, there was no clear reason for this, other than the presence of concurrent limb injuries where plastics was the speciality of choice. This likely partly relates to a lack of awareness of the role of OMFS as a speciality—a UK study found that 72.3% of undergraduate medical students received no exposure to the speciality at university [22]. In the authors’ own experience, A + E doctors unfamiliar with the service often refer facial/neck injuries to plastics unless directed otherwise. Steps are being made to improve awareness of the speciality both within a hospital setting and medical school, and so with time, this situation may change. It would be interesting to see if similar referral patterns are seen in other hospitals both on a domestic UK level and internationally—this is an area requiring further research.
The strengths of this study are it being the longest duration and most in-depth study specific to H&N penetrating injury in the UK to date. Limitations include the reliance on clinical codes to identify cases, which can be rather imprecise and are reliant on cases being coded correctly. However, the converse of this imprecision is that they are broad enough in definition to make it likely very few relevant cases were missed by the search. Quality of extracted data was dependent on quality of medical records. It provides a comprehensive data set available for future comparison and likely to be useful to trauma service planners. It was not possible to measure either financial cost in the short or long term, as the cost data available and the complex nature of resource use in many cases would make producing accurate estimates difficult.
This study has established that penetrating H&N injuries by assault are increasing in the North East of England. Young adult males are the commonest victims, tending to present in the early hours. Concurrent non-H&N injuries are common. A high proportion requires admission and inpatient surgery. These data confirm these injuries are a significant increasing public health problem requiring substantial hospital resources. In our series, CTAs rarely demonstrated significant vascular injury.
Change history
09 August 2021
A Correction to this paper has been published: https://doi.org/10.1007/s10006-021-00989-1
References
Malik NS, Munoz B, de Courcey C et al (2020) Violence-related knife injuries in a UK city; epidemiology and impact on secondary care resources. E Clin Med 20:100296
Office for National Statistics. Crime In England and Wales: year ending September 2019. Available at - https://www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/bulletins/crimeinenglandandwales/yearendingseptember2019#knife-or-sharp-instrument-offences (accessed Apr 2021)
Smith GA (2013) Knife-related injuries treated in United States Emergency Departments, 1990–2008. J Emerg Med 45:315–323
Meer M, Siddiqi A, Morkel JA et al (2010) Knife inflicted penetrating injuries of the maxillofacial region: A descriptive, record-based study. Injury 41:77–81
Pallett JR, Sutherland E, Glucksman E et al (2014) A cross-sectional study of knife injuries at a London major trauma centre. Ann R Coll Surg Eng 96:23–26
Harris R, Olding C, Lacey C et al (2012) Changing incidence and management of penetrating neck injuries in the South East London trauma centre. Ann R Coll Surg Eng 94:240–244
Olding J, Olding C, Bew D et al (2019) Penetrating head & neck trauma – Epidemiology and injury characteristics in terror-related violence, interpersonal violence and deliberate self-harm at a level 1 trauma centre. Surgeon 17:133–138
Siau RTK, Moore A, Ahmed T et al (2013) Management of penetrating neck injuries at a London trauma centre. Eur Arch OtoRhinoLaryngol 270:2123–2128
Kasbekar AV, Combellack EJ, Derbyshire SG et al (2017) Penetrating neck trauma and the need for surgical exploration: six-year experience within a regional trauma centre. J Laryngol Otol 131:8–12
The English Indices of Deprivation (2019) Ministry of Housing, Communities & Local Government. Available at - https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/835115/IoD2019_Statistical_Release.pdf (Accessed Apr 2021)
ICD-10. International Statistical Classification of Diseases and Related Health Problems. 10th Edition. World Health Organisation. Available at - https://icd.who.int/browse10/2010/en (accessed Apr 2021)
Madsen AS, Laing GL, Bruce JL, Clarke DL (2016) A comparative audit of gunshot wounds and stab wounds to the neck in a South African metropolitan trauma service. Ann R Coll Surg Engl 98:7
Lustenberger T, Talving P, Lam L, Kobayashi L, Inaba K, Plurad D et al (2011) Unstable cervical spine fracture after penetrating neck injury: a rare entity in an analysis of 1,069 patients. J Trauma - Injury Infect Crit Care 70:4
Diaz-Martinez J, Marin JC, Gruezo RP (2019) Review of penetrating neck injuries in 279 patients, analysis of a single institution. J Gen Surg 3:1
Melling L, Lansdale N, Mullassery D, Taylor-Robinson D, Jesudason EC (2012) Penetrating assaults in children: Often non-fatal near-miss events with opportunities for prevention in the UK. Injury 43:12
Kyriacou DN, Hutson HR, Anglin D, Peek-Asa C, Kraus JF (1999) The relationship between socioeconomic factors and gang violence in the city of Los Angeles. In: Journal of Trauma - Injury, Infection and Critical Care 46:2
Christodoulou J, Stokes LR, Bantjes J, Tomlinson M, Stewart J, Rabie S et al (2019) Community context and individual factors associated with arrests among young men in a South African township. PLoS ONE 14:1
Navsaria PH, Nicol AJ, Parry CDH, Matzopoulos R, Maqungo S, Gaudin R (2020) The effect of lockdown on intentional and nonintentional injury during the COVID-19 pandemic in Cape Town, South Africa: a preliminary report. South Afr Med J = Suid-Afrikaanse tydskrif vir geneeskunde 0:0
Abdullahi H, Adamu A, Hasheem M (2020) Penetrating arrow injuries of the head-and-neck region: case series and review of literature. Niger Med J 61:5
Ajayi B, Guthrie H, Trompeter A, Tennent D, Lui DF (2021) The rising burden of penetrating knife injuries. Injury Prevent. Online ahead of print
Vulliamy P, Faulkner M, Kirkwood G, West A, O’Neill B, Griffiths MP et al (2018) Temporal and geographic patterns of stab injuries in young people: a retrospective cohort study from a UK major trauma centre. BMJ Open 8:10
Goodson AMC, Payne KFB, Tahim A, Cabot L, Fan K (2013) Awareness of oral and maxillofacial surgery as a specialty and potential career pathway amongst UK medical undergraduates. Surgeon 11:2
Acknowledgements
The authors would like to thank Mr. Simon Endersby.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Informed consent
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The above article was published online with error. Graph 1 and Figure 1 captions has been interchanged.
Rights and permissions
About this article
Cite this article
Steel, B.J., Swansbury, A. & Wheeler, L.T. A 10-year study of penetrating head and neck injury by assault in the North East of England. Oral Maxillofac Surg 26, 213–222 (2022). https://doi.org/10.1007/s10006-021-00980-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-021-00980-w